Abstract
A 27-year-old man presented an anterior open bite relapse. He had low tongue posture positioned anteriorly at rest and during swallowing and reported chronic difficulty in nose breathing. Head cone-beam computed tomography revealed nasal septum deviation, right turbinate hypertrophy, and left maxillary sinus congestion, which were thought to contribute to the breathing problem, encourage the improper tongue posture, and thereby cause the relapse. Multidisciplinary treatment involving an otorhinolaryngologist, an orthodontist, and a periodontist resolved the upper airway obstruction and corrected the malocclusion. The follow-up examination after 3 years 5 months demonstrated stable results.
One of the most challenging malocclusions to treat and maintain is open bite. Its etiology involves a combination of genetic factors, unfavorable growth pattern, and oral habits. Habitual nonnutritive sucking, altered tongue function and posture, and persistent infantile swallowing, for example, can contribute to vertical malocclusion in the growth period.1,2
Several studies have suggested a relationship among nasopharyngeal airway obstruction, mouth breathing, and skeletal and dental malocclusion. Indeed, adenoid hypertrophy and chronic rhinitis may result in mouth breathing and encourage persistent infantile swallowing, which can contribute to anterior open bite.3,4,5,6
As such habits can cause relapse following orthodontic treatment,7,8 contributing factors should be uncovered when diagnosing patients with anterior open bite. Considering the etiological complexity, a multidisciplinary approach involving several health professionals, such as orthodontists, otorhinolaryngologists, orofacial myofunctional therapists, and maxillofacial surgeons, in adult patients, may be necessary. Here, we report the multidisciplinary correction of anterior open bite relapse secondary to upper airway obstruction.
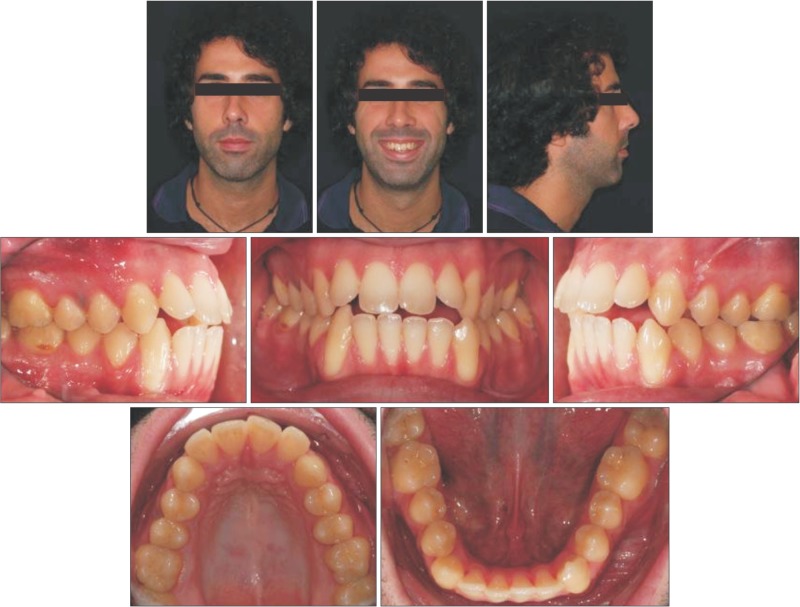
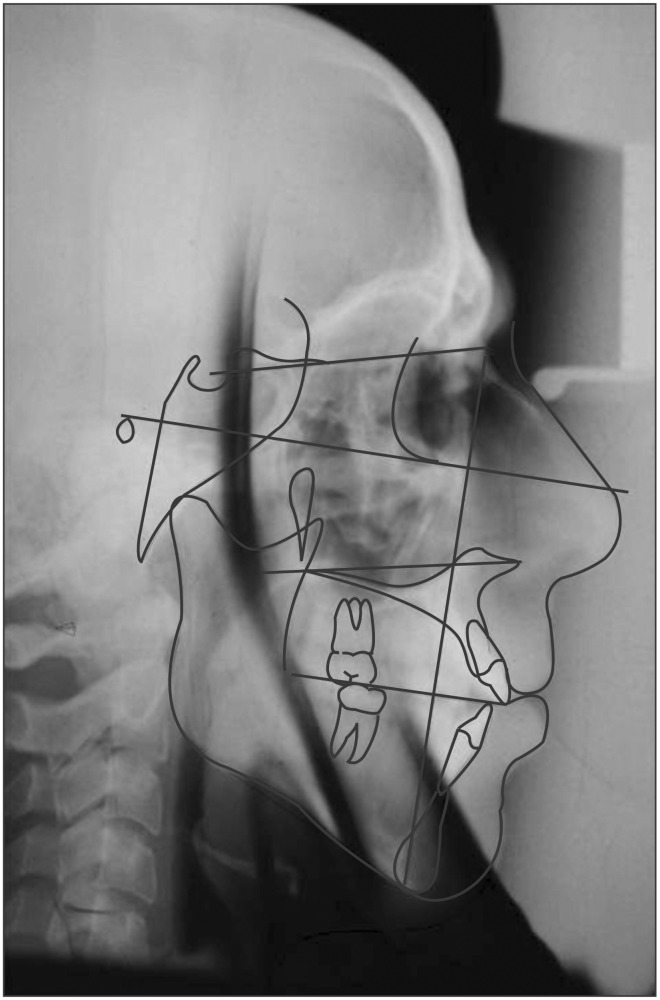
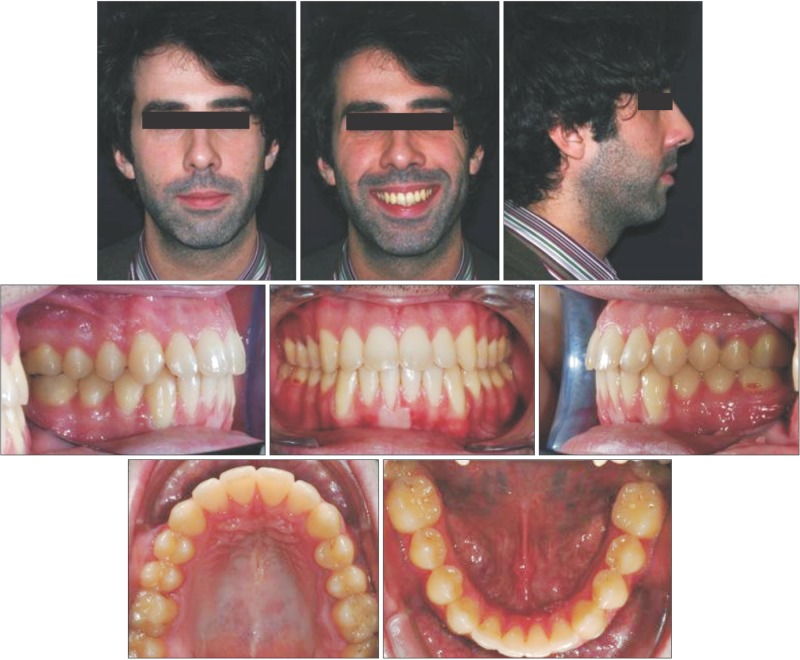
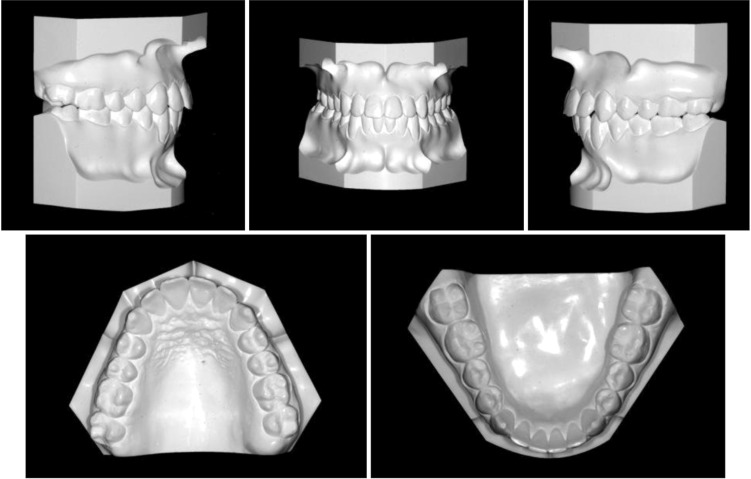
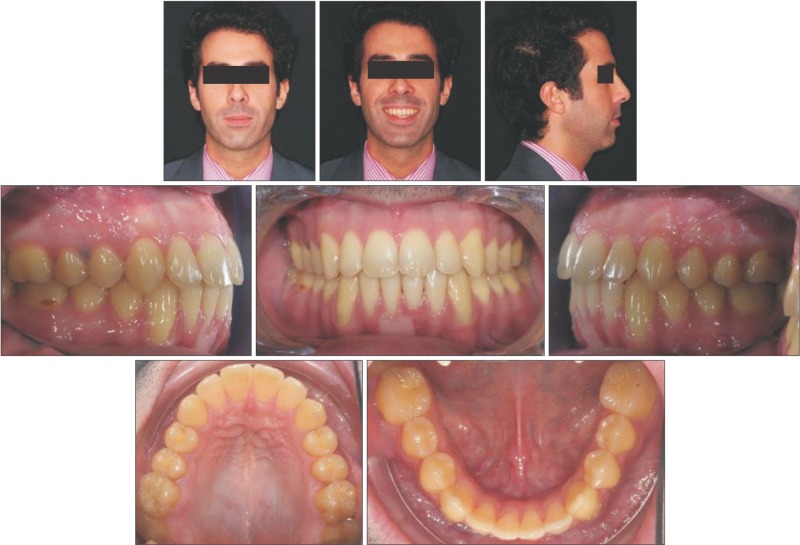
A 27-year-old man presented an anterior open bite relapse (Figures 1,2,3,4). He reported that orthodontic treatment was begun when he was 13 years old and lasted 5 years. Although initially satisfied with the outcome, he noticed relapse of anterior open bite one year after the brackets were removed.
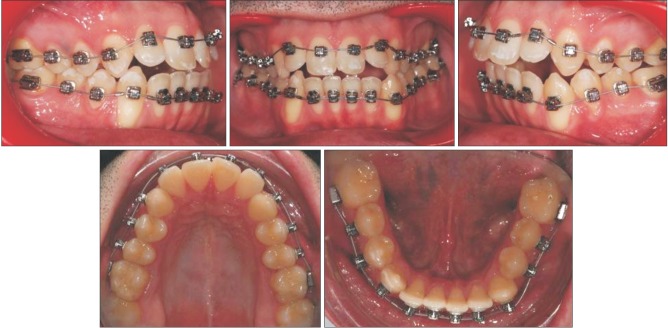
Intraoral examination showed bilateral Angle Class I molar relationship, slight deviation of the upper midline, proclination of the maxillary lateral incisors, crossbite of the maxillary left canine and second premolar, negative crown inclination of the maxillary posterior teeth, and gingival recession at the mandibular canines.
Facial analysis showed increased lower facial height with good lip competence and large nasolabial angle. Slight nasal deviation to the right was also apparent when the patient was viewed anteriorly. Gingival exposure while smiling was confined to the maxillary posterior region. Anterior low tongue posture was noted at rest and during swallowing, and the patient reported chronic difficulty in nose breathing.
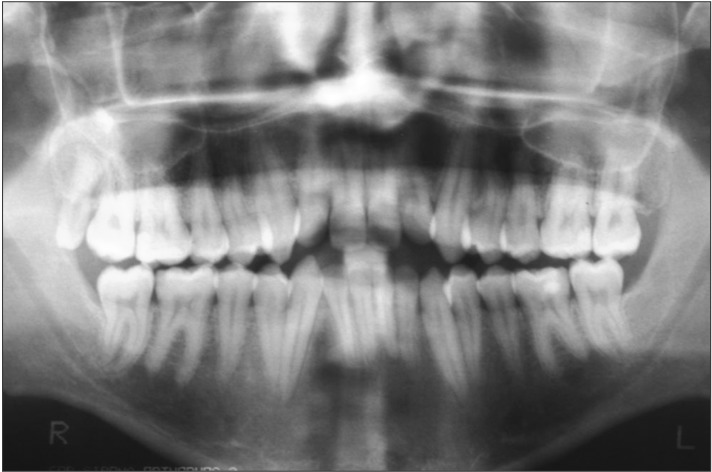
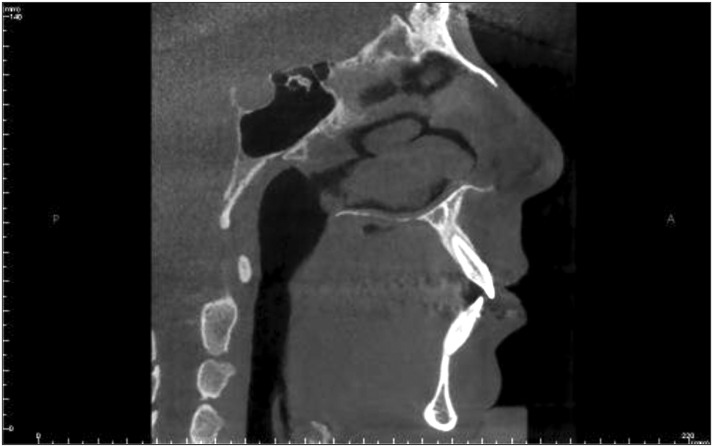
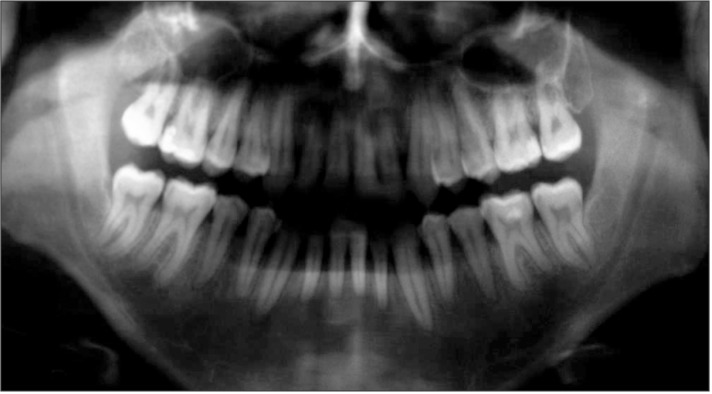
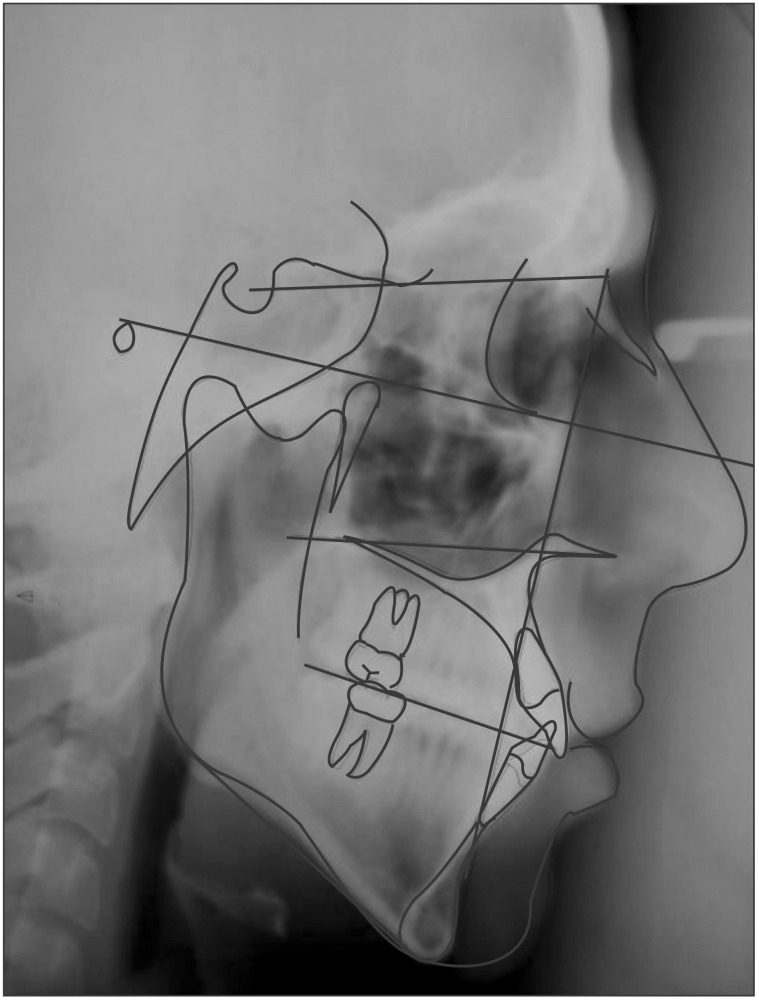
A cone-beam computed tomography (CBCT) of the head was performed to uncover upper airway problems responsible for the breathing difficulty and relapse. The scan showed extremely thin mandibular symphysis, which can markedly affect mandibular incisor inclination during orthodontic treatment (Figure 5). In addition, nasal septum deviation, right turbinate hypertrophy, and left maxillary sinus congestion were visible (Figure 6). All these features were thought to contribute to the breathing problem, encourage the improper tongue posture, and thereby cause the relapse.
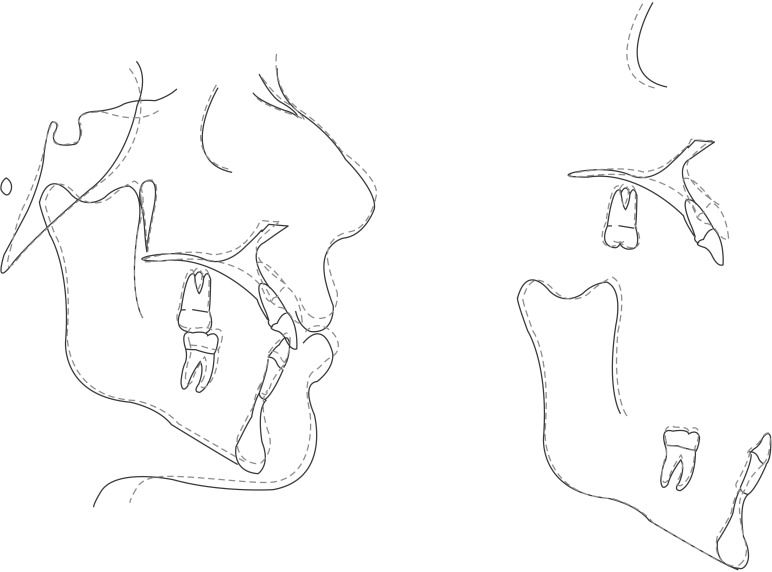
Pretreatment cephalometric analysis confirmed the Class I hyperdivergent skeletal pattern associated with dental anterior open bite and moderate maxillary incisor proclination (Table 1).
The treatment objectives were to (1) maintain the bilateral Angle Class I molar relationship; (2) correct the anterior open bite; (3) balance maxillary gingival exposure, ensuring a pleasant smile; (4) minimize mandibular gingival recession during the treatment; (5) achieve positive crown inclination of the maxillary posterior teeth, creating a wider smile; and (6) ensure stable results overall.
The presence of dental (not skeletal) open bite, lip competence, and good facial and smile esthetics excluded combined orthodontic treatment and orthognathic surgery as well as first premolar extraction. Although use of tongue spurs or a tongue crib during orthodontic treatment can achieve rapid closure of open bite, this approach was rejected because the tongue posture was judged to be secondary to the breathing problem. To meet all the treatment objectives, we offered the patient a multidisciplinary approach involving orthodontic treatment to correct the malocclusion, otorhinolaryngological intervention to resolve the airway obstruction, and periodontal treatment to correct any gingival recession arising in critical mandibular areas during the treatment.
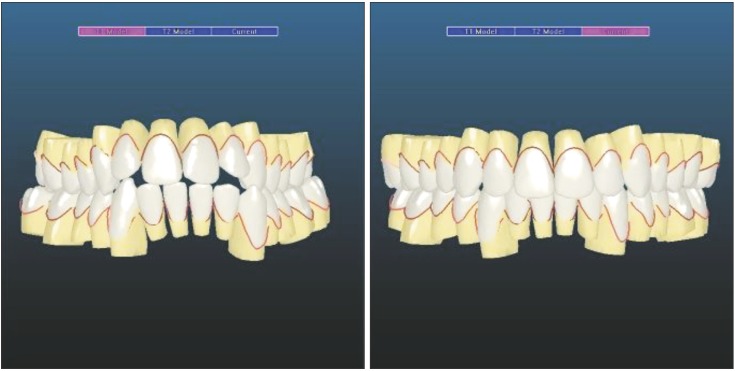
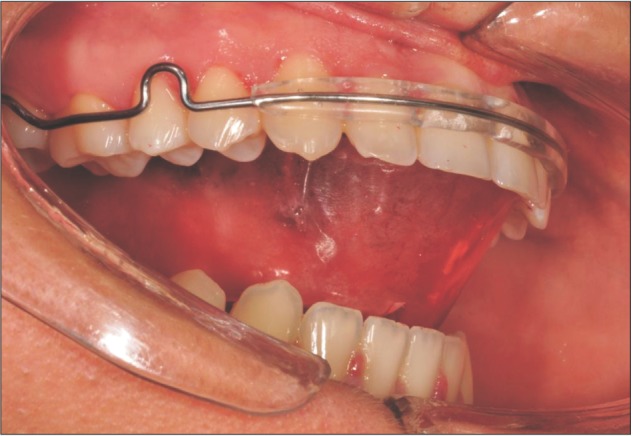
Damon self ligating brackets with Insignia™ (Ormco Co., Orange, CA, USA) were bonded to all the teeth (Figures 7, 8). In the digital setup, we programmed complete correction of the open bite and, because of the susceptibility to relapse, overcorrection of the overbite, placing the maxillary incisal margin 3 mm below the edge of the mandibular incisors. We also programmed positive crown torque of the maxillary posterior teeth and ensured that all the mandibular teeth would be maintained in the middle of the medullary bone to prevent bone dehiscence and fenestrations, which can cause substantial gingival recession.
The brackets were threaded with the following customized archwire sequence: 0.014 inches (in) Damon Copper nickel titanium (Ni-Ti), 0.014 × 0.025 in Damon Copper Ni-Ti, 0.018 × 0.025 in Damon Copper Ni-Ti, 0.019 × 0.025 in stainless steel, and 0.019 × 0.025 in titanium molybdenum alloy (TMA).
Leveling and alignment were performed using thermal Ni-Ti archwires and completed rapidly because of the previous orthodontic treatment and relapse mainly involved the anterior open bite. When the 0.018 × 0.025 in Damon Copper Ni-Ti archwires were fitted, the patient was also supplied with intermaxillary elastics to facilitate bite closure during the remainder of the active phase. Bilateral triangular elastics (3/16 in, 6 oz.) were provided for daytime use, and anterior box elastics (5/16 in, 6 oz.) were added for nocturnal wear.
After 10 months of orthodontic treatment, we referred the patient to an otorhinolaryngologist for bilateral turbinectomy and maxillary sinus cleaning. The surgery was performed by endonasal endoscopy and prompted immediate improvement in the patient's breathing dynamics. The CBCT scan taken 5 months postoperatively showed complete resolution of upper airway obstruction (Figure 9), and at the subsequent orthodontic appointments, the patient reported that he was finally able to breathe through his nose and his sleep quality had improved. At these appointments, we reminded the patient to continue to maintain correct tongue posture at rest and during swallowing.
The orthodontic treatment was concluded at 19 months. The Class I molar and canine relationship was maintained, anterior occlusion was improved, and ideal overbite and overjet was achieved. The treatment brought about mutually protected functional occlusion, with adequate canine disclusion and protrusive guidance. The temporomandibular joints showed no incoordination on opening and closing, and no temporomandibular joint or muscle problems developed during the retention and postretention periods. The facial profile improved, as did the prominence of the upper lip. The lips remained competent, and the smile was balanced and pleasant.
Unfortunately, because of the mandibular anatomy and tooth movement, the existing gingival recession became more pronounced. The periodontist decided to improve the periodontal condition of the right mandibular central incisor alone and delay definitive mucogingival surgery for some years to stabilize the gingival conditions.
The post-treatment panoramic radiograph showed good root parallelism without root resorption. Post-treatment cephalometric evaluation showed acceptable incisor inclination. Superimposition of the pretreatment and post-treatment cephalometric tracings highlighted the amount of extrusion of the maxillary incisors needed to resolve the open bite and confirmed that the mandibular plane angle remained stable (Figures 10,11,12,13,14, Table 1).
The patient was instructed to wear a tongue elevator (Figure 15) for retention at night. This device featured an anterior opening that served as a tactile reminder and a chute that prevented positioning of the tongue between the dental arches. Examination after 3 years 5 months showed stable results. The well-aligned dentition and good overbite were maintained, facial balance was harmonious, and the smile was pleasing with good, stable gingival lines (Figure 16).
The success of the treatment is mainly ascribable to the thorough diagnosis and multidisciplinary approach, resolving not only the relapse but also the underlying issues. Although the previous orthodontic treatment lasted 5 years, it did not guarantee stability of results. We believe that it failed predominantly because it was not aimed at tackling the airway obstruction and consequent tongue malpositioning, which were the root causes of the malocclusion.
There are many options for correcting the tendency to place the tongue too forward (tongue habit management). A tongue crib or tongue spurs can be used during orthodontic treatment to modify tongue posture, maintain stability of treated open bite, and prevent relapse, by establishing a new engram.9,10,11 However, many orthodontists underestimate the importance of upper airway obstruction in oral habits. Anomalies of the nasal septum, turbinates, adenoids, or tonsils and chronic sinusitis can markedly alter respiratory dynamics, compromising dental arch development.4,12,13 Therefore, when poor breathing is suspected, specific investigative tools, such as tomography with a wide field of view, should be used to examine the upper airway. Referral to an otorhinolaryngologist for endoscopic analysis of the airway is also beneficial.
Our patient presented with anterior low tongue posture and reported chronic difficulty in nose breathing, so we examined the airway by digital volumetric tomography. The abnormal findings prompted us to refer the patient to the otorhinolaryngologist. The approach selected was orthodontic closure of the open bite using intermaxillary elastics and midcourse surgical turbinectomy, sinus cleaning, and correction of nasal septum deviation. The surgery had an immediate effect on the patient's respiratory difficulty, enabling him to breathe normally and position the tongue correctly. However, as open bite presents a high risk of relapse,14,15 we prescribed nocturnal use of a tongue elevator for retention. The good results obtained by this multidisciplinary treatment are still preserved over 3 years later.
Dental malocclusion often needs to be treated by a multidisciplinary team to arrive at an accurate diagnosis and offer appropriate solutions. In particular, adults presenting with open bite, especially relapse cases, should be investigated for oral habits and/or airway issues before defining and selecting the best treatment option.
References
1. Subtelny JD, Sakuda M. Open bite: diagnosis and treatment. Am J Orthod. 1964; 50:337–358.
2. Alexander CD. Open bite, dental alveolar protrusion, class I malocclusion: A successful treatment result. Am J Orthod Dentofacial Orthop. 1999; 116:494–500. PMID: 10547506.

3. Oulis CJ, Vadiakas GP, Ekonomides J, Dratsa J. The effect of hypertrophic adenoids and tonsils on the development of posterior crossbite and oral habits. J Clin Pediatr Dent. 1994; 18:197–201. PMID: 8054305.
4. Vig KW. Nasal obstruction and facial growth: the strength of evidence for clinical assumptions. Am J Orthod Dentofacial Orthop. 1998; 113:603–611. PMID: 9637562.

5. Warren DW, Mayo R, Zajac DJ, Rochet AH. Dyspnea following experimentally induced increased nasal airway resistance. Cleft Palate Craniofac J. 1996; 33:231–235. PMID: 8734724.

6. Fujiki T, Inoue M, Miyawaki S, Nagasaki T, Tanimoto K, Takano-Yamamoto T. Relationship between maxillofacial morphology and deglutitive tongue movement in patients with anterior open bite. Am J Orthod Dentofacial Orthop. 2004; 125:160–167. PMID: 14765053.

7. Smithpeter J, Covell D Jr. Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. Am J Orthod Dentofacial Orthop. 2010; 137:605–614. PMID: 20451779.

8. Wriedt S, Buhl V, Al-Nawas B, Wehrbein H. Combined treatment of open bite - long-term evaluation and relapse factors. J Orofac Orthop. 2009; 70:318–326. PMID: 19649579.

9. Giuntini V, Franchi L, Baccetti T, Mucedero M, Cozza P. Dentoskeletal changes associated with fixed and removable appliances with a crib in open-bite patients in the mixed dentition. Am J Orthod Dentofacial Orthop. 2008; 133:77–80. PMID: 18174075.

10. Bosio JA, Justus R. Treatment and retreatment of a patient with a severe anterior open bite. Am J Orthod Dentofacial Orthop. 2013; 144:594–606. PMID: 24075668.
11. Meyer-Marcotty P, Hartmann J, Stellzig-Eisenhauer A. Dentoalveolar open bite treatment with spur appliances. J Orofac Orthop. 2007; 68:510–521. PMID: 18034291.

12. Gungor AY, Turkkahraman H. Effects of airway problems on maxillary growth: a review. Eur J Dent. 2009; 3:250–254. PMID: 19756202.

13. Jena AK, Singh SP, Utreja AK. Sagittal mandibular development effects on the dimensions of the awake pharyngeal airway passage. Angle Orthod. 2010; 80:1061–1067. PMID: 20677955.

14. Speidel TM, Isaacson RJ, Worms FW. Tongue-thrust therapy and anterior dental open-bite. A review of new facial growth data. Am J Orthod. 1972; 62:287–295. PMID: 4559002.
15. Denison TF, Kokich VG, Shapiro PA. Stability of maxillary surgery in openbite versus nonopenbite malocclusions. Angle Orthod. 1989; 59:5–10. PMID: 2923322.
Figure 6
Coronal cone-beam computed tomography image showing nasal septum deviation, right turbinate hypertrophy, and left maxillary sinus congestion.

Figure 9
Coronal cone-beam computed tomography image showing complete resolution of upper airway obstruction.
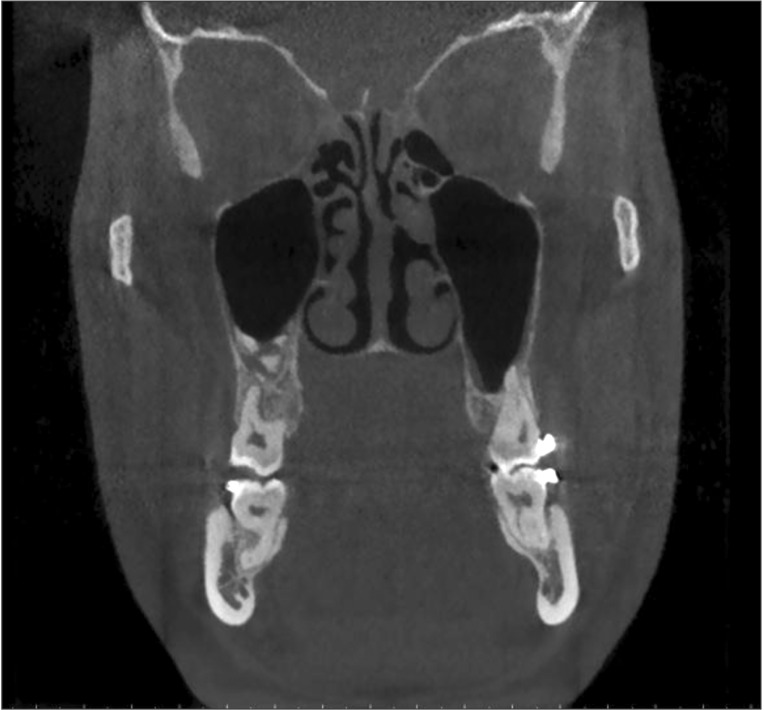
Table 1
Summary of the cephalometric analysis
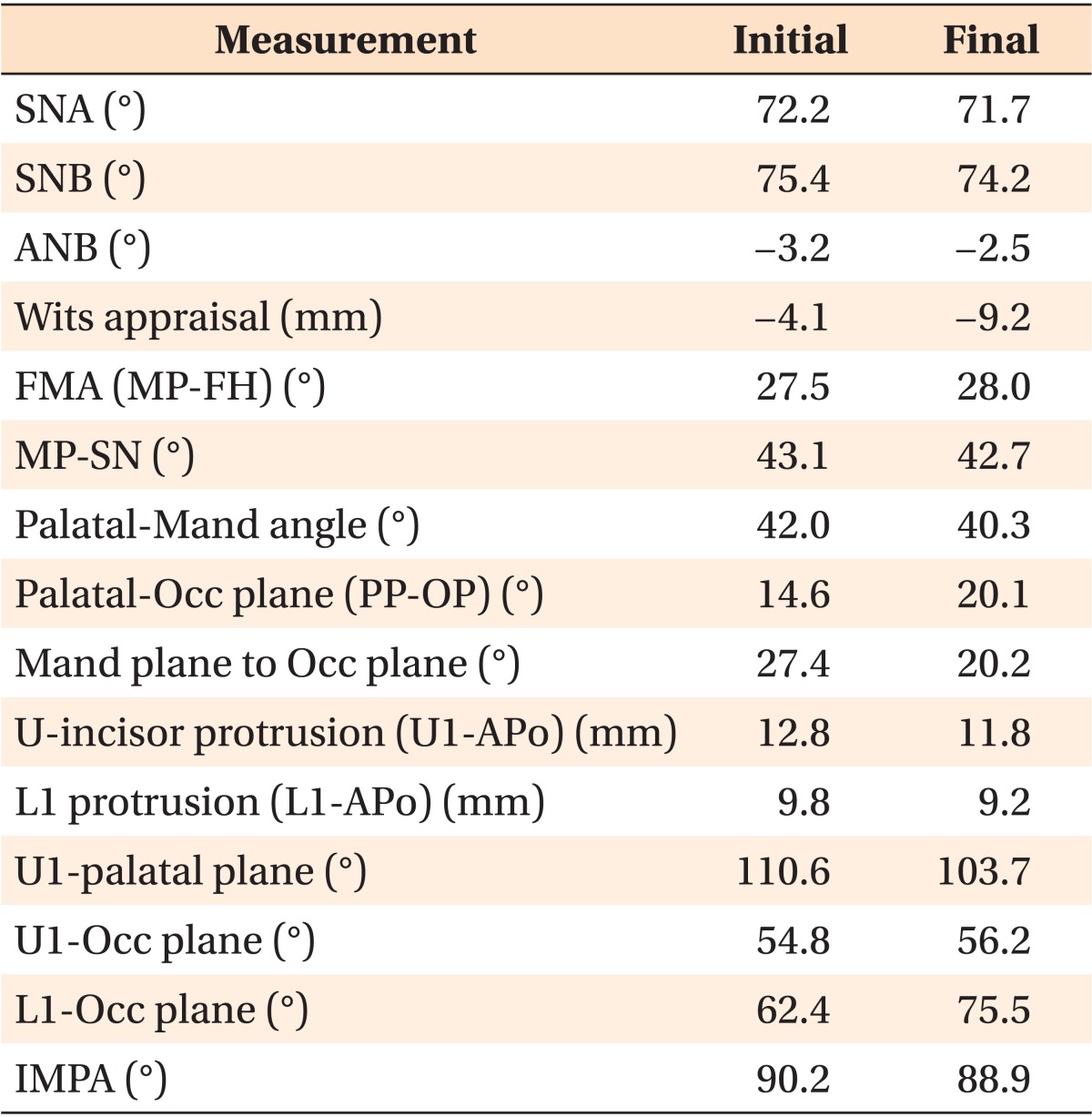
SNA, sella - nasion- A point; SNB, sella - nasion- B point; ANB, A point - nasion - B point; FMA, Frankfort mandibular plane angle; MP, mandibular plane; FH, Frankfort ; Mand, mandibular; Occ, occlusal; U, upper; U1, upper incisor; L1, lower incisor; APo, A point - pogonion; IMPA, lower incisor mandibular plane angle.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download