Abstract
Objective
With the introduction of third-generation light-emitting diodes (LEDs) in dental practice, it is necessary to compare their bracket-bonding effects, safety, and efficacy with those of the second-generation units.
Methods
In this study, 80 extracted human premolars were randomly divided into eight groups of 10 samples each. Metal or polycrystalline ceramic brackets were bonded on the teeth using second- or third-generation LED light-curing units (LCUs), according to the manufacturers’ instructions. The shear bond strengths were measured using the universal testing machine, and the adhesive remnant index (ARI) was scored by assessing the residual resin on the surfaces of debonded teeth using a scanning electron microscope. In addition, curing times were also measured.
Results
The shear bond strengths in all experimental groups were higher than the acceptable clinical shear bond strengths, regardless of the curing unit used. In both LED LCU groups, all ceramic bracket groups showed significantly higher shear bond strengths than did the metal bracket groups except the plasma emulation group which showed no significant difference. When comparing units within the same bracket type, no differences in shear bond strength were observed between the second- and third-generation unit groups. Additionally, no significant differences were observed among the groups for the ARI.
There have been many developments in dental bonding materials in order to improve the efficiency of the bonding procedure and to assure long-term stability.12 In clinical orthodontics, many studies have sought to simplify the procedure of bracket bonding and reduce chair time, while simultaneously maintaining acceptable bonding strengths.134567
A light-emitting diode (LED) is a light-curing unit (LCU) that emits blue-wavelength light to activate the curing mechanism of resin.89 Due to the demand for shorter resin curing times, a second-generation LED LCU, with comparatively higher power than the conventional LED LCU (first-generation), was developed. Recently, a third-generation LED LCU, which claims to be even more effective with regard to curing time, has come into use. This LCU is believed to improve curing time by generating multiple wavelengths from multiple diodes.5 Rueggeberg5 reported that the third-generation LED LCU can effectively provide enough irradiance at the appropriate wavelengths to polymerize any type of dental restorative material.
Among the available products, the VALO® device (Ultradent Products Inc., South Jordan, UT, USA) has three different light-curing modes―standard power, high power, and plasma emulation―with different recommended curing times. Although the curing time is shortened thanks to the use of multiple diodes, one major negative feature of this third-generation unit is its high power intensity. Flury et al.10 noted that most LCUs utilize LED technology with a single high-powered diode (second-generation), which typically reaches irradiances of 1,200 to 1,500 mW/cm2; however, VALO® shows irradiances of up to 3,200 mW/cm2 when using the plasma curing mode. Spranley et al.11 reported that this VALO® caused curing-light burns to soft tissues, whereupon patients had lip burns after routine restorative treatments, despite their lips being covered by rubber dams. Indeed, patient complaints about the heat during continuous curing procedures is problematic and is a concern for clinicians because of the potential hazard to patients.12 Higher intensity means greater heat generation within the tooth, thus increasing the potential for pulp damage.13 Spranley et al.11 reported soft tissue damage when using a third-generation LED LCU (UltraLume LED 5; Ultradent Products Inc.), and Bruzell Roll et al.12 reported that irradiation of soft tissue should be avoided, as excessive exposure to high-intensity light may cause damage or irritation. Malkoc et al.14 assessed the rise in temperature in the pulp during in vitro orthodontic bonding and found that high-intensity halogen light exceeded the critical 5.5℃ rise in temperature, leading to concerns of increased heat-induced pulpal injury.
Hence, if a clinically acceptable level of light intensity can be achieved with conventional curing units, this high-intensity type of LCU is not needed, particularly considering the risk of possible soft-tissue burning. However, most of the previous studies on these devices compared conventional LCUs with LED LCUs, or only studied second-generation LED LCUs.1516 Studies of third-generation LED LCUs, especially regarding their high-intensity modes, are rare.1217
Therefore, the aim of the present study was to compare the level of light intensity between second- and third-generation LED LCUs in terms of the efficiency of bracket bonding. The shear bond strengths and curing times of second- and third-generation LED LCUs were compared using the reference curing mode recommended by the manufacturers. In addition, the difference between metal and polycrystalline ceramic brackets was also examined. Furthermore, adhesive remnant index (ARI) measurements were performed to determine the debonding effects on the tooth surface and resin remnants.
Institutional review board approval was granted by the committee of Wonkwang University Dental Hospital (number: WKDIRB 201407-02).
In this study, human premolars were extracted from young patients (n = 80; age range, 13–29 years) who visited our clinics for orthodontic treatment (Wonkwang University Dental Hospital, Iksan and Daejeon, Korea). Teeth with caries, restorations, cracks, abnormal anatomic shapes, histories of bleaching and bonding, and iatrogenic cracks made by forceps during extraction were excluded. Teeth were rinsed under running water immediately after extraction, and the soft tissues were subsequently removed using a scaler. After storage in normal saline solution, the teeth were embedded in polyvinylchloride tubes (height, 25 mm; diameter, 30 mm) with hard stone (Figure 1).1819
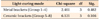
The buccal surface of each tooth was cleaned with non-fluoridated pumice using a rubber prophylactic cup for 10 s and then rinsed with sterile water for 10 s.17 After the teeth were etched with 37% phosphoric acid for 15 s, they were rinsed with sterile water for 15 s and then dried for 5 s using an oil-free air syringe. Bonding primer was applied to the etched surface, and the brackets were bonded with composite resin. Excess composite was gently removed with a scaler before curing. Composite resin was light-cured using either VALO® (Ultradent Products Inc.) or an Ortholux luminous curing light (3M Unitek, Monrovia, CA, USA). All brackets were bonded by one clinician. The same curing mode was used for all applications in order to compare the shear bond strengths of the metal and ceramic brackets. Each sample was stored in 100% relative humidity for 24 h prior to the experiment.1820 Additional details about the materials used in this study are provided in Table 1.
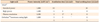
As mentioned above, VALO®, a third-generation LED LCU, and an Ortholux luminous curing unit, a second-generation LED LCU, were used. Various curing modes were applied. VALO® has three different curing modes: (1) standard power, (2) high power, and (3) plasma emulation. The Ortholux luminous curing light does not have multiple curing modes, but the curing time recommended by the manufacturer is different depending on the type of bracket used.
The LCUs were applied perpendicular to the tooth surface, at 1 to 2 mm above the bracket. Each curing mode was applied according to the manufacturer’s instructions. The light intensities of the curing units were measured by a radiometer (Demetron Research Corp., Danbury, CT, USA), and we confirmed that the light intensities were within the range recommended by the manufacturer. The protocols used in this study are displayed in Table 2.
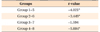
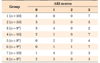
In order to compare the LCUs and brackets, we divided the samples into eight groups of 10 samples each (Table 3).
Shear bond strength was measured using the universal testing machine (Zwick Z020; Zwick GmbH & Co. KG, Ulm, Germany) with a 500-N load cell. The load was measured as a Newton when the bracket debonded from the tooth surface (Figure 1). These measured values were divided by the size of each bracket base (metal bracket, 12.4 mm2; ceramic bracket, 11.54 mm2) and were converted into MPa units.1618
To observe the surfaces and patterns of debonded teeth, each tooth surface was thoroughly inspected using a scanning electron microscope (JSM-6360; JEOL Ltd., Tokyo, Japan). The ARI score was based on the amount of composite resin that remained on the tooth surface (Table 4). Teeth with bracket remnants or fractures were excluded.21
Means and standard deviations were derived from the measured values using PASW Statistics version 17.0 (IBM Co., Armonk, NY, USA). All groups showed normality by the Kolmogorov-Smirnov test and homoscedasticity by the Levene test. To compare the differences among the various light-curing modes within the same type of bracket, a two-way analysis of variance was performed. Student's t-test was also performed to identify differences between the bracket types within the same curing mode. Tukey’s honestly significant difference test was used for multiple cofmparisons. Since the ARI data showed no normality, a Kruskal-Wallis test was performed to compare the light-curing modes within the same bracket type. All statistical analyses were performed at a 0.05 level of significance.
Generally, the shear bond strengths of the metal bracket groups were significantly lower than the bond strengths of the ceramic bracket groups except for when the plasma emulation mode was used (Figure 2).
In the groups where VALO® was used, we found significant differences between the shear bond strengths of the metal and polycrystalline ceramic brackets for all curing modes except the plasma emulation mode.
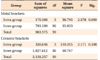
In the groups where the Ortholux luminous curing light was used, the polycrystalline ceramic bracket group showed significantly higher shear bond strengths compared to the metal bracket group (Table 5).
No significant differences were observed among any of the light-curing modes for either bracket type (Table 6).
The ARI scores were based on the images acquired with the scanning electron microscope (Figure 3, Table 7). No significant differences in the ARI scores were identified among the different light-curing modes within the same bracket type (Table 8). In both the metal and ceramic bracket groups, a score of 3 was the most common, while a score of 1 was the second most frequent score in the ceramic bracket groups. There were fractures in six teeth; one in the metal bracket groups and five in the ceramic bracket groups.
First included in the dental armamentarium in 2001, LEDs have been widely used throughout the dental field.9 The advantages of LED LCUs are lamp duration times of up to 10,000 hours, less heat generation, less power consumption, and rechargeable battery power.822 Since there has been a demand for shorter curing times, manufacturers are continuously developing new LED LCUs with increased power intensities,15 as these can reduce both curing time and clinical chair times. The second-generation LED LCU is regarded as a step up from devices that employ multiple discrete LED LCUs to devices that contain more powerful single LED LCUs, which are often specially designed for dental curing applications.13 Currently, LED LCUs with multiple diodes (i.e., third-generation LED LCUs: violet/blue diodes and polywaves) are available, in which the available power intensity is more than 3,500 mW/cm2, depending on the curing mode.1 However, with the possibility of potential hazard to patients from higher intensity of these LED LCU, there has been some doubt as to whether the use of LED LCUs with a high-intensity setting can be justified to shorten chair time. Although it is obvious that third-generation LED LCUs offer not only shorter curing times, but also appropriate bonding strength, it is a serious problem if such devices cause adverse effects. An LED LCU with an appropriate power intensity that could cure resin in a reasonably short time, show adequate bonding strength, and cause no adverse effects would be much more favorable.
According to the manufacturer’s instructions, the recommended curing time for the second-generation LED LCU is 3 s for ceramic brackets and 6 s for metal brackets, which is more efficient than the curing time for first-generation LCUs (20 s). The instructions for VALO® do describe risk prevention tactics; the plasma emulation mode has a 2-s safety delay to limit heating during consecutive curing. If a longer cure is needed, the manufacturer suggests allowing 10 s between consecutive cures or to consider a dual-cure product. Therefore, the overall curing time is shorter when using a second-generation LED LCU than when using a third-generation LED LCU, since the 2-s interval increases the curing time to a total of 8 s. Thus, if the bonding strength of the second-generation LED LCU is appropriate for clinical use, then it will be more suitable than the third-generation unit.
Reynolds23 suggested that a minimum bond strength of 5.9 to 8 MPa is adequate for most clinical orthodontic needs. In this study, the average shear bond strengths were higher than 8 MPa in all of the experimental groups, meaning that the bond strengths are guaranteed not only in the third-generation LED LCU, but also in the second-generation LED LCU (Figure 2).
Moreover, our results showed that the shear bond strengths of the ceramic brackets were higher than the bond strengths of the metal brackets, which is similar to the findings of previous studies.2425 Considering that the ceramic brackets are transparent and direct light transmittance through the bracket,26 this likely explains why this bracket type showed consistently higher bond strengths irrespective of the curing mode, although the differences among the curing modes were not statistically significant.
Higher ARI scores indicate that most of the bonding failures after debonding occur at the bracket-adhesive interface, with the material that remains on the surface preserving the enamel from possible damage.3 However, in the present study, no significant differences in the ARI scores were observed among the groups (Table 8).
Another consideration with regard to shear bond strength is what happens when the bonding strength is too strong, as more force is required to break the bonding, which could lead to tooth fracture. If force greater than 25 to 30 MPa is applied to the longitudinal axis of the enamel prism, then the enamel will fracture. Even when the force is less than 13 MPa, enamel fracture might occur if the force is applied on the curved area of the enamel prism.27 Bishara and Fehr28 reported that it would be advisable to avoid tensile bond strengths greater than 13 MPa. In this study, the average shear bond strengths in both the ceramic and plasma emulation groups, as well as in the standard power groups for the metal brackets, were higher than 13 MPa (Figure 2). According to Reynolds’ suggestion,23 it appears that the bond strengths measured here were acceptable in all curing modes.
In this study, six teeth were fractured in the enamel or in the brackets during the shear bond strength measurements. Among them, five were in the ceramic bracket groups, indicating that the bond strengths of the ceramic brackets were too strong for both LED LCUs. Considering that this study is an in vitro study and that the clinical situation with a complete oral environment is much different, it is hard to fully extrapolate the results of the present study to a clinical setting.
The VALO® device from Ultradent products is a third-generation curing machine, and can emit a wide range of wavelengths from multiple diodes. Resin restorative, with not only camporoquinone but also other materials, can be cured with VALO®. Additionally, the Ortholux luminous curing light from 3M Unitek, with a peak wavelength of 455 nm, closely matches the absorbance peak of camporoquinone. Because matching the wavelength of the curing light to the absorption spectrum of the photoinitiator is the most important factor when curing dental materials, it is essential for clinicians to check that the orthodontic resin material and the LCU are well matched in dental clinics.
This study determined that there were no significant differences in the bond strengths among the various light-curing modes of second- and third-generation LED LCUs within the same bracket group. However, this study did not investigate the thermal effects of LCUs, which indicates the need for additional studies on the effects of LCUs on pulp and soft tissue.
The results of the present study show that the shear bond strengths of all groups were acceptable for clinical use, regardless of the type of curing unit used. The bonding strengths and ARI scores of the second- and third-generation LED LCUs showed no differences when using metal and polycrystalline ceramic brackets in terms of the curing efficiency, although the curing time was shorter for the second-generation LED LCUs.
Figures and Tables
 | Figure 2Graph of the mean and standard deviation of the shear bond strength for each group. See Table 3 for group description. |
 | Figure 3Scanning electron microscope images of the debonding remnant adhesives and teeth. A, Adhesive remnant index (ARI) 0; B, ARI 1; C, ARI 2; D, ARI 3. |
Table 8
Comparison of the adhesive remnant index (ARI) scores between different light-curing modes
df, Degree of freedom; Sig., significance.
By Kruskal-Wallis test; p = 0.05.
See Table 3 for group description.
References
1. Flury S, Lussi A, Hickel R, Ilie N. Light curing through glass ceramics with a second- and a third-generation LED curing unit: effect of curing mode on the degree of conversion of dual-curing resin cements. Clin Oral Investig. 2013; 17:2127–2137.

2. Price RB, Felix CM, Whalen JM. Factors affecting the energy delivered to simulated class I and class v preparations. J Can Dent Assoc. 2010; 76:a94.
3. Dall’Igna CM, Marchioro EM, Spohr AM, Mota EG. Effect of curing time on the bond strength of a bracket-bonding system cured with a light-emitting diode or plasma arc light. Eur J Orthod. 2011; 33:55–59.

4. Swanson T, Dunn WJ, Childers DE, Taloumis LJ. Shear bond strength of orthodontic brackets bonded with light-emitting diode curing units at various polymerization times. Am J Orthod Dentofacial Orthop. 2004; 125:337–341.

6. Lee JH, Lee M, Kim KN, Hwang CJ. Resin bonding of metal brackets to glazed zirconia with a porcelain primer. Korean J Orthod. 2015; 45:299–307.

7. Lee JY, Kim JS, Hwang CJ. Comparison of shear bond strength of orthodontic brackets using various zirconia primers. Korean J Orthod. 2015; 45:164–170.

8. Mills RW, Jandt KD, Ashworth SH. Dental composite depth of cure with halogen and blue light emitting diode technology. Br Dent J. 1999; 186:388–391.

9. Uhl A, Sigusch BW, Jandt KD. Second generation LEDs for the polymerization of oral biomaterials. Dent Mater. 2004; 20:80–87.

10. Flury S, Lussi A, Hickel R, Ilie N. Light curing through glass ceramics: effect of curing mode on micromechanical properties of dual-curing resin cements. Clin Oral Investig. 2014; 18:809–818.

11. Spranley TJ, Winkler M, Dagate J, Oncale D, Strother E. Curing light burns. Gen Dent. 2012; 60:e210–e214.
12. Bruzell Roll EM, Jacobsen N, Hensten-Pettersen A. Health hazards associated with curing light in the dental clinic. Clin Oral Investig. 2004; 8:113–117.

14. Malkoç S, Uysal T, Uşümez S, Işman E, Baysal A. In-vitro assessment of temperature rise in the pulp during orthodontic bonding. Am J Orthod Dentofacial Orthop. 2010; 137:379–383.

15. Cha JY, Lee KJ, Park SH, Kim TW, Yu HS. Comarison of the shear bond strength of brackets in regards to the light curing source. Korean J Orthod. 2006; 36:198–206.
16. Mavropoulos A, Cattani-Lorente M, Krejci I, Staudt CB. Kinetics of light-cure bracket bonding: power density vs exposure duration. Am J Orthod Dentofacial Orthop. 2008; 134:543–547.

17. Kang J, Jun S, Kim J, Kim J, Yoo S. Evaluation of new LED curing light on resin composite polymerization. J Korean Acad Pediatr Dent. 2014; 41:152–156.

18. Kwon TH, Kang JM, Chang NY, Kang KH. Shear bond strength of ceramic brackets bonded with antimicrobial monomer-containing self-etching primer. Korean J Orthod. 2011; 41:16–24.

19. Judy RH, Dunn WJ, Patel AB, Swanson T. Effective single-charge end point of cordless light-emitting diode light-curing units. Am J Orthod Dentofacial Orthop. 2006; 130:378–384.

20. International Organization for Standardization. ISO/TS 11405: 2003(E). Dentistry: Dental materials: testing of adhesion to tooth structure. Geneva, Switzerland: World Health Organization;2003.
21. Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984; 85:333–340.

22. Wiggins KM, Hartung M, Althoff O, Wastian C, Mitra SB. Curing performance of a new-generation light-emitting diode dental curing unit. J Am Dent Assoc. 2004; 135:1471–1479.

24. Eslamian L, Borzabadi-Farahani A, Mousavi N, Ghasemi A. A comparative study of shear bond strength between metal and ceramic brackets and artificially aged composite restorations using different surface treatments. Eur J Orthod. 2012; 34:610–617.

25. Reddy YG, Sharma R, Singh A, Agrawal V, Agrawal V, Chaturvedi S. The shear bond strengths of metal and ceramic brackets: An in-vitro comparative study. J Clin Diagn Res. 2013; 7:1495–1497.

26. Eliades T, Johnston WM, Eliades G. Direct light transmittance through ceramic brackets. Am J Orthod Dentofacial Orthop. 1995; 107:11–19.

27. Graber TM, Eliades T, Athanasiou AE. Risk management in orthodontics: Experts’ guide to malpractice. Surrey, UK: Quintessence Books;2004. p. 25.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download