Abstract
Objective
Methods
Results
Conclusions
Figures and Tables
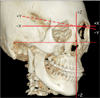
 | Figure 1Superimposition of three-dimensional cone-beam computed tomography images with the cranial base structures by using the OnDemand3D software (CyberMed Inc., Seoul, Korea). The boxes indicate the areas of superimposition. A, Axial view; B, sagittal view; C, coronal view. |
 | Figure 2Coordinate system and zero point (Nasion). X-axis: (+) left, (−) right; Y-axis: (+) posterior, (−) anterior; Z-axis: (+) superior, (−) inferior. |
 | Figure 3Hard-tissue landmarks. The description of the landmarks is shown in Table 2. |
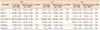
Table 3
Subject characteristics before surgery (T0)
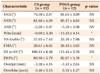
Values are presented as mean ± standard deviation.
CS, Conventional surgery; POGS, preorthodontic orthognathic surgery; SNA, sella-nasion-A point angle; SNB, sella-nasion-B point angle; ANB, A point-nasion-B point angle; Wits, Wits appraisal; SN-GoMe, mandibular plane angle to the anterior cranial base; FMA, mandibular plane angle to the Frankfort plane; U1-SN, upper incisor angle to the anterior cranial base; IMPA, lower incisor angle to the mandibular plane.
NS, Not significant as determined using the Mann-Whitney U test; *p < 0.05; †p < 0.01.
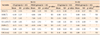
Table 4
Comparison of the extent of surgical movements of the maxilla and mandible (T0–T1)
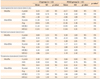
CS, Conventional surgery; POGS, preorthodontic orthognathic surgery; SD, standard deviation; NS, not significant; ANS, anterior nasal spine; PNS, posterior nasal spine; Pog, pogonion; Mf, mental foramen; Rt, right; Lt, left.
*p < 0.05; †p < 0.01; ‡p < 0.001; using the Wilcoxon signed-rank test.
§Using the Mann-Whitney U test.
Table 5
Comparison of the extent of postsurgical changes in the maxilla and mandible (T1–T2)
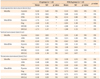
CS, Conventional surgery; POGS, preorthodontic orthognathic surgery; SD, standard deviation; NS, not significant; ANS, anterior nasal spine; PNS, posterior nasal spine; Pog, pogonion; Mf, mental foramen; Rt, right; Lt, left.
*p < 0.01; †p < 0.001; using the Wilcoxon signed-rank test.
‡p < 0.05; §p < 0.01; using the Mann-Whitney U test.
Table 6
Cephalometric variables at each stage
Values are presented as mean ± standard deviation.
CS, Conventional surgery; POGS, preorthodontic orthognathic surgery; SNA, sella-nasion-A point angle; SNB, sella-nasion-B point angle; ANB, A point-nasion-B point angle; U1-SN, upper incisor angle to the anterior cranial base; IMPA, lower incisor angle to the mandibular plane; OJ, overjet; OB, overbite; NS, not significant.
NS, not significant as determined using the Mann-Whitney U test; *p < 0.05; †p < 0.01; ‡p < 0.001.
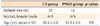
Table 7
Comparison of the changes in skeletal and dental variables during the postsurgical period (T1-T2)
CS, Conventional surgery; POGS, preorthodontic orthognathic surgery; SD, standard deviation; SNA, sella-nasion-A point angle; SNB, sella-nasion-B point angle; ANB, A point-nasion-B point angle; U1-SN, upper incisor angle to the anterior cranial base; IMPA, lower incisor angle to the mandibular plane; OJ, overjet; OB, overbite; NS, not significant.
*p < 0.05; †p < 0.01; ‡p < 0.001; using the Wilcoxon signed-rank test.
§p < 0.01; using the Mann-Whitney U test.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download