Abstract
A 12-year-old girl was referred to our clinic for evaluation of an unaesthetic dental appearance. All permanent teeth were erupted, while the deciduous maxillary right canine was retained. Cone-beam computed tomography revealed a complete transposition of the maxillary left canine and first premolar involving both the crowns and the roots. Initial cephalometric analysis showed a skeletal Class III pattern, with a slight maxillary retrusion and a compensated proclination of the upper incisors. The patient's teeth were considered to be in the correct position; therefore, we decided to attempt treatment by correcting the transposition and using only orthodontic compensation of the skeletal Class III malocclusion. After 25 months of active orthodontic treatment, the patient had a Class I molar and canine relationship on both sides, with ideal overbite and overjet values. Her profile was improved, her lips were competent, and cephalometric evaluation showed acceptable maxillary and mandibular incisor inclinations. The final panoramic radiograph showed that good root parallelism was achieved. Two-year follow-up intraoral photography showed stable results.
The positional interchange of two adjacent teeth is referred to as tooth transposition.123 A number of theories have been proposed to explain this anatomical condition. Some authors believe it is of genetic origin4567 while others consider that supernumerary teeth or retained deciduous teeth may cause dental transpositions.8
The most common transposition occurs between the maxillary cuspid and first premolar.910 Unilateral transpositions are more common than bilateral, and the left side is more frequently involved than the right.12391011
In complete tooth transpositions, all teeth are involved. In incomplete tooth transpositions, only the crowns are involved, while the roots remain in the correct positions.11213
In cases of tooth transposition, orthodontic therapy may be performed with or without tooth extraction. When teeth are not to be extracted, the orthodontist should consider the relative advantages of aligning teeth in a corrected position or in their transposed position. Factors to be considered when choosing the treatment include root and crown position (which are related to the risk of root resorption), gingival quality and gingival level of the transposed teeth, risk of caries, duration of orthodontic treatment,13 dental morphology and the need for dental reshaping, occlusal considerations related to the canines, and facial aesthetics.11
This case report describes the successful treatment of a patient with the maxillary canine and first premolar (MxC.P1) that was corrected with orthodontic therapy. The patient was treated by aligning all teeth into their correct position.
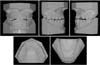
A 12-year-old patient was referred to our clinic for evaluation of an unaesthetic dental appearance. The intraoral examination showed that all permanent teeth were erupted, while the deciduous maxillary right canine was retained. No arch length discrepancy was noted on the upper or lower arch. Her overbite was reduced (0 mm), with an edge-to-edge relationship between the upper and lower incisors. The upper dental midline was centered with the facial midline; the lower dental midline was deviated 1 mm to the right (Figures 1 and 2).
Cone-beam computed tomography (CBCT) examination revealed a complete transposition of the maxillary left canine and first premolar, close contact between the roots of the left canine and first premolar, and resorption of the distal root surface of the left first premolar (Figures 3 and 4). Skeletal analysis showed a Class III malocclusion with increased vertical height. The upper incisors were proclined and the lower incisors were retroclined (Table 1). Soft tissue cephalometric analy showed a dolichofacial pattern with a harmonic profile at rest; the nasolabial angle was within the reference range and the labiomental angle appeared slightly increased.
During spontaneous smiling, the patient's facial profile appeared to be remarkably concave because of the downward displacement of the tip of the nose. Her lips appeared adequate and competent, masking the skeletal discrepancy. The patient's periodontal tissues were thin in the frontal mandibular area, and her level of oral hygiene was good (Figure 1).
The treatment objectives were to obtain a Class I molar and canine relationship with ideal upper and lower incisor inclination, to correct the lower midline with an ideal overjet and overbite, and to correct the MxC.P1 transposition on the left side without extractions and without increasing resorption of the root of the first premolar.
The following treatment alternatives were considered for the transposed teeth: 1) extraction of all first premolars; 2) extraction of the maxillary left canine or first premolar; and 3) extraction of no teeth, with teeth aligned either in the transposed position or in a corrected position. The extraction options were eliminated because of the patient's Class III profile and the thin periodontal tissue in her anterior lower arch. Extraction therapy may also cause unintended lingual crown inclination of the mandibular incisors.
Taking into account the skeletal Class III pattern with the slight maxillary retrusion and compensated proclination of the upper incisors, three options were considered: a) an orthognathic surgical operation to correct the skeletal Class III malocclusion; b) orthopedic treatment with rapid palatal expansion and reverse headgear to correct the maxillary retrognathia, followed by orthodontic treatment to correct the dental malocclusion; and c) orthodontic treatment with dental compensation using intermaxillary elastics.
With all of these options, the transposition of the left canine and first premolar could be treated either by aligning the teeth in the transposed order or by correcting the transposition. In an orthognathic operation, we would have positioned the upper incisors in the correct inclination relative to the maxillary occlusal plane, and in the same manner we would have replaced the upper canines in the correct position by correcting the left transposition. An orthognathic operation would have been performed at a later time, closer to the end of skeletal growth. The patient refused this option. Because she was only 12 years old, rapid palatal expansion and reverse headgear could not be considered. Therefore, we decided to treat her only with orthodontic compensation of the skeletal Class III malocclusion.
Because the MxC.P1 transposition was complete, maintaining the transposed order during alignment would have required less time and less risk of worsening the premolar root resorption than would correction of the transposition. However, maintaining the transposition might have required extensive restorative camouflaging of the left canine and first premolar. The patient preferred to have her teeth restored to their correct positions; therefore, we decided to correct the transposition to achieve a Class I canine and molar relationship.
Straightwire passive self-ligating brackets (Damon 3MX; Ormco Corporation, Orange, CA, USA) were placed on both arches. Because of the incisors' inclination and the plan to use Class III intermaxillary elastics to correct the molar and canine relationship, a low torque prescription was used on the upper frontal teeth (+7° torque value) and standard torque was used on the lower incisors (-1° torque value). In order to correct the transposition, an upper central incisor bracket with a higher torque prescription was bonded to the left first premolar (+17° torque value). The bracket slot was positioned at the same level as the second premolar bracket slot in order to prevent crown tipping. The root of the first premolar could thus be moved palatally without crown tipping (Figure 5).
Because the crown of the first premolar was in the correct position, we applied a passive laceback between 26 and 24. In this way, prevention of mesial tipping of the first premolar was achieved during the alignment phase.
After nine months of treatment, the first premolar had a good positive crown torque. This condition was quite evident because the palatal cuspid of the premolar was extruded as compared with the buccal cuspid of the same tooth (Figure 6).
A full-thickness buccal flap was performed and a metal button was bonded to the left impacted canine (Figure 7A). The crown of the canine was at the same level as the first premolar crown. To facilitate the extrusion of the canine, a ligature wire was connected between the button and the copper-nickel-titanium 0.014 archwire. During extrusion, mesial movement of the impacted canine was accomplished with a ligature wire placed mesially and a coil spring placed between the lateral and first premolars on the left side. The mucosal flap was closed over the canine (Figure 7B). A continuous ligature wire was used on the upper frontal teeth in order to reduce flaring.
After three months, the canine completely moved over the premolar and the crown appeared under the mucosa. The crown was exposed with a diode laser, and a positive torque bracket (+7° torque value) was bonded to the tooth. The orthodontic treatment was completed in 25 months.
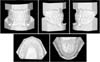
After 25 months of active orthodontic treatment, the patient had a bilateral Class I molar and canine relationship with good overbite and overjet values. The profile was improved, the lips were competent, and the cephalometric evaluation showed acceptable maxillary and mandibular incisor inclinations. The final panoramic radiograph showed that good root parallelism was achieved. The superimpositions (alignment tracings of the sella-nasion line at the sella) showed mesial movement of the upper molars, a reduction of the upper incisor angle, and a slightly increased proclination of the lower incisors (Figure 8). Gingival levels and periodontal tissue architecture were adequate, oral hygiene was good, the smile appeared natural, and the smile line was correct. A lower splint retainer from cuspid to cuspid and a Boston retainer with vestibular resin in the upper anterior zone were applied for the retention period. Incisal and canine guidances were present (Figures 8, 9, 10, Table 1).
After two years, intraoral photographs were taken, and the records showed that stable results were achieved with the correction of the MxC.P1 transposition using nonextraction therapy in this patient with Class III malocclusion (Figure 11).
Management and treatment of a maxillary caninepremolar transposition can be challenging for an orthodontist. The clinician must first decide whether to correct the transposition or maintain the teeth in their transposed positions.1415
Both approaches have advantages and disadvantages. Correcting the transposition may result in a natural and aesthetic arch form, a pleasant smile, and good architecture of the gingival margins. Disadvantages of correcting the transposition include long treatment time, the potential risk of root resorption of involved teeth, difficult torque control for the cuspid and first premolar, and a high risk of dehiscence and fenestration of supporting bone.
Aligning the teeth while maintaining the transposition may lead to aesthetic and functional problems. The palatal cusp of the premolar may constrain lateral jaw movements and cause intercuspidation problems; crown reshaping at the conclusion of the treatment must therefore be considered. This treatment option may also cause an unaesthetic gingival contour on the transposed area of the maxilla. Advantages of maintaining the transposition include a shorter treatment duration, easier mechanics for the orthodontist, and less risk of root resorption.
Before making a decision, the clinician should examine the patient clinically and/or radiographically for evidence of fenestration, dehiscence, or root resorption. The current gold standard for the radiographic diagnosis of both impacted and transposed teeth is CBCT.161718 With this diagnostic tool, the patient is exposed to low doses of radiation, and detailed information about craniofacial structures can be obtained.18
The CBCT of our patient revealed a complete MxC. P1 transposition on the left side of the maxilla, with a partial root resorption on the distal side of the first premolar. The crown of the premolar was in the correct position, but the root was inclined mesially and the cuspid crown was adjacent to the root apex of first premolar. Together with the patient, we decided to move the displaced tooth to its correct position. Tooth movements were monitored carefully to minimize the risk of worsening the premolar root resorption. The key biomechanical goals were as follows: 1) to maintain the mesial root inclination of the premolar, which we accomplished by keeping the bracket slot parallel and at the same level as brackets on adjacent teeth; 2) to move the premolar root palatally in order to achieve a safe distance between cuspid crown and premolar root, which we did by using a high-torque incisor bracket on the first premolar; 3) to move the cuspid forward to its correct mesial position; and 4) to provide ideal second- and third-order bends and values for the cuspid and first premolar in order to guarantee good intercuspidation and pleasant aesthetic results.
At the conclusion of the orthodontic treatment, a healthy periodontium was maintained; premolar root resorption had not progressed (Figure 12); the patient's profile was maintained; and intercuspidation was adequate, with molar and cuspid Class I relationships on both sides. The final CBCT results showed that displaced tooth roots were located in maxillary medullar bone without fenestrations or dehiscences (Figure 13). Our patient understands that the Class III skeletal pattern must be monitored until her growth is complete.
Orthodontic treatment of dental transposition is always challenging. Clinicians should consider the advantages and limitations of extraction and nonextraction treatment. They must also understand their patients' anatomical limitations, ability to comply with treatment requirements, and aesthetic expectations. CBCT is essential for determining the appropriate treatment.
Figures and Tables
Figure 4
Three-dimensional reconstruction of the maxilla, with transposition of the left canine and first premolar.

Figure 5
Intraoral photographs at bonding stage. A high-torque central incisor bracket (+17o torque value) was bonded to the first left premolar to facilitate the correction of the transposition.

Figure 6
Intraoral photographs of the left side, showing the positive crown torque of the first premolar. The palatal cuspid of the tooth is extruded compared with the buccal cuspid of the same tooth.

Figure 7
Surgical procedure. A, Intraoral photo of the surgical exposure of the left canine; B, mucosal flap closed over the canine.

Figure 8
Post-treatment records: radiographs and cephalometric tracings (black, before treatment; red, after treatment).

Figure 12
Three-dimensional image of the absence of progression of left first premolar (2.4) root resorption.

Table 1
Comparison between pre- and post-treatment cephalometric measurements

SNA, Sella-nasion-A point; SNB, Sella-nasion-B point; A-Na perp, distance from A point to the perpendicular line to Frankfurt plane passing from Na point; Pg-Na perp, distance from Pg to the perpendicular line to Frankfurt plane passing from Na point; FMA, Frankfort mandibular plane angle; FH, Frankfort plane; MP, mandibular plane; SN, Sella-nasion; U1, upper incisor; PP, palatal plane; L1, lower incisor; IMPA, lower incisor mandibular plane angle.
The patient maintained a Class III skeletal pattern with a good dental compensation.
References
1. Babacan H, Kiliç B, Biçakçi A. Maxillary canine-first premolar transposition in the permanent dentition. Angle Orthod. 2008; 78:954–960.

2. Sato K, Yokozeki M, Takagi T, Moriyama K. An orthodontic case of transposition of the upper right canine and first premolar. Angle Orthod. 2002; 72:275–278.
3. Cho SY, Chu V, Ki Y. A retrospective study on 69 cases of maxillary tooth transposition. J Oral Sci. 2012; 54:197–203.

4. Chattopadhyay A, Srinivas K. Transposition of teeth and genetic etiology. Angle Orthod. 1996; 66:147–152.
5. Peck L, Peck S, Attia Y. Maxillary canine-first premolar transposition, associated dental anomalies and genetic basis. Angle Orthod. 1993; 63:99–109.
6. Feichtinger C, Rossiwall B, Wunderer H. Canine transposition as autosomal recessive trait in an inbred kindred. J Dent Res. 1977; 56:1449–1452.

7. Svinhufvud E, Myllärniemi S, Norio R. Dominant inheritance of tooth malpositions and their association to hypodontia. Clin Genet. 1988; 34:373–381.

8. Laptook T, Silling G. Canine transposition: approaches to treatment. J Am Dent Assoc. 1983; 107:746–748.
9. Farret MM, Farret MM, Farret AM, Hollweg H. Unusual orthodontic approach to a maxillary caninepremolar transposition and a missing lateral incisor with long-term follow-up. Am J Orthod Dentofacial Orthop. 2012; 142:690–697.

10. Ely NJ, Sherriff M, Cobourne MT. Dental transposition as a disorder of genetic origin. Eur J Orthod. 2006; 28:145–151.

11. Ciarlantini R, Melsen B. Maxillary tooth transposition: correct or accept. Am J Orthod Dentofacial Orthop. 2007; 132:385–394.

12. Giacomet F, Araújo MT. Orthodontic correction of a maxillary canine-first premolar transposition. Am J Orthod Dentofacial Orthop. 2009; 136:115–123.

13. Nishimura K, Nakao K, Aoki T, Fuyamada M, Saito K, Goto S. Orthodontic correction of a transposed maxillary canine and first premolar in the permanent dentition. Am J Orthod Dentofacial Orthop. 2012; 142:524–533.

14. Weeks EC, Power SM. The presentations and management of transposed teeth. Br Dent J. 1996; 181:421–424.

15. Filho LC, Cardoso MA, An TL, Bertoz FA. Maxillary canine-first premolar transposition. Restoring normal tooth order with segmented mechanics. Angle Orthod. 2007; 77:167–175.
16. Nakajima A, Sameshima GT, Arai Y, Homme Y, Shimizu N, Dougherty H Sr. Two- and three-dimensional orthodontic imaging using limited cone beam-computed tomography. Angle Orthod. 2005; 75:895–903.
17. Walker L, Enciso R, Mah J. Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2005; 128:418–423.

18. Maverna R, Gracco A. Different diagnostic tools for the localization of impacted maxillary canines: clinical considerations. Prog Orthod. 2007; 8:28–44.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download