Abstract
Objective
The purpose of this study was to evaluate treatment effects after distalization of the mandibular dentition using ramal plates through lateral cephalograms.
Methods
Pre- and post-treatment lateral cephalograms and dental casts of 22 adult patients (11 males and 11 females; mean age, 23.9 ± 5.52 years) who received ramal plates for mandibular molar distalization were analyzed. The treatment effects and amount of distalization of the mandibular molars were calculated and tested for statistical significance. The significance level was set at p < 0.001.
Results
The mandibular first molar distalization
at the crown and root were 2.10 mm (p < 0.001) and 0.81 mm (p = 0.011), respectively. In the evaluation of skeletal variables, there was a significant increase in the Wits appraisal (p < 0.001). In the evaluation of the soft tissue, there was no significant effect on upper lip position, but the lower lips showed a significant retraction of 2.2 mm (p < 0.001).
Conclusions
The mandibular molars showed a significant amount of distalization accompanied by limited extrusion and mesiobuccal rotation of the crowns. A ramal plate may be a viable device for mandibular total arch distalization in Class III patients who are reluctant to undergo orthognathic surgery.
The achievement of a pleasing profile with nonsurgical treatment of Class III patients has always been challenging. Several modalities have been applied for Class III camouflage treatment.123
Several intraoral appliances have been introduced for mandibular molar distalization,45 but unfortunately, most require patient compliance. Non-compliance appliances, such as a distal extension lingual arch, Jones jig, or Franzulum appliance, usually produce tipping, anchorage loss, and flaring of the anterior teeth.678
Temporary skeletal anchorage devices (TSADs) have been applied to overcome these drawbacks in molar distalization.910 However, the placement of miniscrews between the interradicular spaces can result in interference with the distalization process, and the miniscrews might require relocation during distalization. To avoid this disadvantage, Poletti et al.11 installed a miniscrew in the retromolar region for distalization of the lower dentition. However, the placement of a single miniscrew on each side might not be sufficient to withstand the forces required for total arch distalization. Therefore, Sugawara et al.1213 placed a skeletal anchorage system behind the second molar at the mandibular body and evaluated the treatment effects of this appliance.
Recently, Kook et al.14 have reported the application of a plate placed at the retromolar fossa of the ramus for mandibular dentition distalization. This appliance might have a force vector more parallel to the occlusal plane, and is exposed through the retromolar region, which should cause less irritation than buccal miniscrews that are exposed through the movable vestibular mucosa and buccal cheek. However, the treatment effects of a ramal plate have not been evaluated.
The purpose of this study was to evaluate the treatment effects after distalization of the mandibular dentition using a ramal plate through lateral cephalograms and three-dimensional (3D) virtual models.
The sample consisted of pre- and post-treatment lateral cephalograms of 22 adult patients (11 males and 11 females; mean age, 23.9 ± 5.52 years) who had received ramal plates for mandibular molar distalization in the Department of Orthodontics, Seoul St. Mary's Hospital, The Catholic University of Korea. The sample size required to detect a difference of at least 1.5 units with a standard deviation of 2 units using a power of 0.8 and a probability of type I error (α) = 0.05 was 16 patients. Approval was obtained from the institutional review board of the Catholic University of Korea (KC14RISE0483) and informed consent was obtained from all subjects according to the Declaration of Helsinki. The inclusion criteria were (1) patients older than 18 years at the start of treatment, (2) with dental Class III malocclusion with more than a one-half cusp discrepancy at the molars, (3) missing or extracted third molars, and (4) no syndrome or systemic disease.
The ramal plates were placed in the retromolar fossa between the anterior border of the mandibular ramus and the temporal crest. After a mucoperiosteal flap opening was created in the retromolar area, an L-plate (Le Forte system; Jeil Medical Corp., Seoul, Korea) was adapted to fit the bone surface. The hook on the plate was located 3 mm lateral to the buccal surface of the second molar, and between the buccal groove and 3 mm anterior to the distal surface anteroposteriorly (Figure 1). The third molars were extracted during plate installation.
Each plate was fixated with two miniscrews 5 mm in length (with pilot drilling). The flap was sutured over the plate and the hook was extended through the mucosa. The anterior screw hole of the plate was cut occlusally to convert it into a hook for easier placement of elastics or nickel-titanium closed-coil springs. The elastics or closed-coil springs were connected to hooks that were crimped to the archwire between the lateral incisors and canines after placement of the plate.
The hooks were adjusted to be in line with the facial axis points of the mandibular dentition so that the traction forces were parallel to the occlusal plane. Power chain elastics were connected from the plate hooks to the first molar bracket hooks to deliver a force of 300 g per side and were replaced every 3 weeks.
The plates were placed after the leveling and alignment of the mandibular dental arch was completed. The distalization started with a 0.019 × 0.025 inch stainless steel archwire that was fully engaged, and ended when an acceptable overjet was achieved.
Figure 2 demonstrates the lateral cephalometric records of one of the cases at baseline, after leveling and alignment, and at post-treatment.
Pre- and post-treatment lateral cephalograms were digitized. For bilateral landmarks, the midpoint between the right and left superimposed landmarks was selected. For the evaluation of the total treatment effect, the Frankfort horizontal (FH) line and a perpendicular line (VFH) at the pterygoid point were established as the horizontal and vertical reference lines, respectively. To evaluate the amount of distalization, the mandibular plane (MP) and a perpendicular line (VMP) at the menton were used as the horizontal and vertical reference lines, respectively. The distal surface point of the molar crown and the incisal edge of the incisor were used to identify the crowns. The apex and distal root apex were used to identify the incisor and molar root, respectively. Thirty-one linear and angular cephalometric variables were calculated (Figure 3, 4).
The cephalometric digitization of eight randomly selected cases was repeated 2 weeks later by the same examiner. The intraclass correlation coefficient (ICC) was applied to evaluate intra-examiner reliability. The ICC for all variables ranged between 0.961 and 0.912.
Statistical evaluation was performed using SPSS software ver. 16.0 (SPSS Inc., Chicago, IL, USA). The Shapiro-Wilk test was used to assess the normality of the distributions. The paired-sample t-test was applied to evaluate differences between pre- and post-treatment variables, since all these variables were normally distributed. The significance level was set at p < 0.05. The Bonferroni correction was applied to compensate for multiple comparisons, resulting in a significance level of p < 0.001.
In the evaluation of tooth movement in relation to the FH and VFH as the craniofacial reference lines, there was a significant 3.2 mm (p < 0.001) distalization of the mandibular first molars, while their roots were distalized 2.0 mm with distal tipping of 4.6° (p < 0.001). The incisors showed a significant retraction of 4.2 mm (p < 0.001) with a lingual inclination of 10.5° (p < 0.001). The first molar crowns showed no significant change in vertical position (Table 1).
With respect to the mandibular reference lines, the distalization of the first molars was 2.1 mm (p < 0.001), while their roots were distalized 0.8 mm (p = 0.011). The amount of distal tipping was not statistically significant (1.45° ± 4.72°; p = 0.166). The incisors showed a significant retraction of 4.2 mm (p < 0.001) with a significant lingual inclination of 11.2° (p < 0.001). The first molar showed 0.77 mm of intrusion, while the incisor demonstrated 0.93 mm of extrusion (Table 1).
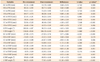
In the evaluation of skeletal variables, there was a significant change in the sagittal relationship between the mandible and maxilla (Wits, 2.4 mm; p < 0.001). However, the A point-nasion-B point (ANB) and sella-nasion-B point (SNB) angles were not changed significantly. Moreover, the MP angle did not increase significantly (Table 2).
In the evaluation of soft tissue, there was no significant effect on upper lip position (nasolabial angle, p = 0.29; true vertical line-upper lip, p = 0.231). However, the lower lip showed a significant retraction of 2.2 mm (p < 0.001). The position of the chin and the ratios between the upper lip and the lower lip and chin showed no significant changes (Table 2).
The treatment of Class III patients with moderate mandibular prognathism has always been complicated. 1516 The distal movement of mandibular molars is considered a challenging treatment objective. However, the application of TSADs to distalize the molars has increased the range of camouflage treatment. It is difficult to distalize more than 2–3 mm with miniscrews because of the interradicular space,171819 but with ramal plates, there is no need to consider relocating the screws.
The ramal plate may have an increased stability and can withstand large forces because it is supported by two miniscrews. For mandibular distalization, usually only one miniscrew is placed per side.1020 Although a buccal shelf mini-implant was successful in distalizing the mandibular arch,20 the force vector resulted in greater rotation of the mandibular occlusal plane. In addition, several studies reported a higher failure rate for miniscrews placed in the mandible compared with those placed in the maxilla.2122
Several studies reported less than 3.5 mm of mandibular arch distalization using miniscrews.232425 Sugawara et al.12 reported distalization of 3.5 mm at the crown level and 1.8 mm at the root level of the first molar combined with a distal tipping ratio of 46.3%. In our study, the amount of distalization was 3.2 mm at the crown level and 2.0 mm at the root level, but with a tipping ratio of 37.5%. This might be due to the difference in the force vectors that resulted from the different placement sites of the two appliances. In addition, different measurement methods might have played a role. Moreover, only patients with Class III malocclusion were included in our study, while in the study by Sugawara et al.,12 patients with Class I and II malocclusion were included to increase their small sample size. Future studies might be recommended to evaluate factors contributing to distal tipping and their effects on the stability of the treatment outcome.
There was a significant change in the sagittal relationship between the mandible and maxilla (Wits, 2.4 mm; p < 0.001), but the ANB and SNB were not changed significantly. This may be due to the fact that the Wits appraisal is measured on the occlusal plane, which might have rotated during treatment.
Since mandibular rotation caused by changes in the vertical positions of the dentition might obscure the actual amount of mandibular molar distalization, two sets of reference lines were used in our study; the FH-VFH and MP-VMP. Although the FH-VFH measurement might mask the exact amount of tooth movement, they were essential to evaluate the total treatment effects, which sum the changes in the mandibular and occlusal planes and tooth movement. In addition, these measurements demonstrate the final relationship of the mandible and mandibular dentition with respect to the cranial base. Meanwhile, measurements from the MP-VMP were used for the assessment of dental changes that occurred as a result of distalization using a ramal plate.
Lateral cephalometric measurements suffer from several drawbacks, such as errors in the identification of landmarks, their projection in two dimensions, the superimposition of anatomical structures, and issues relative to head orientation, which have raised questions about the reliability of these types of analyses.2627 Therefore, it would have been preferable if this study had been conducted with cone-beam computed tomography (CBCT) images. Unfortunately, not all patients included in this study had pre- and post-treatment CBCT records.
It might be important to assess the placement site of the ramal plate thoroughly because of the retromolar foramen, which may exist in 9–25% of the population.282930 Through this foramen, a neurovascular bundle emerges as an extra supply to the pulp tissue and periodontium of the third molar. Other shortcomings are the surgical procedures required for placement and removal of the ramal plate.
Our study included patients with discrepancies of near one-half cusp Class III molar relationships, and this might have resulted in limiting the average distalization. Therefore, a future study including only severe cases might demonstrate the full capability of the ramal plate. In addition, the use of 3D evaluation or 3D-derived cephalograms would decrease the error from superimposition of the right and left sides and would increase the sample size.
In some of our cases, the mandibular incisors showed large amounts of root movement, forcing their apices out of the lingual plate of the symphysis. The vitality and mobility of these teeth were monitored throughout treatment and during the retention period. The retention records showed that the roots became covered by bone again. A future study is recommended to evaluate the effects of total arch distalization on the mandibular anterior teeth and to assess any side effects associated with the treatment.
The relationship between the force vector and the center of the resistance of the mandibular dentition might be an essential factor resulting in minimal distal tipping (4.6°) and vertical changes in the mandibular molars. Future studies are warranted to analyze the biomechanics of the appliance using a finite element analysis. Moreover, studies evaluating the efficiency, effectiveness, and feasibility of the appliance are recommended.
The post-treatment stability of tooth movement has also been an important issue in orthodontics. Previously, there was a common belief that the greater the amount of tooth movement, the more the teeth would be tipped, and that there would be a greater chance of relapse. Sugawara et al.12 stated that the short-term relapse was 0.3 mm for 3.5 mm of distalization. Therefore, it might be important to inform the patient about the possibility of relapse and suggest factors that may decrease its probability. However, the amount of relapse was not investigated in our study, so a future study is needed to evaluate relapse in mandibular molar distalization and the correlation of relapse with respect to the amount of distalization and tipping.
It was possible to achieve efficient total arch distalization using ramal plates. With ramal plates, there was no significant change in the vertical position of the mandibular molars nor in the MP angle; however, the amount of root distalization was not statistically significant. Therefore, the ramal plate can be considered a viable treatment option for mandibular total arch distalization in Class III patients who are reluctant to undergo extraction or orthognathic surgery.
Figures and Tables
Figure 1
The placement site of the ramal plate showing the retromolar fossa. A, The placement site of the ramal plate; B, the ramal plate after adjustment to fit into the retromolar fossa; C, the ramal plate emerging through the attached gingiva; and D, the ramal plate connected to an archwire with a power chain elastic.

Figure 2
Cephalometric radiographs are shown. A, Pretreatment; B, after leveling and alignment; and C, post-treatment.

Figure 3
Cephalometric reference lines and variables. A, Frankfort horizontal (FH) plane; B, perpendicular to the FH at the pterygoid; C, mandibular plane (MP); D, perpendicular to MP at menton.
1, Molar crown to B; 2, molar root to B; 3, molar crown to A; 4, molar root to A; 5, molar long axis–A angle; 6, incisor crown to B; 7, incisor root to B; 8, incisor crown to A; 9, incisor root to A; 10, incisor long axis–A angle; 11, molar crown to D; 12, molar root to D; 13, molar crown to C; 14, molar root to C; 15, molar long axis–C angle; 16, incisor crown to D; 17, incisor root to D; 18, incisor crown to C; 19, incisor root to C; and 20, incisor long axis–C angle.
Figure 4
Cephalometric skeletal and soft-tissue measurements.
1, A point-nasion-B point (ANB); 2, sella-nasion-B point (SNB); 3, Wits; 4, perpendicular to Pog–N; 5, FH to manidibular plane angle (FMA); 6, facial height ratio (posterior facial height 6a/anterior facial height 6b); 7, nasolabial angle; 8, true vertical line-upper lip; 9, true vertical line-lower lip; 10, true vertical line-soft tissue pogonion; 11, stomion inferior-soft tissue menton/subnasale-stomion superior.

Table 2
Comparisons between pre- and post-treatment cephalometric skeletal and soft tissue variables
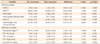
Values are presented as mean ± standard deviation.
ANB, A point-nasion-B point; SNB, sella-nasion-B point; Pog, pogonion; N, nasion; FMA, FH to manidibular plane angle; S, sella; Go, gonion; Na, nasion; Me, menton; TVL, true vertical line; UL, upper lip; LL, lower lip; TVL-Pog', TVL-soft tissue pogonion; Stmi-Me'/Sn-Stms, stomion inferior-soft tissue menton/subnasal-stomion superior.
*Analyzed by paired t-test.
Notes
References
1. Kim YH, Han UK, Lim DD, Serraon ML. Stability of anterior openbite correction with multiloop edgewise archwire therapy: A cephalometric follow-up study. Am J Orthod Dentofacial Orthop. 2000; 118:43–54.

2. Janson G, de Souza JE, Alves Fde A, Andrade P Jr, Nakamura A, de Freitas MR, et al. Extreme dentoalveolar compensation in the treatment of Class III malocclusion. Am J Orthod Dentofacial Orthop. 2005; 128:787–794.

3. Saito I, Yamaki M, Hanada K. Nonsurgical treatment of adult open bite using edgewise appliance combined with high-pull headgear and class III elastics. Angle Orthod. 2005; 75:277–283.
4. Byloff F, Darendeliler MA, Stoff F. Mandibular molar distalization with the Franzulum Appliance. J Clin Orthod. 2000; 34:518–523.
5. Celentano G, Longobardi A, Cannavale R, Perillo L. Mandibular lip bumper for molar torque control. Prog Orthod. 2011; 12:90–92.

6. Kinzinger G, Gross U, Diedrich P. Fixed lingual arch appliance for compliance-free unilateral molar distalization in the mandible. Three case studies. J Orofac Orthop. 2000; 61:440–450.

7. O'Donnell S, Nanda RS, Ghosh J. Perioral forces and dental changes resulting from mandibular lip bumper treatment. Am J Orthod Dentofacial Orthop. 1998; 113:247–255.
8. Muse DS, Fillman MJ, Emmerson WJ, Mitchell RD. Molar and incisor changes with Wilson rapid molar distalization. Am J Orthod Dentofacial Orthop. 1993; 104:556–565.

9. Chung KR, Ahn HW, Kim SJ, Lee KB, Kim SH. Correction of collapsed occlusion with degenerative joint disease focused on the mandibular arch and timely relocation of a miniplate. Am J Orthod Dentofacial Orthop. 2012; 141:e53–e63.

10. Jing Y, Han X, Guo Y, Li J, Bai D. Nonsurgical correction of a Class III malocclusion in an adult by miniscrew-assisted mandibular dentition distalization. Am J Orthod Dentofacial Orthop. 2013; 143:877–887.

11. Poletti L, Silvera AA, Ghislanzoni LT. Dentoalveolar class III treatment using retromolar miniscrew anchorage. Prog Orthod. 2013; 14:7.

12. Sugawara J, Daimaruya T, Umemori M, Nagasaka H, Takahashi I, Kawamura H, et al. Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop. 2004; 125:130–138.

13. Sugawara Y, Kuroda S, Tamamura N, Takano-Yamamoto T. Adult patient with mandibular protrusion and unstable occlusion treated with titanium screw anchorage. Am J Orthod Dentofacial Orthop. 2008; 133:102–111.

14. Kook YA, Park JH, Bayome M, Kim S, Han E, Kim CH. Distalization of the mandibular dentition with a ramal plate for skeletal Class III malocclusion correction. Am J Orthod Dentofacial Orthop. 2016; In press.

15. Ryu HK, Chong HJ, An KY, Kang K. Short-term and long-term treatment outcomes with Class III activator. Korean J Orthod. 2015; 45:226–235.

16. Suh HY, Lee SJ, Park HS. Use of mini-implants to avoid maxillary surgery for Class III mandibular prognathic patient: a long-term post-retention case. Korean J Orthod. 2014; 44:342–349.

17. Park J, Cho HJ. Three-dimensional evaluation of interradicular spaces and cortical bone thickness for the placement and initial stability of microimplants in adults. Am J Orthod Dentofacial Orthop. 2009; 136:314.e1–314.e12.

18. Poggio PM, Incorvati C, Velo S, Carano A. "Safe zones": a guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006; 76:191–197.
19. Ludwig B, Glasl B, Kinzinger GS, Lietz T, Lisson JA. Anatomical guidelines for miniscrew insertion: Vestibular interradicular sites. J Clin Orthod. 2011; 45:165–173.
20. Chang C, Liu SS, Roberts WE. Primary failure rate for 1680 extra-alveolar mandibular buccal shelf mini-screws placed in movable mucosa or attached gingiva. Angle Orthod. 2015; 85:905–910.

21. Chen YJ, Chang HH, Huang CY, Hung HC, Lai EH, Yao CC. A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 2007; 18:768–775.

22. Schätzle M, Männchen R, Zwahlen M, Lang NP. Survival and failure rates of orthodontic temporary anchorage devices: a systematic review. Clin Oral Implants Res. 2009; 20:1351–1359.

23. Park HS, Lee SK, Kwon OW. Group distal movement of teeth using microscrew implant anchorage. Angle Orthod. 2005; 75:602–609.
24. Oh YH, Park HS, Kwon TG. Treatment effects of microimplant-aided sliding mechanics on distal retraction of posterior teeth. Am J Orthod Dentofacial Orthop. 2011; 139:470–481.

25. Ye C, Zhihe Z, Zhao Q, Ye J. Treatment effects of distal movement of lower arch with miniscrews in the retromolar area compared with miniscrews in the posterior area of the maxillary. J Craniofac Surg. 2013; 24:1974–1979.

26. Baumrind S, Frantz RC. The reliability of head film measurements. 1. Landmark identification. Am J Orthod. 1971; 60:111–127.
27. Ahlqvist J, Eliasson S, Welander U. The cephalometric projection. Part II. Principles of image distortion in cephalography. Dentomaxillofac Radiol. 1983; 12:101–108.
28. Bilecenoglu B, Tuncer N. Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg. 2006; 64:1493–1497.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download