1. Mitchell L, Carter NE, Doubleday B. An introduction to orthodontics. 2nd ed. New York, NY: Oxford University Press;2001.
2. Graber LW, Vanarsdall RL, Vig KWL. Orthodontics: Current principles and techniques. Philadelphia, PA: Elsevier Mosby;2012.
3. Timms DJ. The dawn of rapid maxillary expansion. Angle Orthod. 1999; 69:247–250. PMID:
10371430.
4. Bishara SE, Staley RN. Maxillary expansion: clinical implications. Am J Orthod Dentofacial Orthop. 1987; 91:3–14. PMID:
3541577.

5. Lagravere MO, Major PW, Flores-Mir C. Long-term skeletal changes with rapid maxillary expansion: a systematic review. Angle Orthod. 2005; 75:1046–1052. PMID:
16448254.
6. Proffit WR, Sarver DM, Fields HW. Contemporary orthodontics. St. Louis, Mo: Mosby Elsevier;2007.
7. Suri L, Taneja P. Surgically assisted rapid palatal expansion: a literature review. Am J Orthod Dentofacial Orthop. 2008; 133:290–302. PMID:
18249297.

8. Betts NJ, Vanarsdall RL, Barber HD, Higgins-Barber K, Fonseca RJ. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 1995; 10:75–96. PMID:
9082002.
9. Malkoc S, Sari Z, Usumez S, Koyuturk AE. The effect of head rotation on cephalometric radiographs. Eur J Orthod. 2005; 27:315–321. PMID:
15947234.

10. Leonardi R, Annunziata A, Caltabiano M. Landmark identification error in posteroanterior cephalometric radiography. A systematic review. Angle Orthod. 2008; 78:761–765. PMID:
18302479.
11. Major PW, Johnson DE, Hesse KL, Glover KE. Landmark identification error in posterior anterior cephalometrics. Angle Orthod. 1994; 64:447–454. PMID:
7864466.
12. Nur M, Kayipmaz S, Bayram M, Celikoglu M, Kilkis D, Sezgin OS. Conventional frontal radiographs compared with frontal radiographs obtained from cone beam computed tomography. Angle Orthod. 2012; 82:579–584. PMID:
21999214.

13. Palomo JM, Valiathan M, Hans MGJ. 3D orthodontic diagnosis and treatment planning. In : Kapila SD, editor. Cone beam computed tomography in orthodontics : Indications, insights, and innovations. Ames, IA: John Wiley & Sons Inc.;2014. p. 221.
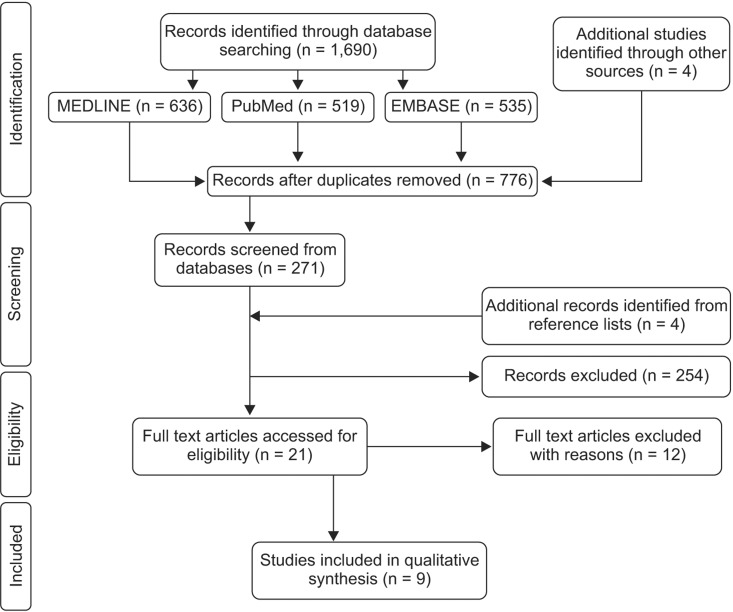
14. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009; 3:e123–e130. PMID:
21603045.

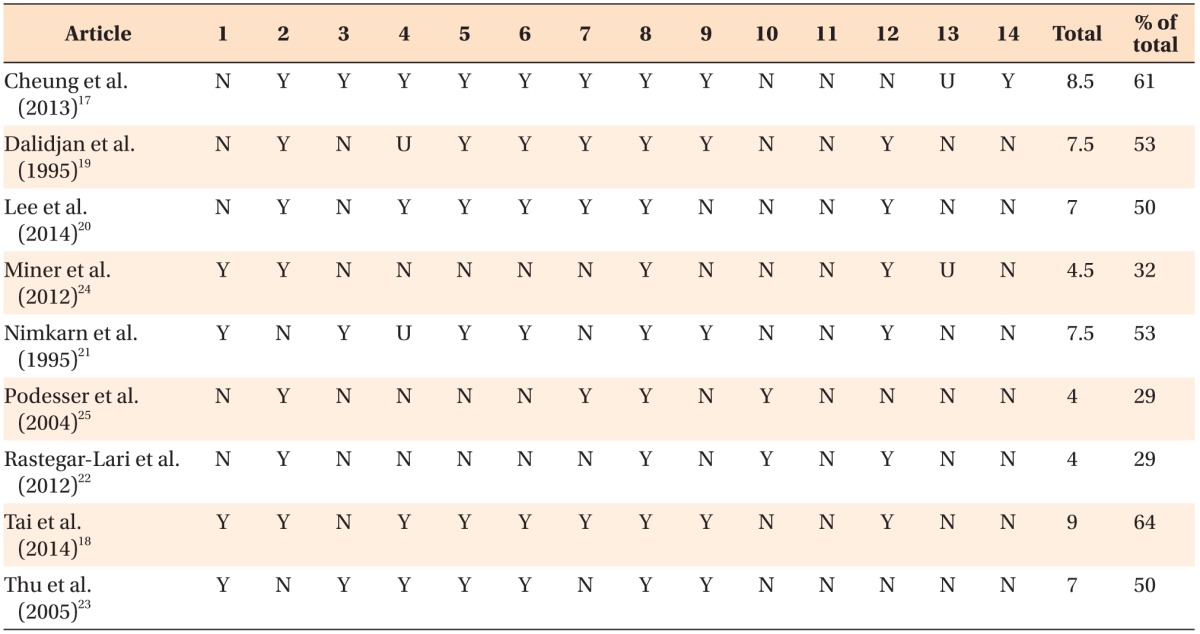
16. Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003; 3:25. PMID:
14606960.

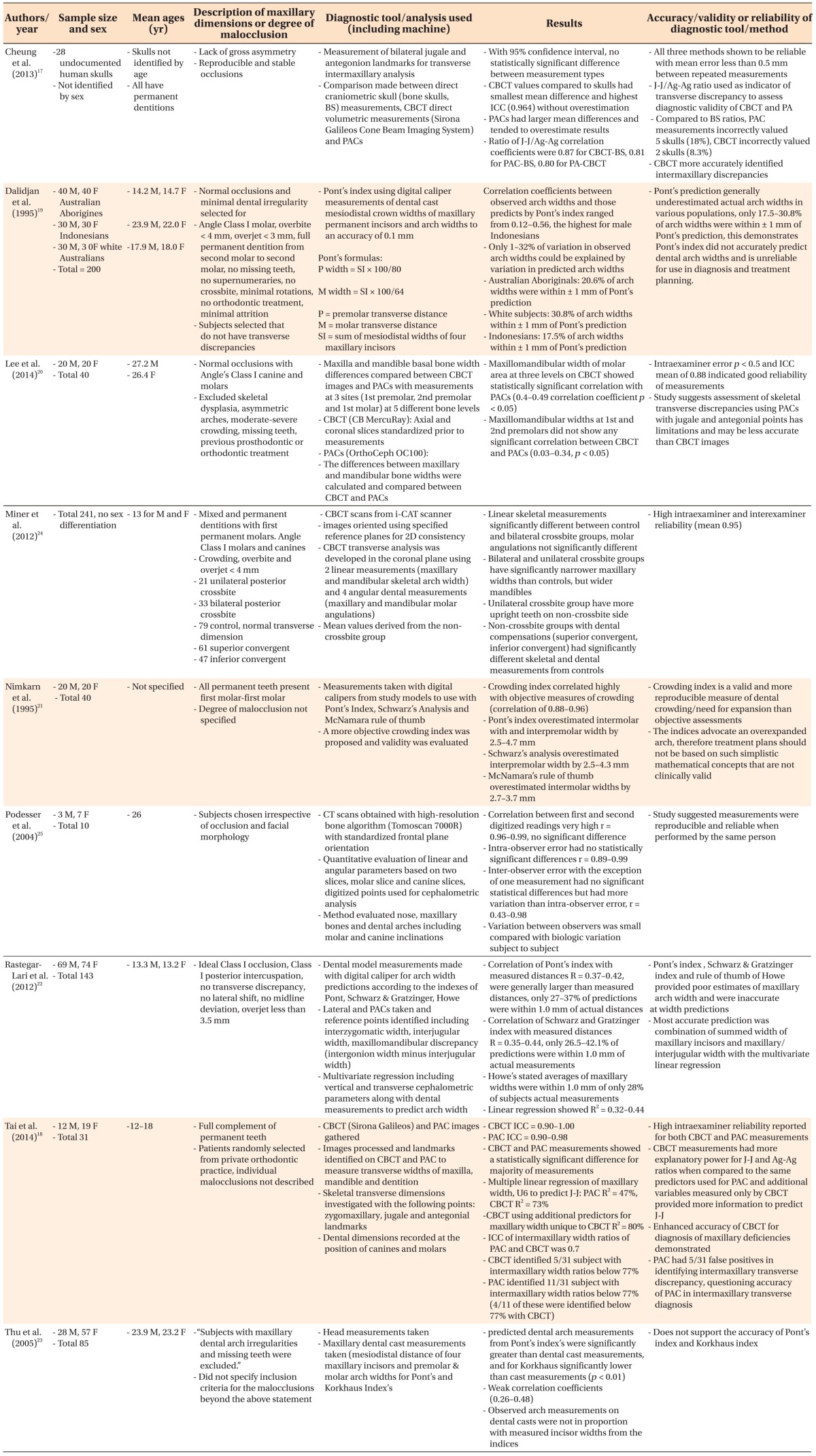
17. Cheung G, Goonewardene MS, Islam SM, Murray K, Koong B. The validity of transverse intermaxillary analysis by traditional PA cephalometry compared with cone-beam computed tomography. Aust Orthod J. 2013; 29:86–95. PMID:
23785942.
18. Tai B, Goonewardene MS, Murray K, Koong B, Islam SM. The reliability of using postero-anterior cephalometry and cone-beam CT to determine transverse dimensions in clinical practice. Aust Orthod J. 2014; 30:132–142. PMID:
25549515.
19. Dalidjan M, Sampson W, Townsend G. Prediction of dental arch development: an assessment of Pont's Index in three human populations. Am J Orthod Dentofacial Orthop. 1995; 107:465–475. PMID:
7733055.

20. Lee KM, Hwang HS, Cho JH. Comparison of transverse analysis between posteroanterior cephalogram and cone-beam computed tomography. Angle Orthod. 2014; 84:715–719. PMID:
24325622.

21. Nimkarn Y, Miles PG, O'Reilly MT, Weyant RJ. The validity of maxillary expansion indices. Angle Orthod. 1995; 65:321–326. PMID:
8526290.
22. Rastegar-Lari T, Al-Azemi R, Thalib L, Årtun J. Dental arch dimensions of adolescent Kuwaitis with untreated ideal occlusion: variation and validity of proposed expansion indexes. Am J Orthod Dentofacial Orthop. 2012; 142:635–644. PMID:
23116504.
23. Thu KM, Winn T, Abdullah N, Jayasinghe JA, Chandima GL. The maxillary arch and its relationship to cephalometric landmarks of selected malay ethnic group. Malays J Med Sci. 2005; 12:29–38. PMID:
22605945.
24. Miner RM, Al Qabandi S, Rigali PH, Will LA. Conebeam computed tomography transverse analysis. Part I: Normative data. Am J Orthod Dentofacial Orthop. 2012; 142:300–307. PMID:
22920695.

25. Podesser B, Williams S, Bantleon HP, Imhof H. Quantitation of transverse maxillary dimensions using computed tomography: a methodological and reproducibility study. Eur J Orthod. 2004; 26:209–215. PMID:
15130045.

26. Vanarsdall RL Jr. Transverse dimension and long-term stability. Semin Orthod. 1999; 5:171–180. PMID:
10860069.

27. de Oliveira MA Jr, Pereira MD, Hino CT, Campaner AB, Scanavini MA, Ferreira LM. Prediction of transverse maxillary dimension using orthodontic models. J Craniofac Surg. 2008; 19:1465–1471. PMID:
19098534.

28. Betts NJ, Lisenby WC. Normal adult transverse jaw values obtained using standardized posteroanterior cephalometrics. J Dent Res. 1994; 73:298. abstr.
29. Crosby DR, Jacobs JD, Bell WH. Special adjunctive considerations 1. transverse (horizontal) maxillary deficiency. In : Bell WH, editor. Modern practice in orthognathic and reconstructive surgery. 3th ed. Philadelphia, PA: Saunders;1992. p. 2403–2430.
30. Alvaran N, Roldan SI, Buschang PH. Maxillary and mandibular arch widths of Colombians. Am J Orthod Dentofacial Orthop. 2009; 135:649–656. PMID:
19409348.

31. Pont A. Der zahn-index in der orthodontie. Zeitschrifi fur Zahnärztliche Orthopaedie. 1909; 3:306–321.
32. Schwarz AM, Gratzinger M. Removable orthodontic appliances. Philadelphia, PA: Saunders;1966. p. 64.
33. Howe RP, McNamara JA Jr, O'Connor KA. An examination of dental crowding and its relationship to tooth size and arch dimension. Am J Orthod. 1983; 83:363–373. PMID:
6573844.

34. Ricketts RM, Roth RH, Chaconas SJ, Schulhof RJ, Engel GA. Orthodontic diagnosis and planning. Denver, CO: Rocky Mountain Data Systems;1982.
35. Major PW, Johnson DE, Hesse KL, Glover KE. Effect of head orientation on posterior anterior cephalometric landmark identification. Angle Orthod. 1996; 66:51–60. PMID:
8678346.
36. Thurow RC. Cephalometric methods in research and private practice. Angle Orthod. 1951; 21:104–116. PMID:
14857377.
37. Lagravère MO, Carey J, Toogood RW, Major PW. Three-dimensional accuracy of measurements made with software on cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2008; 134:112–116. PMID:
18617110.

38. Hans MG, Valiathan M, Palomo JM. Cone beam computed tomography: A link with the past, a promise for the future. Semin Orthod. 2011; 17:81–87.

39. Lascala CA, Panella J, Marques MM. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom). Dentomaxillofac Radiol. 2004; 33:291–294. PMID:
15585804.

40. Cardoso JR, Pereira LM, Iversen MD, Ramos AL. What is gold standard and what is ground truth? Dental Press J Orthod. 2014; 19:27–30. PMID:
25715714.

41. Pretty IA, Maupomé G. A closer look at diagnosis in clinical dental practice: part 1. Reliability, validity, specificity and sensitivity of diagnostic procedures. J Can Dent Assoc. 2004; 70:251–255. PMID:
15120020.
42. Streit LM. CWRU's transverse analysis developing norms [master's thesis]. Cleveland, OH: Case Western Reserve University;2012.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download