Abstract
Objective
The aim of this study was to investigate three-dimensional molar displacement after distalization via miniscrews and a horizontal modification of the trans-palatal-arch (TPA).
Methods
The subjects in this clinical trial were 26 Class II patients. After the preparation of a complete set of diagnostic records, miniscrews were inserted between the maxillary 2nd premolar and 1st molar on the palatal side. Elastic modules connected to the TPA exerting an average force of 150-200 g/side parallel to the occlusal plane were applied. Cone-beam computed tomography was utilized to evaluate the position of the miniscrews relative to the adjacent teeth and maxillary sinus, and the direction of force relative to molar furcation. The distances from the central point of the incisive papilla to the mesiopalatal cusps of the 1st maxillary molars and the distances between the mesiopalatal cusps of the left and right molars were measured to evaluate displacement of the maxillary molars on the horizontal plane. Interocclusal space was used to evaluate vertical changes.
Class II malocclusion can be appraised as skeletal and dental Class II.1 The treatment of skeletal Class II malocclusion in non-growing individuals involves either surgical correction of the jaw abnormality, or orthodontic camouflage which usually requires the extraction of premolars or distal movement of the maxillary molars.23 For several years, extraoral appliances such as headgear were the most widely used distalizing appliances, but they are not esthetically desirable or socially acceptable, especially for adults. They are also removable and require patient compliance, which can compromise the results.4
Several intraoral noncompliance devices for maxillary molar distalization have been recommended since the 1980s.5 These include but are not limited to the Hilgers pendulum appliance, Jones jig distalization apparatus, open nickel-titanium (NiTi) push coils, distal jet, repelling magnets, and molar slider.67891011 Numerous side effects have been reported in association with these tooth-borne distalizing appliances, including anchorage loss of the maxillary premolars and flaring of the incisors, and a significant amount of relapse can occur. Also, the distalized molars must be used for anchorage during retraction of the premolars and anterior teeth,5 resulting in a bite-opening effect that is not tolerable for most patients.
Temporary anchorage devices (TADs) have been investigated, in an effort to overcome some of the side effects associated with tooth-borne distalizing appliances.1 Dental implants, miniscrews, and miniplates have been used for skeletal anchorage.11112131415 TADs have several advantages. They are relatively easy to place, inflict less trauma on the oral tissues, are stable under normal degrees of force, and can bear force immediately after placement.
Miniscrews, in particular, are relatively inexpensive and patient compliance is limited to maintaining good oral hygiene. Moreover, they exert immediate orthodontic force, reducing the total treatment time. Given their small size, they can be inserted in a variety of sites on the alveolar and basal bones.316171819 However, they have been associated with damage to anatomical structures such as dental roots, nerves, and blood vessels, and there are the possibilities of screw breakage on placement and removal, and screw failure with peri-implant inflammation. The reported success rates of miniscrews range from 80% to 95%.20
The placement of miniscrews in the buccal interradicular bone is one of the most common approaches used to provide skeletal anchorage. The interradicular space is a potentially advantageous region for insertion, because there is less potential for complications related to soft tissue irritation, particularly if they are placed through the attached gingiva.20 Although adjacent teeth may limit mesiodistal tooth movement, buccal interdental miniscrews are very useful for molar distalization, due to their ease of placement, and simple application during treatment. With a properly positioned TAD, 3 mm of distal movement per side can be achieved.21
On the palatal side, a TAD may be placed paramedian (near the midline) or in the interdental space. While paramedian appliances usually require more expensive and sophisticated attachments, the risk of root damage associated with them is minimal.161222 TADs placed on the palatal interdental area can apply distalization forces directly to the molar. Moreover, these TADs can also control the mesiodistal axis of the molar via manipulation of the line of action.22
We have introduced a new appliance using palatal miniscrews "mimi-implant-aided (MIA) in the interdental area between the 1st molar and 2nd premolar root and a trans-palatal arch (TPA) to overcome some of the mechanical shortcomings of previous appliances, in contexts including anterior protrusion, extrusion of posterior teeth, and tipping of molar teeth (MIA-TPA). Traction between TADs in the palatal interdental area and a TPA can produce direct distalization force that travels through the center of resistance of molars (Figure 1). The purpose of the present study was to measure the three-dimensional (3D) movement of 1st molars after using this newly designed distalizing appliance.
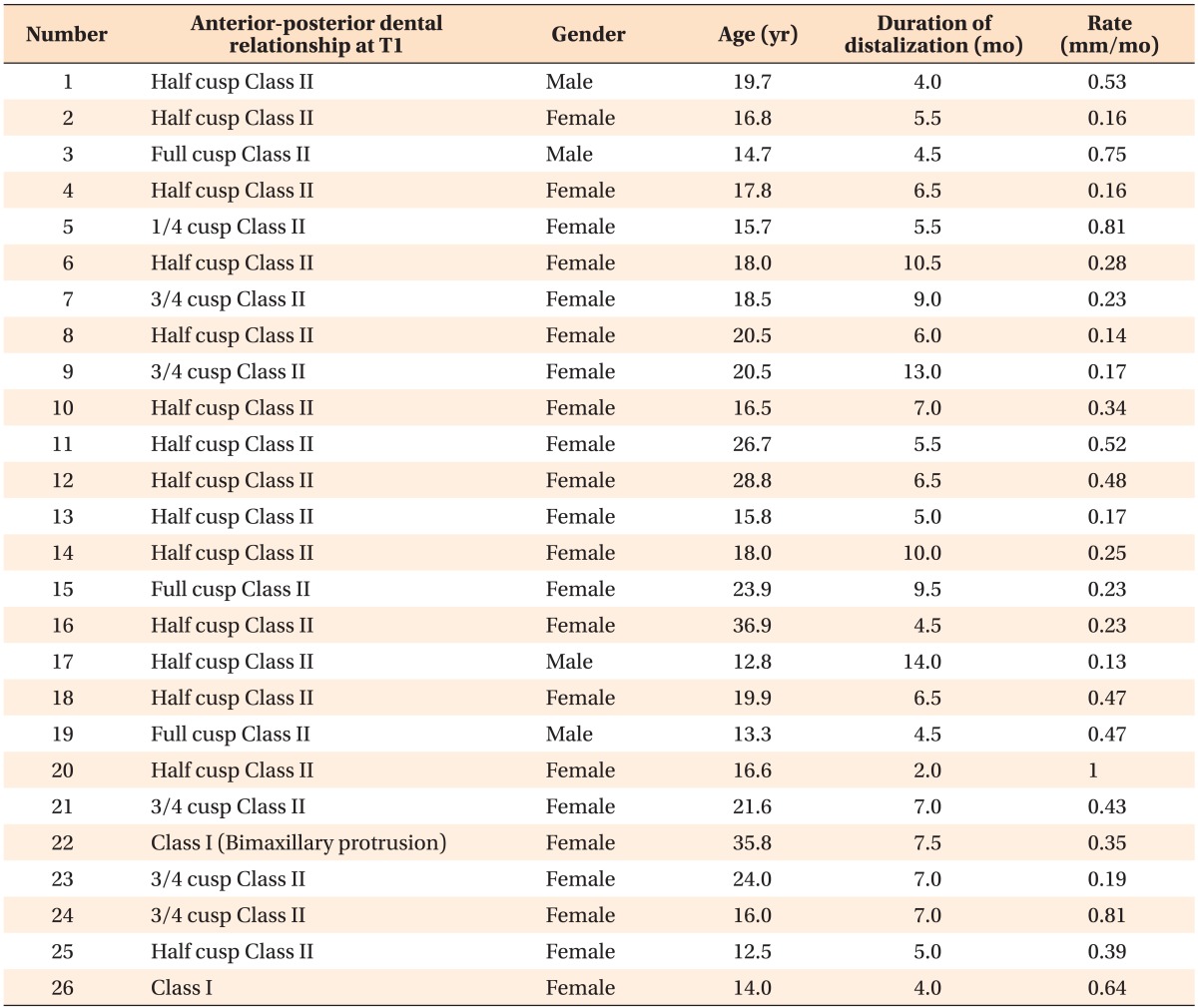
The sample group consisted of 26 patients (22 females, 4 males) with an average age of 19.8 ± 6.3 years (range 12-36 years) at the beginning of treatment (Table 1). The main inclusion criterion was Angle Class II malocclusion of no more than one cusp on each side. Patients with missing teeth, substantial restorations, or any craniofacial malformation were excluded from the study. The study was approved by the University Research and Ethics Committee, and registered as a clinical trial at Iranian Registry of Clinical Trials (No. IRCT201302269085N3). All patients (and their parents in the case of minors) were informed about the treatment procedures involved, and informed consent was provided.
After preparing the initial diagnostic records including dental casts, a dentist placed two miniscrews, each with a range of 8-10 mm in length and 1.4, 1.6, or 2.0 mm in diameter in the palatal interdental area under local anesthesia. Miniscrews were inserted between maxillary 2nd premolars and 1st molars with a self-tapping technique, approximately 5-6 mm from the gingival crest at an angle of 60-80° relative to the long axis of adjacent teeth. The heads of the screws were approximately 2 mm above the mucosal surface, to facilitate the attachment of elastic modules. A palatal sheath was then placed on the 1st molar's band. A TPA was made on a cast with stainless steel wire of 0.8 mm in diameter, with two helices or hooks soldered into the lateral incisors area. Final adjustment of the TPA was performed inside the patient's mouth.
Miniscrews were immediately placed under loading. Miniscrews were loaded with an average force of 150-200 gram-force/side via elastic modules, and ligature wire was used to connect the TPA, almost parallel to the occlusal plane of the miniscrew. Elastic modules were replaced every 3 weeks, and TPAs were adjusted appropriately. All of the other teeth were bonded from 2nd molar to 2nd molar with standard edgewise brackets and tubes (Dentaurum, Ispringen, Germany), and leveling and aligning were performed before the termination of distalization to reduce any possible anchorage loss after distalization. The final arch wire was 0.018-in stainless steel. A cone-beam computed tomography (CBCT) scan (Newtom 3G; Quantitative Radiology, Verona, Italy) was performed to evaluate the precise position of mini screws relative to adjacent teeth and the direction of the force relative to molar teeth.
After maxillary 1st molars were driven to super Class I relationship, distalization was terminated and a final impression was taken for final evaluation. Digital model analysis of molars was used to evaluate changes in the 3D position of the maxillary molars. Digital scans of models before and after distalization were prepared via a Maestro 3D dental scanner (AGE Solutions S.r.l., Pontedera, Italy). Maestro Ortho Studio software version 2.5 (AGE Solutions S.r.l.) was used to analyze the digital models.
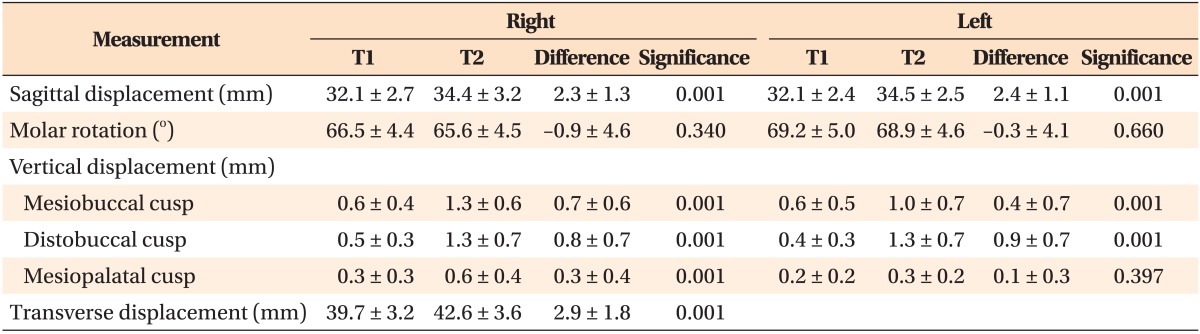
Reference points were used to analyze digital casts. The palatal rugae possesses unique characteristics, and as it tends to exhibit reasonable stability during growth, it may serve as a suitable reference point for longitudinal cast analysis.23 As the patients in the current study were not in an active growth period and no potential incisor movement was anticipated during the distalization period, as in Nalcaci et al.,1 the distance from the central point of the incisive papilla to the mesiopalatal cusp of the 1st maxillary molars was used to measure distalization. The distances between the mesiopalatal cusps of the left and right molars were measured to evaluate intermolar width. The angles between the incisive papilla and the distopalatal and mesiobuccal cusps of the 1st maxillary molars were measured to evaluate the rotation of maxillary molars1 (Figure 2). Interocclusal space at the mesiobuccal, distobuccal, and mesiopalatal cusps of the 1st maxillary molars was evaluated by occlusion inspection, and Maestro 3D scanner and software was used to evaluate vertical movement. After putting the casts in the maximum intercuspal position, the spaces between the maxillary 1st molar cusps and the antagonist tooth at T1 and T2 were measured via a 0.5-mm interval scale with a color coded tool (Figure 3).
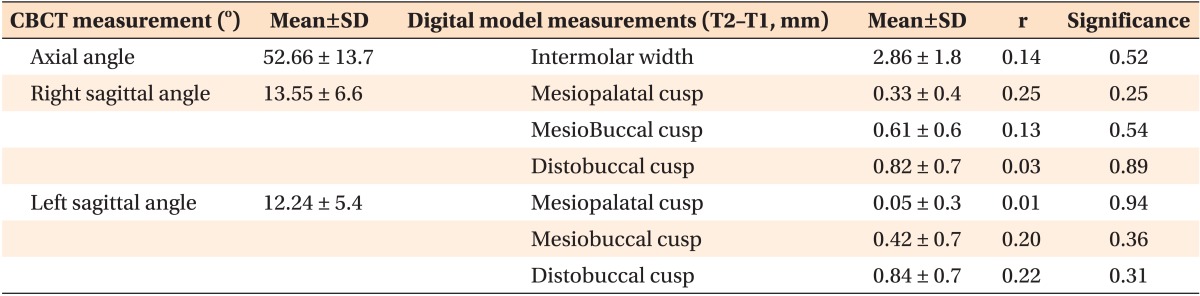
For CBCT analysis, Digital Imaging and Communications in Medicine (DICOM) files were imported to a Dolphin 3D 11 (Dolphin Imaging, Chatsworth, CA, USA). The orientation was adjusted in accordance with the palatal plane and midsagittal plane. Right and left sagittal and axial sections were prepared. In sagittal planes, a line was drawn along the helix in the TPA and miniscrew. The angle between this line and a line drawn parallel to the occlusal plane was measured on right and left 3D sagittal view. In 3D axial view, lines between the helix and the miniscrews on the right and left sides were drawn, and the angle between those lines (axial angle) was measured (Figure 4).
Descriptive statistics were used to examine the normal distribution of the data. Measurements were repeated one month after the initial measurements, and the reliability of the measurements was calculated via the intraclass correlation test. Reliability was between 79.7 and 97.0 for linear measurements, and between 93.8 and 96.6 for angular measurements. The paired t-test was used to compare measurements acquired before and after distalization in a digital cast. A probability of p < 0.05 was deemed to indicate statistical significance. Pearson's correlation was used to evaluate the relationships between CBCT parameters and digital cast parameters. Statistical Package for the Social Sciences ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analyses.
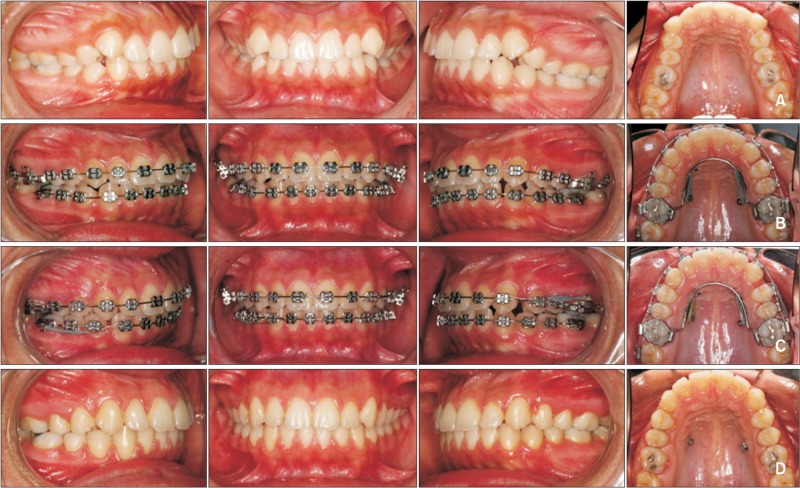
Maxillary 1st molars were moved distally an average of 2.3 ± 1.1 mm, and the difference between the right and left sides was not statistically significant (p = 0.63). The mean duration of distalization was 6.8 ± 2.8 months (range 2-14 months), thus the average rate of distalization achieved via the method utilized in the current study was 0.4 ± 0.2 mm/month. A representative case is shown in Figure 5.
Maxillary 1st molars were slightly rotated mesially around the palatal root after distalization, though the amount of rotation was not statistically significant (this rotation is shown with a minus sign in Table 2). The mean intermolar width increase was 2.9 ± 1.8 mm (range 0.6-6.8 mm). The examination of vertical movement of three cusps of the maxillary molars showed relative molar intrusion that was statistically significant, except in the left mesiopalatal cusp (Table 2). Twenty-three patients agreed to have initial CBCT scans. CBCT parameters were not significantly correlated with digital cast parameters (Table 3).
Orthodontists are frequently faced with mild to moderate Class II molar and canine relationships that they prefer not to treat via the extraction of premolars, and for which treatment via auxiliary methods is often unsatisfactory due to insufficient patient compliance. Many studies on intraoral maxillary molar distalization without patient cooperation have been performed, in order to solve the patient compliance problem associated with extraoral distalization appliances.110111220222425262728 In the present study, maxillary 1st molars were distalized via mini-implant-aided TPA.
In MIA-TPA, direct traction from elastic modules spanning from a miniscrew to a TPA helix is used to achieve molar distalization. Miniscrews were inserted into the palate in this study, wherein attached gingiva is not a major concern, in contrast to the buccal side. Moreover, there is more interdental space in the palate relative to the buccal side, and larger miniscrews (2 mm in diameter) can be inserted. In the present study, the protrusion of anterior teeth was completely prevented using this method.
The mesiodistal axis of molar movement can be controlled by adjusting the vertical position of miniscrews and/or the direction of the line of action relative to furcation. Thus, bodily tooth movement is promoted, rather than tipping movement. In the current study, a removable TPA was used which made possible both proper adjustment of the line of action, and the control of molar rotation. Other advantages of TPAs are their simplicity, and ease of fabrication. The appliance is of a reduced size relative to other similar devices, and was tolerated by all of our patients without any concerns. There were also no problems reported with regard to the maintenance of oral hygiene.
In the treatment protocol used in the current study, elastic modules were used to generate force. With regard to traction, elastic modules can produce the desired amount of force even at close distances. The elastic properties of the modules were lost relatively quickly in the oral cavity however, so the force applied was intermittent in nature, and they needed to be changed at least every 3 weeks. While NiTi pull coils allow for the application of more continuous force for distalization, they require a distance of at least 20 mm between the miniscrew and helix, to produce an appropriate level of force.
In this study, 3D models were used for the 3D analysis of maxillary molar movements. Two-dimensional (2D) analysis by superimposing pretreatment and posttreatment cephalometric tracings has commonly been used in orthodontic studies.26 There are some disadvantages of cephalometric radiographs and superimpositions. Patients must be exposed to additional radiation. The superimposition of lateral cephalograms is not easily accomplished, because the relevant radiographic landmarks and structures are frequently difficult to accurately trace. Also, the process of superimposing can be technique-sensitive.29 Cephalometric superimposition can reveal positional changes in the maxillary and mandibular dentition in both vertical and sagittal dimensions, but not in the buccopalatal direction. In contrast to 2D analysis, 3D analysis of serial dental models can provide further information on tooth movements, particularly in the buccolingual or transverse direction. The projection of bilateral teeth on the midsagittal plane also causes greater tracing errors because of the difficulty in identifying the bilateral teeth. Consequently, the separate investigation of the tooth movements on each side, which can be achieved relatively easily via 3D models, is seldom attempted via cephalometric analysis.26
In this study, the distal movement of molars was measured along the line connecting the central point of the incisive papilla and the mesiolingual cusp of the 1st molar. While this measurement does not reflect true distal movement, measuring the intermolar change can provide a clear determination of both the distal and buccal movement of maxillary molars according to best available anatomical reference points. Applying a distal force to maxillary molars moved them in three dimensions. With the device used in the current study, maxillary 1st molars were distalized 2.3 ± 1.1 mm. In other studies based on intraosseous anchorage appliances, distalization was between 1.3 and 6.4 mm.110202224262728 Distalization was higher in studies that used tooth-borne appliances such as pendulums or dual force distalizers supported by mini-implants for molar distalization.222527
The main reasons for the reduced distal movement of maxillary molars in our study were related to characteristics of our sample. The majority of patients in our sample required less than one cusp of distal movement. Nalcaci et al.1 distalized molars via miniscrews with open coil springs by an average 3.95 ± 1.35 mm. Gelgör et al.10 distalized molars by an average 3.9 ± 1.6 mm via screws supported by TPAs and NiTi open coil springs. Yamada et al.20 used miniscrews and elastomeric chain or NiTi closed coils for distalization, and average molar movement was 2.8 ± 1.6 mm.
The mean duration of distalization in our study was 6.8 ± 2.8 months, thus the rate of distalization was 0.4 ± 0.2 mm/month. In other studies, the duration of distalization was between 4.5 and 10.2 months.11020222425262728 Nalcaci et al.1 reported an average duration of 9.61 ± 2.1 months, and a rate of 0.41 mm/month. This rate was comparable with that observed in the present study. Yamada et al.20 reported a duration of 8.4 months and a rate of 0.33 mm/month.
In this study, mean maxillary 1st molar rotation was -0.86 ± 4.6° and -0.35 ± 4.1° in the right and left sides respectively. This amount of rotation was neither statistically nor clinically significant. Nalcaci et al.1 reported 0.54° and 0.74° rotation in the right and left sides respectively. Buccal movement of molars was evident in the current study, with a mean increase of 2.9 ± 1.8 mm in intermolar width. Many studies1112224 reported buccal movement of molars, while Yamada et al.,20 and Lai et al.,26 reported palatal movement of molars.
TPAs made up of 0.8 mm round stainless steel wire do not have enough strength to resist expansion due to distal traction force. Intrusion was the hallmark of this appliance, and numerous authors reported intrusion of molars in their studies.1222425 In a study similar to the current study, maxillary molars were intruded by an average of 0.3 ± 0.8 mm.1 On the other hand, Yamada et al.20 and Lai et al.26 reported extrusion of molars. In the majority of our cases, the line of action of force passed through the furcation and the center of resistance of molars in an apical direction, thus molars were intruded.
The vertical movement of molars was measured via 3D models. These measurements were based on the interocclusal space between maxillary and mandibular molars. Concomitant intrusion of 2nd molars and premolars could be masked by mandibular overclosure, if present at all. So, we did not measure absolute intrusion via this type of measurement, instead interocclusal discrepancy was measured. It is probable that a degree of underestimation occurred. The absolute measurement of intrusion is more accurately achieved via CBCT before and after distalization. However, a second CBCT was not approved by the relevant Research Ethics Committee.
Two miniscrews of 1.4 × 8.0 mm inserted in the same patient failed in the current study. They were found to be loose at the first visit after fitting. Larger miniscrews (2.0 × 10.0 mm) were then inserted in this patient, but these also became loose so the patient was removed from the study. Among the remaining patients, 3 screws (5.7%) became loose. In these cases, second screws were inserted successfully during their next visit. Excessive contact between the TPA and the miniscrew was the probable cause of screw failure in these cases.
References
1. Nalcaci R, Bicakci AA, Ozan F. Noncompliance screw supported maxillary molar distalization in a parallel manner. Korean J Orthod. 2010; 40:250–259.

2. Choi YJ, Lee JS, Cha JY, Park YC. Total distalization of the maxillary arch in a patient with skeletal Class II malocclusion. Am J Orthod Dentofacial Orthop. 2011; 139:823–833. PMID: 21640890.

3. Choi NC, Park YC, Lee HA, Lee KJ. Treatment of Class II protrusion with severe crowding using indirect miniscrew anchorage. Angle Orthod. 2007; 77:1109–1118. PMID: 18004931.

4. Grec RH, Janson G, Branco NC, Moura-Grec PG, Patel MP, Castanha Henriques JF. Intraoral distalizer effects with conventional and skeletal anchorage: a meta-analysis. Am J Orthod Dentofacial Orthop. 2013; 143:602–615. PMID: 23631962.

5. Sugawara J, Kanzaki R, Takahashi I, Nagasaka H, Nanda R. Distal movement of maxillary molars in nongrowing patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop. 2006; 129:723–733. PMID: 16769490.

6. Kinzinger GS, Eren M, Diedrich PR. Treatment effects of intraoral appliances with conventional anchorage designs for non-compliance maxillary molar distalization: a literature review. Eur J Orthod. 2008; 30:558–571. PMID: 18820306.

7. Sodagar A, Ahmad Akhoundi MS, Rafighii A, Arab S. Fabrication and evaluation of a noncompliant molar distalizing appliance: bonded molar distalizer. J Dent (Tehran). 2011; 8:107–116. PMID: 22457837.
8. McSherry PF, Bradley H. Class II correction-reducing patient compliance: a review of the available techniques. J Orthod. 2000; 27:219–225. PMID: 11099554.

9. Mavropoulos A, Karamouzos A, Kiliaridis S, Papadopoulos MA. Efficiency of noncompliance simultaneous first and second upper molar distalization: a three-dimensional tooth movement analysis. Angle Orthod. 2005; 75:532–539. PMID: 16097221.
10. Gelgör IE, Büyükyilmaz T, Karaman AI, Dolanmaz D, Kalayci A. Intraosseous screw-supported upper molar distalization. Angle Orthod. 2004; 74:838–850. PMID: 15673149.
11. Cornelis MA, De Clerck HJ. Maxillary molar distalization with miniplates assessed on digital models: a prospective clinical trial. Am J Orthod Dentofacial Orthop. 2007; 132:373–377. PMID: 17826606.

12. Gelgor IE, Karaman AI, Buyukyilmaz T. Comparison of 2 distalization systems supported by intraosseous screws. Am J Orthod Dentofacial Orthop. 2007; 131:161.e1–161.e8. PMID: 17276855.

13. Kuroda S, Yamada K, Deguchi T, Kyung HM, Takano-Yamamoto T. Class II malocclusion treated with miniscrew anchorage: comparison with traditional orthodontic mechanics outcomes. Am J Orthod Dentofacial Orthop. 2009; 135:302–309. PMID: 19268827.

14. Park HS, Lee SK, Kwon OW. Group distal movement of teeth using microscrew implant anchorage. Angle Orthod. 2005; 75:602–609. PMID: 16097229.
15. Blaya MG, Blaya DS, Guimaraes MB, Hirakata LM, Marquezan M. Patient's perception on mini-screws used for molar distalization. Rev Odonto Ciênc. 2010; 25:266–270.
16. Park HS, Kwon TG, Sung JH. Nonextraction treatment with microscrew implants. Angle Orthod. 2004; 74:539–549. PMID: 15387034.
17. Goyal A, Shivalinga B, Jyothikiran H, Patel V. Mini-implant supported molar distalization. J Dent Implant. 2013; 2:136–140.

18. Villela HM, Santos Sampaio AL, Bezerra F. Use of orthodontic miniscrews in asymmetrical corrections. Dental Press J Orthod. 2008; 13:107–117.
19. Kang YG, Kim JY, Nam JH. Control of maxillary dentition with 2 midpalatal orthodontic miniscrews. Am J Orthod Dentofacial Orthop. 2011; 140:879–885. PMID: 22133954.

20. Yamada K, Kuroda S, Deguchi T, Takano-Yamamoto T, Yamashiro T. Distal movement of maxillary molars using miniscrew anchorage in the buccal interradicular region. Angle Orthod. 2009; 79:78–84. PMID: 19123698.

21. Graber LW, Vanarsdall RL, Vig K. Orthodontics, current principles and techniques biomechanical considerations with temporary anchorage devices. 5th ed. Philadelphia, PA: Mosby;2012. p. 381–420.
22. Oberti G, Villegas C, Ealo M, Palacio JC, Baccetti T. Maxillary molar distalization with the dual-force distalizer supported by mini-implants: a clinical study. Am J Orthod Dentofacial Orthop. 2009; 135:282.e1–282.e5. discussion 282-3PMID: 19268824.

23. Almeida MA, Phillips C, Kula K, Tulloch C. Stability of the palatal rugae as landmarks for analysis of dental casts. Angle Orthod. 1995; 65:43–48. PMID: 7726462.
24. Kircelli BH, Pektaş ZO, Kircelli C. Maxillary molar distalization with a bone-anchored pendulum appliance. Angle Orthod. 2006; 76:650–659. PMID: 16808573.
25. Escobar SA, Tellez PA, Moncada CA, Villegas CA, Latorre CM, Oberti G. Distalization of maxillary molars with the bone-supported pendulum: a clinical study. Am J Orthod Dentofacial Orthop. 2007; 131:545–549. PMID: 17418723.

26. Lai EH, Yao CC, Chang JZ, Chen I, Chen YJ. Three-dimensional dental model analysis of treatment outcomes for protrusive maxillary dentition: comparison of headgear, miniscrew, and miniplate skeletal anchorage. Am J Orthod Dentofacial Orthop. 2008; 134:636–645. PMID: 18984395.

27. Polat-Ozsoy O, Kircelli BH, Arman-Ozçirpici A, Pektaş ZO, Uçkan S. Pendulum appliances with 2 anchorage designs: conventional anchorage vs bone anchorage. Am J Orthod Dentofacial Orthop. 2008; 133:339.e9–339.e17. PMID: 18331928.

28. Sar C, Kaya B, Ozsoy O, Özcirpici AA. Comparison of two implant-supported molar distalization systems. Angle Orthod. 2013; 83:460–467. PMID: 23106546.

29. Hoggan BR, Sadowsky C. The use of palatal rugae for the assessment of anteroposterior tooth movements. Am J Orthod Dentofacial Orthop. 2001; 119:482–488. PMID: 11343019.

Figure 1
Mini-implant-aided trans palatal arch molar distalizing appliances include a horseshoe shaped palatal bar inserted in the palatal sheath, and two miniscrews between the 1st molar and 2nd premolar. They exert a traction force from the anterior helix to the miniscrews. A, Before the start of treatment; B, after the completion of distalization.

Figure 2
The measurements on digital models. A, Distance between mesiopalatal cusps of both side first molars and incisive papilla; B, angle between the lines connecting incisive papilla to distopalatal cusp of the first molar and mesiopalatal cusp to distopalatal cusp of the first molar.
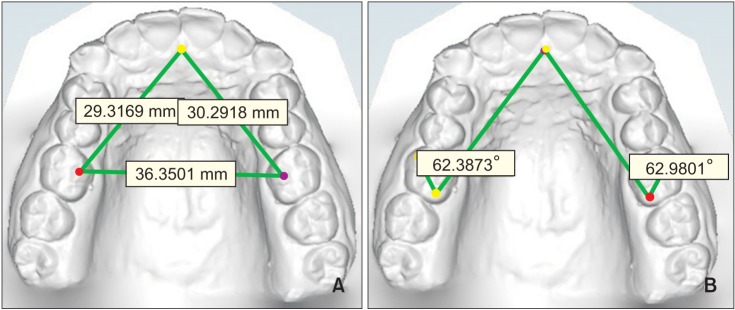
Figure 3
Evaluation methods of vertical teeth movement by three-dimensional digital model. A, Before treatment; B, after treatment. The red areas are contact areas, which are more marked on the right first maxillary molars before treatment than after treatment. Red marks are stronger on premolars and second molars after treatment, which is an additional sign of first molar intrusion.
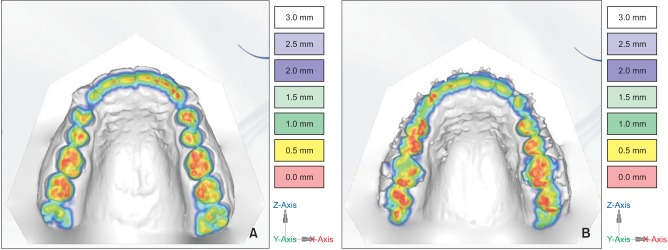
Figure 4
Demonstrations of the lines of traction force by cone-beam computed tomography (CBCT) images. A, Right sagittal view; B, left sagittal biew; C, coronal view. In right and left sagittal views of the CBCT scan, the angle between the lines of traction from the helix to the minscrews relative to the occlusal plane clearly indicate the apical direction of distal driving force. The coronal view shows the divergent distal driving force as the expansion component of applied force.
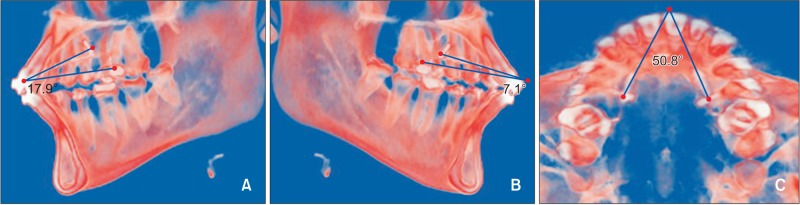
Figure 5
The sequence of changes in dentition. A, Before treatment; B, at the start of appliance placement and leveling; C, after the completion of distalization, and D, after debonding.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download