INTRODUCTION
MATERIALS AND METHODS
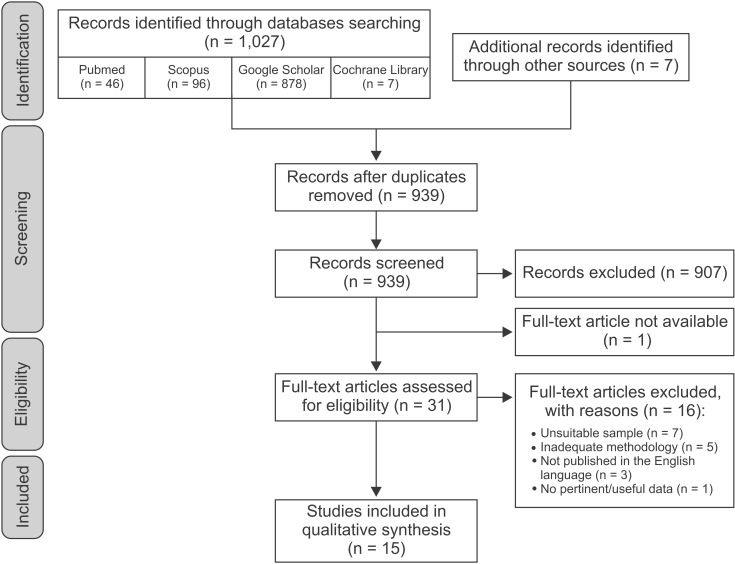
Search strategy
Screening and study selection
Type of study: Randomized or non-randomized controlled trials, cohort or case-control studies (with a minimum sample size of 10 patients in each group) addressing the research question of the predictive value of cephalometric analysis in oral appliance treatment outcomes in adult OSA patients. Studies had to be published in English in an international peer-reviewed literature
Population: Male or female adult patients (≥ 18 years old) with a polysomnographic diagnosis of OSA (i.e., 5 or more respiratory events [apneas or hypopneas] per hour of sleep)
Intervention: Treatment with any MAD for OSA The exclusion criteria were:
Lack of a clear description of inclusion/exclusion criteria
Previous and/or current surgical or pharmacological interventions
Limitation to severe OSA patients
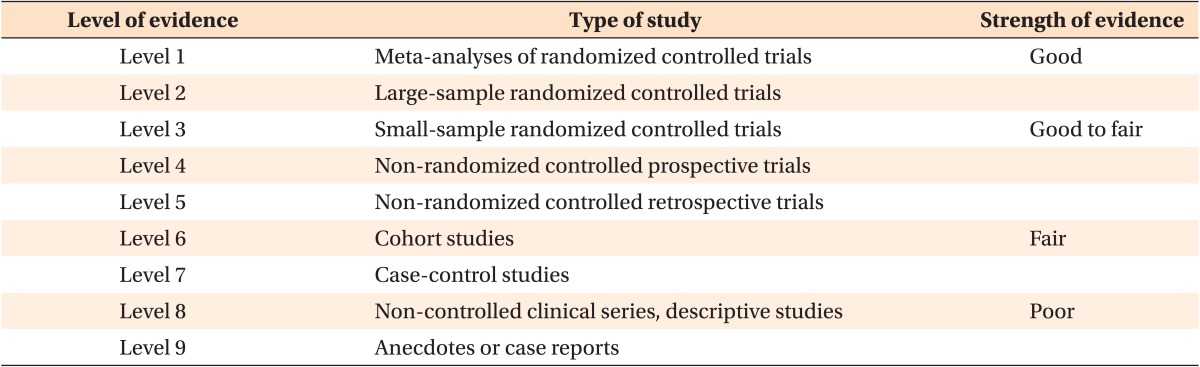
Data extraction and quality assessment of selected studies
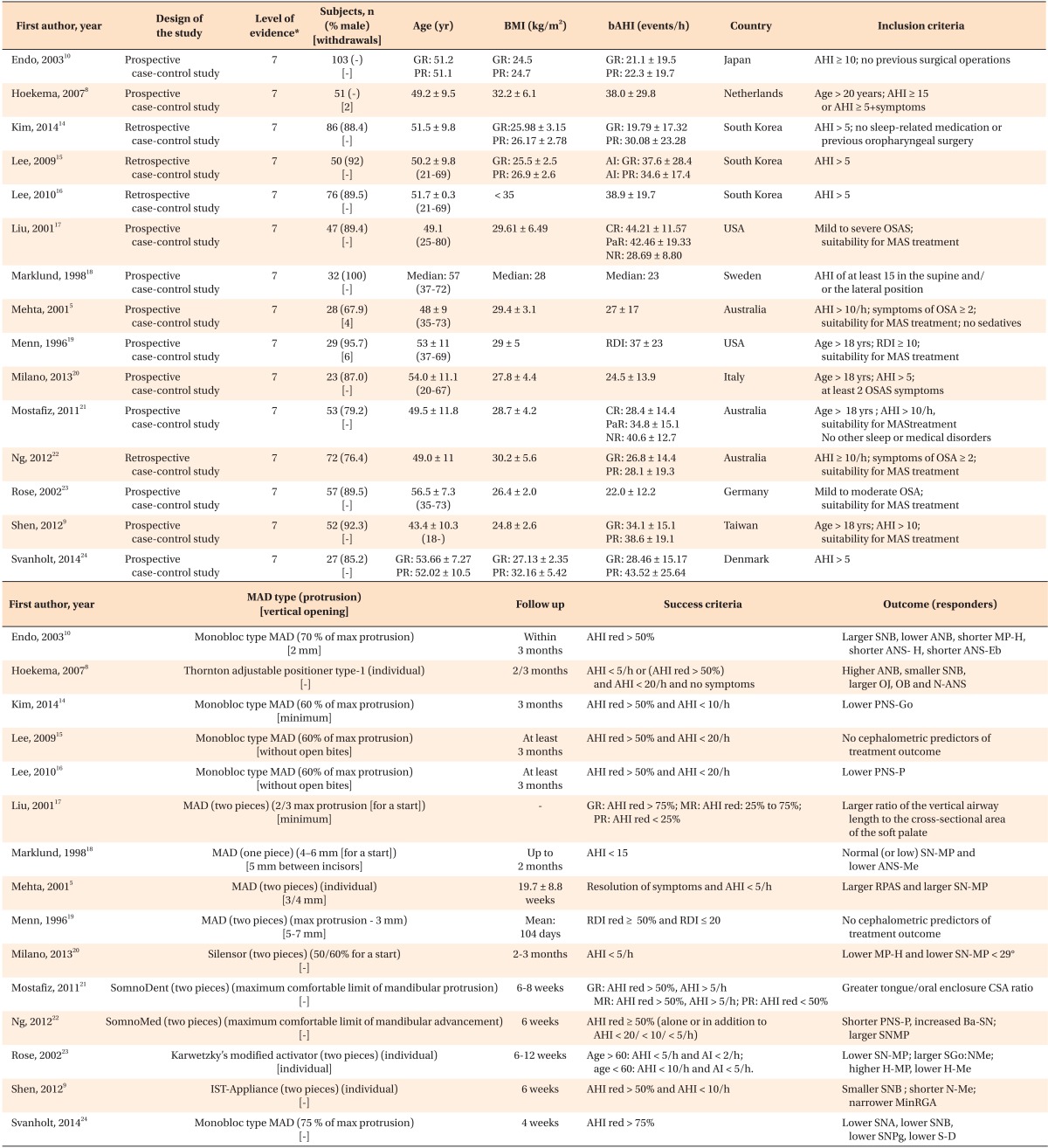
RESULTS
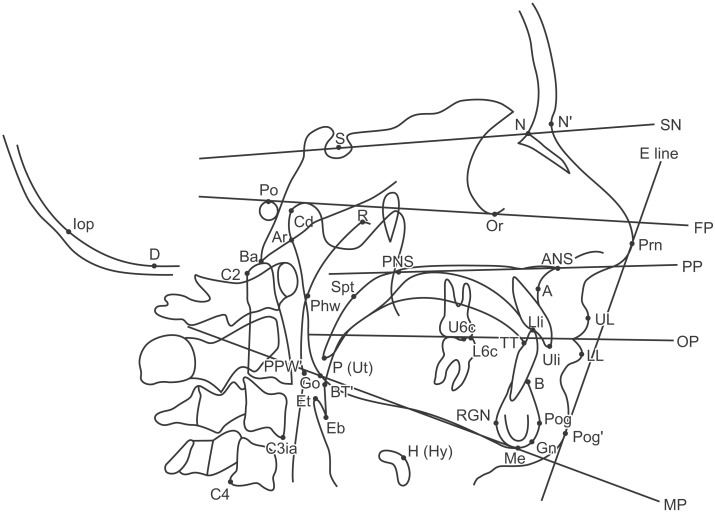
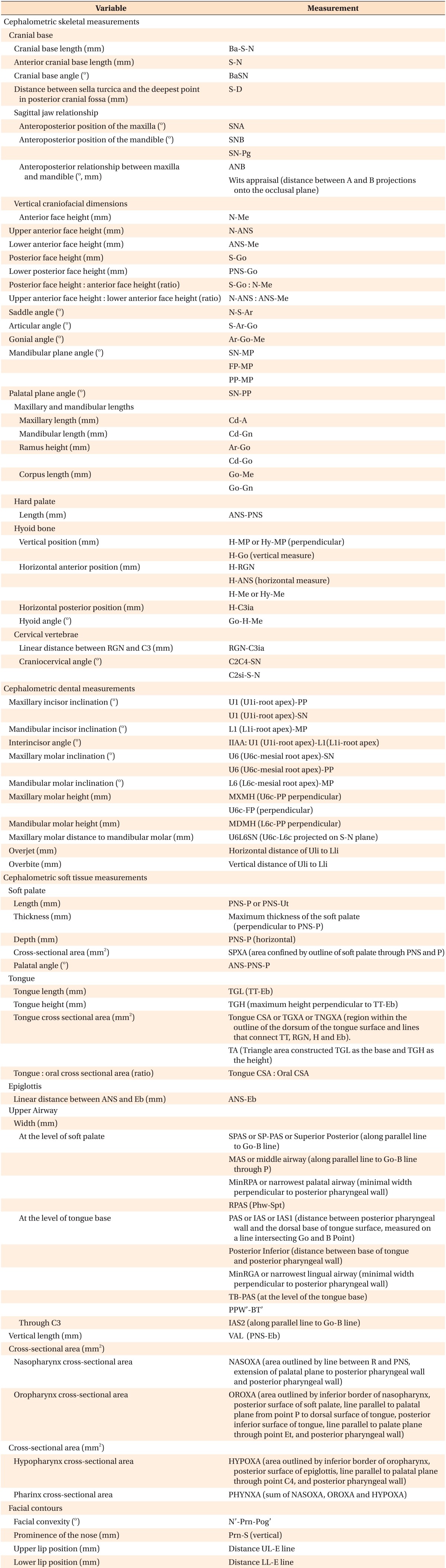
Cephalometric skeletal measurements
Cranial base
1-piece MAD: Svanholt et al.24 found that the distance between the sella turcica and the deepest point in the posterior cranial fossa was lower in the group that responded positively to MAD therapy.
2-piece MAD: Both cranial base and anterior cranial base lengths were reported to be non-predictive of MAD treatment outcome.5822 Two studies addressed the predictive value of cranial base angle with contrasting results; one found an increased cranial base angulation to be predictive of MAD treatment success22 and the other did not.5
Sagittal jaw relationship
1-piece MAD: Data concerning sagittal jaw relationship were controversial. SNA and ANB were recognized either as predictive of treatment success when decreased1024 or as non-predictive101418 of treatment outcome. SNB was found to be non-predictive1418 or predictive of treatment success when increased10 or decreased.24
2-piece MAD: The majority of papers indicated that sagittal jaw relationship cephalometric parameters were not suitable for predicting treatment outcome (SNA,58919202122 SNB,519202122 ANB,517202122 Wits appraisal20). However, a decreased SNB value89 or an increased ANB value8 were occasionally reported as predictive of treatment success.
Vertical craniofacial dimensions
1-piece MAD: Vertical craniofacial dimension parameters were usually recognized as non-predictive of treatment outcome,1424 with the exception of lower anterior face height,18 lower posterior face height,14 and mandibular plane angle,18 which were occasionally identified as predictive of treatment success when decreased.
2-piece MAD: Saddle angle, articular angle, gonial angle, palatal plane angle, posterior face height, and the ratio between upper anterior face height and lower anterior face height were not useful for predicting MAD treatment outcomes.920212223 The majority of the papers ascribed a non-predictive role to anterior face height, upper anterior face height, lower anterior face height, and the ratio between posterior face height and anterior face height, but a lower anterior face height value9 as well as higher values of upper anterior face height8 and of the ratio of posterior face height to anterior face height23 were also occasionally found in good responders. Data on the predictive role of mandibular plane angle were conflicting: 3 out of 7 studies found it to be non-predictive of treatment outcomes,8921 2 studies indicated an increased value as a predictor of treatment success,522 and 2 studies reported a decreased value as a predictor of treatment success.2023
Hyoid bone
1-piece MAD: Endo et al.10 found decreased values of MP-H, H-Me, and ANS-H to be predictive of MAD treatment success, whereas Kim et al.14 supported a non-predictive role of H-Me and ANS-H.
2-piece MAD: There was general agreement that H-RGN, C3ia-H, H-Go, Go-H-Me were not suitable for predicting MAD treatment outcomes.9172021 Rose et al.23 found that decreases in H-Me and ANS-H were predictive of treatment success, while Hoekema et al.8 did not. Data on MP-H were conflicting. Five out of 7 studies found it to be non-predictive,5891921 while the two others reported that decreased MP-H20 and increased MP-H23 were predictive of treatment success.
Cervical vertebrae
1-piece MAD: Svanholt et al.24 found that the prevalence of and severity of morphological deviations of the upper spine were greater in the group of patients that failed MAD.
2-piece MAD: Neither the linear distance between RGN and C3ia21 nor the craniocervical angle2122 seemed to be predictive of MAD treatment outcome.
Cephalometric dental measurements
1-piece MAD: Studies investigating dental parameters agreed on the lack of predictive value of these measurements for treatment outcome.1424
2-piece MAD: Overjet and overbite were widely recognized as non-predictive of treatment success.917202223 However, Hoekema et al.8 found that increased overjet and overbite were prognostically favorable. Increased maxillary molar height also seemed to be associated with a better chance of successful treatment.17 None of the other cephalometric dental measurements exhibited predictive value.2123
Cephalometric soft tissue measurements
Soft palate
1-piece MAD: Soft palate depth and thickness and palatal angle were identified as non-predictive of treatment outcomes,1014 whereas data concerning soft palate length, which, when decreased,16 was recognized both as non-predictive of treatment outcome1415 and predictive of treatment success, were controversial.
2-piece MAD: Shen recognized soft palate thickness as non-predictive of treatment outcome.9 The role of soft palate length was controversial. Two out of 6 studies found that decreased soft palate length was predictive of treatment success922 while 4 did not.8192021
Tongue
1-piece MAD: There was general agreement that the cephalometric variables of tongue length, height, and cross-sectional area were not useful for predicting MAD treatment outcomes.101415
2-piece MAD: Tongue-related cephalometric variables were widely recognized as non-predictive of MAD treatment outcome9172223 with the sole exception of tongue/oral enclosure cross-sectional ratio, which Mostafiz et al.21 found was increased in complete responders.
Epiglottis
1-piece MAD: Only 1 study examined the predictive role of the distance between ANS and Eb in treatment outcomes, finding that the greater this distance, the less effective the treatment.10
2-piece MAD: No study investigated the predictive role of epiglottis parameters.
Upper airway
1-piece MAD: Upper airway parameters were unanimously recognized as non-predictive of MAD treatment outcome.101416
2-piece MAD: Neither vertical length nor cross-sectional area were found to be predictive of outcome. 91720 Concerning the upper airway widths, only 1 study (Shen et al.9) found significantly decreased retroglossal width in good responders. The majority showed a non-predictive role for retropalatal width, although Mehta et al.5 and Liu et al.17 found an increased retropalatal space in good and poor responders, respectively.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download