Abstract
Objective
To test the null hypothesis that SmartClip self-ligating brackets are more effective than conventional brackets for initial mandibular alignment and identify influential factors.
Methods
Fifty patients were randomly allocated to two equal treatment groups by using an online randomization program: self-ligating group (SmartClip brackets) and conventional group (Gemini brackets). The archwire sequence was standardized. Changes in anterior irregularity index, intercanine width, and intermolar width were assessed on plaster models at 8th and 16th weeks. Changes in incisor position and inclination were assessed on lateral cephalometric radiographs at 16 weeks. Intragroup and intergroup comparisons were performed with paired t-test and Student's t-test, respectively. Multiple linear regression was performed to identify variables affecting improvement in anterior ambiguity.
Results
Data of 46 patients were analyzed; those missing an appointment (n = 2) or showing bracket breakage (n = 2) were excluded. Incisor inclination (p < 0.05), intercanine width (p < 0.05), and intermolar width (p > 0.05) increased at 8 and 16 weeks in both the groups; no significant intergroup differences were noted (p > 0.05). Initial anterior irregularity index and intercanine width change were significantly associated with improvement in anterior irregularity (p < 0.001).
Self-ligating brackets were introduced in orthodontics several decades ago and they experienced resurgence in the last decade with almost all major orthodontic companies offering a self-ligating bracket type.1 Selfligating brackets are popular among clinicians because of reportedly lower resistance to sliding, higher therapeutic efficiency, faster ligation and archwire removal, and shorter chair time,2,3 all of which can reduce overall treatment time.4,5 However, techniques, archwire types and sequences, operator experience, and recall intervals were not controlled in previous studies.6 Further, selfligating brackets are reported to produce less friction than other bracket systems in vitro.7,8,9,10 Because many factors such as archwire dimensions and deflection, bracket slot dimensions and design, interbracket distance, archwire and bracket compositions, saliva, and perturbations can influence the amount of friction in a fixed appliance system,11,12,13 whether self-ligating brackets clinically reduce friction is questionable.
Several prospective randomized clinical trials of selfligating and conventional brackets have been published,1,6,14,15,16,17,18,19,20,21,22,23,24 but only a few focused on initial mandibular alignment with SmartClip self-ligating brackets.6,14,15 Two investigated irregularity changes but not incisor inclination and position or transversal changes.6,15 The third compared relatively long-term (at least 30 weeks) changes in crowding, incisor position and inclination, and intercanine, interpremolar, and intermolar widths.14 Unfortunately, none excluded patients with bracket breakage,6,14,15 which could affect irregularity changes. In addition, other factors that might affect improvement in irregularity have not been completely evaluated.
The aims of this single-center prospective randomized controlled clinical trial were to compare the effectiveness of SmartClip self-ligating and conventional brackets for initial mandibular alignment and identify factors affecting improvement in anterior ambiguity. The null hypothesis was that SmartClip self-ligating brackets are more effective than conventional brackets.
Ethical approval from the local ethics committee (B302KTU0200000/490) and informed consent from the patients and/or their parents were obtained. The sample size was calculated by the Pandis method25: 21 patients were required in each group for 90% power to detect a difference of 2.0 (± 2.3) mm in anterior irregularity index at a significance level of 0.05.
A single operator (M.C.) reviewed the initial data of 80 patients recalled from the orthodontic waiting list of Karadeniz Technical University. The inclusion criteria were as follows: (1) skeletal Class I malocclusion (0° < ANB angle [the angle between Nasion-A point line and Nasion-B point line] < 4° and overjet within 2-4 mm26); (2) permanent dentition; (3) nonextraction treatment of the mandibular arch in patients aged 12-18 years; and (4) over 3-mm irregularity in the mandibular anterior region. Those with previous orthodontic treatment, history of systemic diseases, congenital deformities, current medication, mandibular tooth agenesis, failure to attend one appointment, and bracket breakage were excluded. Finally, 50 patients were enrolled to increase the power and compensate for possible dropouts. These patients were randomly divided into two equal treatment groups by using a randomization program (http://www.randomizer.org/form.htm): self-ligating group (SmartClip brackets; 3M Unitek, Monrovia, CA, USA) and conventional group (Gemini brackets, 3M Unitek).
Bracket bonding, archwire insertion, and orthodontic treatment were performed by two nonblinded experienced operators (M.C. and M.B.) between June and December 2012 at the same clinic. Both types of brackets (0.022-inch slot) were bonded to all the teeth between the mandibular first molars by using Transbond XT (3M Unitek). The archwire sequence was standardized: 0.014-inch round heat-activated nickel-titanium archwire (3M Unitek) for 8 weeks and 0.016-inch round heat-activated nickel-titanium archwire (3M Unitek) up to 16 weeks. The archwire was cut distal to the molar tube without cinching. Intermaxillary elastics, headgear, lingual arch, or coil springs were not used. Conventional brackets were ligated with 0.01-inch stainless steel wire (3M Unitek). The patients were examined at 4-week intervals to ensure intact brackets.
Changes in Little's index,27 intercanine width (distance between the cusp tips), and intermolar width (distance between the central and mesial pits) were assessed in plaster models at 8 and 16 weeks by using a digital caliper (Mitutoyo, Tokyo, Japan). Changes in incisor position and inclination (IMPA [the angle of mandibular incisor to mandibular plane]; I-NB angle, I-NB length [the angle and/or distance of mandibular incisor to Nasion-B point line]) were assessed with NemoCeph NX 2006 software (NemoTec, Madrid, Spain) on lateral cephalometric radiographs taken in a standardized position by an experienced technician. All measurements were performed in random order by one researcher (D.K.) blinded to the patient name and time point.
To examine intraobserver reliability, the same researcher (D.K.) repeated all the measurements 3 weeks after the initial assessment in 15 randomly selected patients and intraclass correlations were calculated. Differences between the readings were tested with paired t-test to estimate systematic error. Intraclass correlation values above 0.931 (0.931-0.967) confirmed the reliability of the measurements. All the measurements were free of systematic error (p > 0.05).
After the Shapiro-Wilk test was performed for determining normality (p > 0.05), paired t-test and Student's t-test were applied for intragroup and intergroup comparisons, respectively. Gender distribution was analyzed by Pearson's chi-square test. Multiple linear regression was performed to identify variables affecting improvement in anterior irregularity: bracket type, chronological age, initial anterior irregularity index, initial intercanine and intermolar widths, initial incisor position and inclination, and mean changes in measured variables at 8 and 16 weeks. All statistical analyses were performed with SPSS software for Windows (version 10.0; SPSS, Inc., Chicago, IL, USA). The significance level was set at p < 0.05 for all the tests.
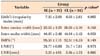
One patient in each group failed to attend an appointment and two patients in the self-ligating group experienced bracket breakage. Therefore, data of 46 patients were analyzed (Figure 1). The self-ligating group consisted of 22 patients (17 male and five female subjects; mean age, 15.48 ± 2.53 years) and the conventional group comprised 24 patients (16 male and eight female subjects; mean age, 14.65 ± 2.02 years). The groups showed no significant differences in gender distribution and chronological age (p > 0.05; Table 1) as well as initial values (p > 0.05; Table 2).
Anterior irregularity index values significantly decreased up to 16 weeks in both the groups (p < 0.01; Table 3). Intercanine width significantly increased at 8 and 16 weeks in the self-ligating (p < 0.05 and p < 0.01, respectively) and conventional (p < 0.05) groups, but intermolar width did not change significantly (p > 0.05). During 16 weeks of alignment, the mandibular incisors were significantly proclined (p < 0.001), but their position did not significantly change in both the groups (p > 0.05). Student's t-test showed no significant intergroup differences in these changes (p > 0.05).
Initial anterior irregularity index and intercanine width changes were significantly associated with improvement in anterior irregularity (p < 0.001). None of the other variables had significant effects (p > 0.05; Table 4).
Previous studies1,6,14,15 showing no differences in the amount of irregularity change in the mandibular arch between self-ligating and conventional brackets did not exclude patients with bracket breakage and failure to attend an appointment. In this study, we excluded such patients and it eliminated the potential effects of bracket breakage on initial alignment in the mandibular arch which was not previously done.
This clinical trial showed no significant difference in mandibular alignment, although slightly better correction (0.9 mm) was achieved in the self-ligating group. The finding is similar to that of Miles,6 who reported 0.7-mm difference in correction between SmartClip self-ligating and conventional brackets. However, the author6 did not investigate potential factors affecting Little's index27 changes. We found that initial anterior irregularity index and intercanine width changes have significant effects on improvement in anterior irregularity during initial alignment. Although the groups did not show significant differences in these variables, the slightly higher anterior irregularity index before the treatment (~0.9 mm) and marginally larger intercanine width (~0.2 mm) in the self-ligating group might be responsible for this result. Fleming et al.15 reported a similar relationship between initial irregularity and irregularity changes due to alignment with SmartClip self-ligating brackets over 8 weeks. They also reported that mandibular alignment is independent of bracket type, supporting our finding.
According to Fleming et al.,14 the ideal alignment procedure would involve slight incisor proclination and intercanine expansion but considerable intermolar expansion, which are important for long-term stability.28 SmartClip self-ligating and conventional brackets did not show significant differences in these parameters in the present study. Contrarily, Fleming et al.14 reported approximately 1-mm greater increase in intermolar width with self-ligating brackets. This difference can be attributed to several factors including alignment and leveling over 30 weeks and use of 0.017 × 0.025-inch and 0.019 × 0.025-inch nickel-titanium and stainless steel rectangular archwires.14 Alignment in the present study was performed for 16 weeks and only round nickel-titanium archwires were used.
Despite the recently reported advantages of self-ligating brackets,29,30 the present and previous prospective randomized clinical studies6,14,15 showed that such brackets do not affect initial mandibular alignment. In addition, Ong et al.19 reported that self-ligating brackets are no more efficient than conventional brackets for anterior alignment or passive extraction space closure in the maxillary arch during the first 20 weeks. Clinicians should therefore consider the cost of these systems and their assumed advantages. SmartClip self-ligating brackets have some notable disadvantages including difficulty of archwire insertion on rotated teeth, disengaging of rectangular archwires,6 and increased discomfort during archwire insertion and removal.16
This study showed relatively short-term outcomes. Therefore, prospective randomized clinical trials of long-term irregularity correction and transversal effects of both bracket types are warranted.
The null hypothesis was rejected. SmartClip self-ligating and conventional brackets have similar effectiveness for initial mandibular alignment. Initial anterior irregularity index and intercanine width change are important predictors of improvement in anterior irregularity during initial mandibular alignment, but bracket type has little effect.
Figures and Tables
Table 3
Comparison of mandibular arch changes

Values are presented as mean ± standard deviation.
SL, Self-ligating group; CL, conventional group; IMPA, the angle of mandibular incisor to mandibular plane; I-NB, the angle and/or distance of mandibular incisor to N-B line (Nasion-B point).
Mean value by paired t-test; p-value by Student's t-test.
*p < 0.05; †p < 0.01; ‡p < 0.001.
Notes
References
1. Pandis N, Polychronopoulou A, Makou M, Eliades T. Mandibular dental arch changes associated with treatment of crowding using self-ligating and conventional brackets. Eur J Orthod. 2010; 32:248–253.

2. Damon DH. The rationale, evolution and clinical application of the self-ligating bracket. Clin Orthod Res. 1998; 1:52–61.

3. Harradine NW, Birnie DJ. The clinical use of Activa self-ligating brackets. Am J Orthod Dentofacial Orthop. 1996; 109:319–328.

4. Eberting JJ, Straja SR, Tuncay OC. Treatment time, outcome, and patient satisfaction comparisons of Damon and conventional brackets. Clin Orthod Res. 2001; 4:228–234.

6. Miles PG. SmartClip versus conventional twin brackets for initial alignment: is there a difference? Aust Orthod J. 2005; 21:123–127.
7. Hain M, Dhopatkar A, Rock P. The effect of ligation method on friction in sliding mechanics. Am J Orthod Dentofacial Orthop. 2003; 123:416–422.

8. Hain M, Dhopatkar A, Rock P. A comparison of different ligation methods on friction. Am J Orthod Dentofacial Orthop. 2006; 130:666–670.

9. Pizzoni L, Ravnholt G, Melsen B. Frictional forces related to self-ligating brackets. Eur J Orthod. 1998; 20:283–291.

10. Henao SP, Kusy RP. Evaluation of the frictional resistance of conventional and self-ligating bracket designs using standardized archwires and dental typodonts. Angle Orthod. 2004; 74:202–211.
11. Frank CA, Nikolai RJ. A comparative study of frictional resistances between orthodontic bracket and arch wire. Am J Orthod. 1980; 78:593–609.

12. Kapila S, Angolkar PV, Duncanson MG Jr, Nanda RS. Evaluation of friction between edgewise stainless steel brackets and orthodontic wires of four alloys. Am J Orthod Dentofacial Orthop. 1990; 98:117–126.

13. Braun S, Bluestein M, Moore BK, Benson G. Friction in perspective. Am J Orthod Dentofacial Orthop. 1999; 115:619–627.

14. Fleming PS, DiBiase AT, Sarri G, Lee RT. Comparison of mandibular arch changes during alignment and leveling with 2 preadjusted edgewise appliances. Am J Orthod Dentofacial Orthop. 2009; 136:340–347.

15. Fleming PS, DiBiase AT, Sarri G, Lee RT. Efficiency of mandibular arch alignment with 2 preadjusted edgewise appliances. Am J Orthod Dentofacial Orthop. 2009; 135:597–602.

16. Fleming PS, Dibiase AT, Sarri G, Lee RT. Pain experience during initial alignment with a selfligating and a conventional fixed orthodontic appliance system. A randomized controlled clinical trial. Angle Orthod. 2009; 79:46–50.

17. Fleming PS, DiBiase AT, Lee RT. Randomized clinical trial of orthodontic treatment efficiency with self-ligating and conventional fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010; 137:738–742.

18. Pandis N, Polychronopoulou A, Katsaros C, Eliades T. Comparative assessment of conventional and self-ligating appliances on the effect of mandibular intermolar distance in adolescent nonextraction patients: a single-center randomized controlled trial. Am J Orthod Dentofacial Orthop. 2011; 140:e99–e105.

19. Ong E, McCallum H, Griffin MP, Ho C. Efficiency of self-ligating vs conventionally ligated brackets during initial alignment. Am J Orthod Dentofacial Orthop. 2010; 138:138.e1–138.e7.

20. Cattaneo PM, Treccani M, Carlsson K, Thorgeirsson T, Myrda A, Cevidanes LH, et al. Transversal maxillary dento-alveolar changes in patients treated with active and passive self-ligating brackets: a randomized clinical trial using CBCT-scans and digital models. Orthod Craniofac Res. 2011; 14:222–233.

21. Wahab RM, Idris H, Yacob H, Ariffin SH. Comparison of self- and conventional-ligating brackets in the alignment stage. Eur J Orthod. 2012; 34:176–181.

22. Bertl MH, Onodera K, Čelar AG. A prospective randomized split-mouth study on pain experience during chairside archwire manipulation in self-ligating and conventional brackets. Angle Orthod. 2013; 83:292–297.

23. Fleming PS, Lee RT, Marinho V, Johal A. Comparison of maxillary arch dimensional changes with passive and active self-ligation and conventional brackets in the permanent dentition: a multicenter, randomized controlled trial. Am J Orthod Dentofacial Orthop. 2013; 144:185–193.

24. Johansson K, Lundström F. Orthodontic treatment efficiency with self-ligating and conventional edgewise twin brackets: a prospective randomized clinical trial. Angle Orthod. 2012; 82:929–934.

25. Pandis N. Sample calculations for comparison of 2 means. Am J Orthod Dentofacial Orthop. 2012; 141:519–521.

26. Celikoglu M, Akpinar S, Yavuz I. The pattern of malocclusion in a sample of orthodontic patients from Turkey. Med Oral Patol Oral Cir Bucal. 2010; 15:e791–e796.

27. Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975; 68:554–563.

28. Burke SP, Silveira AM, Goldsmith LJ, Yancey JM, Van Stewart A, Scarfe WC. A meta-analysis of mandibular intercanine width in treatment and postretention. Angle Orthod. 1998; 68:53–60.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download