Abstract
Maxillary protraction is the conventional treatment for growing Class III patients with maxillary deficiency, but it has undesirable dental effects. The purpose of this report is to introduce an alternative modality of maxillary protraction in patients with dentoskeletal Class III malocclusion using a modified C-palatal plate connected with elastics to a face mask. This method improved skeletal measurements, corrected overjet, and slightly improved the profile. The patients may require definitive treatment in adolescence or adulthood. The modified C-palatal plate enables nonsurgical maxillary advancement with maximal skeletal effects and minimal dental side effects.
Maxillary protraction with a tooth-borne appliance and face mask is the conventional treatment in growing patients with Class III malocclusion caused by maxillary deficiency. However, it results in forward displacement of the maxilla, extrusion of maxillary molars, and clockwise rotation of the mandible.1234 Several methods overcoming these drawbacks by skeletal anchorage have been reported.567 However, miniplate placement in the infrazygomatic crest and lateral nasal wall areas is an aggressive procedure as two surgical sites are required.89
Several studies have evaluated the suitability of the palate as a skeletal anchorage site in the mixed dentition period.101112 Favero et al.13 placed miniscrews in the palate of a patient with deciduous dentition for maxillary protraction. Further, Ludwig et al.14 used hybrid tooth- and bone-borne rapid palatal expanders for protraction in adolescents. Recently, Kook et al.1516 placed palatal plates for molar distalization in adolescents with almost no side effects on the palatal soft tissue. The palatal approach is more desirable than surgery for placing infrazygomatic crest miniplates because it involves a flapless procedure with a single plate that works bilaterally.
The purpose of this report is to introduce an alternative modality of maxillary protraction in growing patients with dentoskeletal Class III malocclusion using a modified C-palatal plate and face mask.
The appliance consists of a palatal miniplate with three hooks on each arm (0.8 mm thick, 2.0 mm wide, and 28.0 mm long). The plate is fixed to the palate with three miniscrews (diameter, 2.0 mm; length, 8.0 mm), driven into screw tubes 2 mm apart from the midpalatal suture (Figure 1A).
A silicone jig is used during placement to guarantee a consistent distance between the plate arms and the palatal tissues. The plate is adapted to the contours of the cast with the arms extending to the gingival level in the canine areas while maintaining approximately 2 mm of space between the arms and the palatal surface. The fabrication of the jig has been described previously (Figure 1B).16
After administration of local anesthesia, the jig-plate assembly is placed on the palate guided by the occlusal surfaces of the jig. Three self-drilling miniscrews are installed with a torque driver (Jeil Medical Corporation, Seoul, Korea) at 30 rpm using less than 30 N·cm; then, the jig is removed and the miniscrews are tightened. The palatal plate functions as the point of force application and the face mask serves as extraoral anchorage.
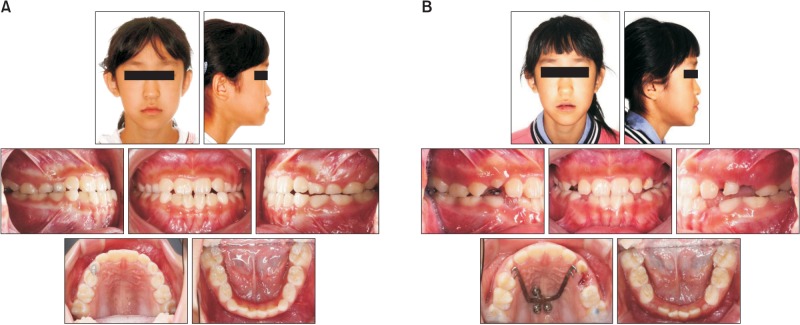
A female patient aged 9 years 8 months visited the clinic with the chief complaint of cross bite. She had a hyperdivergent growth pattern. Intraoral examination revealed early mixed dentition and Class III molar and canine relationships with anterior cross bite (Figure 2A).
To correct the cross bite, a C-palatal plate with hooks in the deciduous canine area was placed with the aid of a silicone jig. Elastics were connected to a face mask at approximately 20° downward to the occlusal plane for 14 hours daily to deliver a force of 500 g per side.
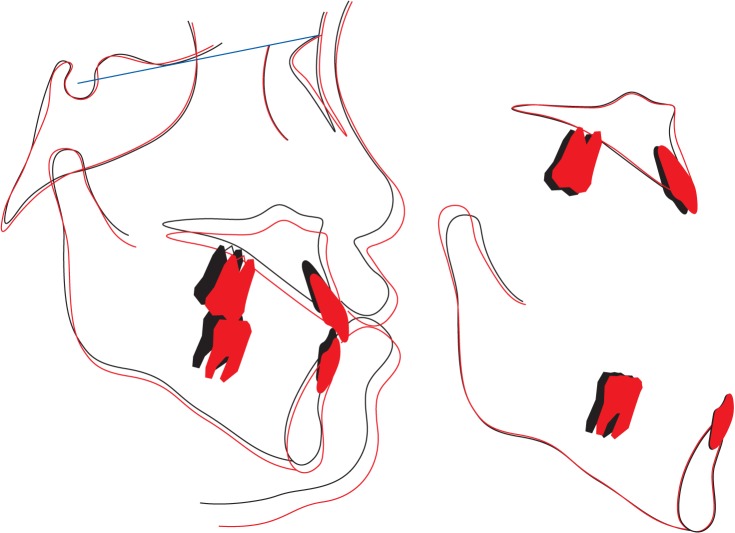
This treatment successfully corrected the cross bite. A point as well as the maxillary molars were displaced anteroinferiorly, and the posterior nasal spine (PNS) showed downward movement. Cephalometric superimposition show improvement of the skeletal Class III relationship (Figures 2B, 3, and 4; Table 1). The total treatment time was 18 months, and the patient and her parents were satisfied with the profile.
The application of skeletal anchorage is a viable modality to correct skeletal Class III malocclusion in growing patients. Temporary skeletal anchorage devices are placed in the palate because of the ease of access, reduced susceptibility to inflammation, and good quantity of bone in the area.17
A palatal plate can be used as the point of force application to overcome dental side effects and maximize the skeletal gain of maxillary protraction. When compared with the aggressive surgical procedures required for miniplate placement in the infrazygomatic crest area, a palatal plate can be safely and easily placed by clinicians. Kim et al.18 evaluated stress distribution by three-dimensional finite element analysis of maxillary protraction with a palatal plate: they stated that the palatal approach is more efficient than traction from miniscrews placed buccally in the infrazygomatic area and reported forward displacement with counterclockwise rotation of the maxillofacial complex.
In agreement, our patient showed anteroinferior displacement of A point with further downward movement of the PNS, resulting in earlier contact between the posterior teeth and clockwise rotation of the mandible. This outcome may be explained by the lower point of force application to the center of resistance of the maxilla in the proposed method than in the buccal and conventional approaches. The profile improved because of the combination of forward maxillary displacement and clockwise mandibular rotation, causing backward displacement of the chin. Further studies are recommended to evaluate the effectiveness of this treatment, especially by three-dimensional assessment using conebeam computed tomography (CBCT).
In a meta-analysis, Feng et al.19 showed that bone-anchored miniplates might result in maxillary advancement as well as reduction of mandibular rotation, extrusion of maxillary molars, and proclination of maxillary incisors. In addition, placement of a bonded transpalatal arch between maxillary first molars is recommended to decrease extrusion of maxillary posterior teeth, especially in patients with the hyperdivergent facial type.
Recently, Nienkemper et al.20 demonstrated a 1.9 mm of forward movement of the maxilla using a bone-tooth-borne hybrid hyrax-facemask appliance in children with dentoskeletal Class III malocclusion. In addition, Nguyen et al.21 reported 3.7 mm forward displacement of the maxilla using an intraoral skeletal anchorage appliance by three-dimensional superimposition of CBCT-derived models. In our case, the maxilla was displaced forward by 1.5 mm. The difference in the amount of displacement might be primarily due to the aggressive protraction method in the previous study; it required surgical placement of four miniplates, two in the infrazygomatic crests and two between the mandibular lateral incisors and canines. Other reasons could be the differences between the evaluation methods and individual and ethnic variations of the patients. In our patient, the overjet was corrected and the profile slightly improved. However, these changes might have been supported by normal growth of the maxilla during the long treatment (18 months). Therefore, the treatment effect might be smaller than 1.5 mm. The improvements due to growth and the treatment are not exactly distinguishable. In addition, some relapse of the corrected overjet is expected because of the chin cup effect of the face mask. Therefore, a second therapeutic phase may be necessary for definitive correction. Moreover, the shape and depth of the palatal vault might have played a role in determining the relationship between the center of resistance and the force vector. A further study is warranted to evaluate the influence of different palatal vault configurations on the effects of a protraction palatal plate and growth.
Despite its advantages, a palatal plate might cause inflammation of the palatal mucosal and speech disturbance from decreased tongue space. Therefore, several measures were taken to decrease the probability of inflammation, including the addition of screw tubes and accurate placement of the plate with a jig. The effect on speech has been evaluated using a different design: the previous study showed that the impact on speech articulation is reversible within two weeks due to high adaptability of the tongue.22
In conclusion, application of a modified C-palatal plate and face mask seems to be a suitable modality of maxillary protraction due to its maximal skeletal effects, minimal dental side effects, and nonsurgical approach. However, this appliance is not suitable for patients with maxillary transverse deficiency because it prevents opening of the midpalatal suture.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Ki Beom Kim for invaluable advice on the construction of the appliance and Dr. Chee Soo Ahn for assisting in manuscript preparation.
Notes
References
1. Baik HS. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995; 108:583–592. PMID: 7503035.

2. Gallagher RW, Miranda F, Buschang PH. Maxillary protraction: treatment and posttreatment effects. Am J Orthod Dentofacial Orthop. 1998; 113:612–619. PMID: 9637563.
3. Kama JD, Ozer T, Baran S. Orthodontic and orthopaedic changes associated with treatment in subjects with Class III malocclusions. Eur J Orthod. 2006; 28:496–502. PMID: 16772318.

4. Kim JH, Viana MA, Graber TM, Omerza FF, BeGole EA. The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial Orthop. 1999; 115:675–685. PMID: 10358251.

5. Smalley WM, Shapiro PA, Hohl TH, Kokich VG, Brånemark PI. Osseointegrated titanium implants for maxillofacial protraction in monkeys. Am J Orthod Dentofacial Orthop. 1988; 94:285–295. PMID: 3177282.

6. Singer SL, Henry PJ, Rosenberg I. Osseointegrated implants as an adjunct to facemask therapy: a case report. Angle Orthod. 2000; 70:253–262. PMID: 10926436.
7. Enacar A, Giray B, Pehlivanoglu M, Iplikcioglu H. Facemask therapy with rigid anchorage in a patient with maxillary hypoplasia and severe oligodontia. Am J Orthod Dentofacial Orthop. 2003; 123:571–577. PMID: 12750679.

8. Cha BK, Choi DS, Ngan P, Jost-Brinkmann PG, Kim SM, Jang IS. Maxillary protraction with miniplates providing skeletal anchorage in a growing Class III patient. Am J Orthod Dentofacial Orthop. 2011; 139:99–112. PMID: 21195283.

9. Kaya D, Kocadereli I, Kan B, Tasar F. Effects of facemask treatment anchored with miniplates after alternate rapid maxillary expansions and constrictions; a pilot study. Angle Orthod. 2011; 81:639–646. PMID: 21299407.

10. Han S, Bayome M, Lee J, Lee YJ, Song HH, Kook YA. Evaluation of palatal bone density in adults and adolescents for application of skeletal anchorage devices. Angle Orthod. 2012; 82:625–631. PMID: 22077190.

11. Lee SM, Park JH, Bayome M, Kim HS, Mo SS, Kook YA. Palatal soft tissue thickness at different ages using an ultrasonic device. J Clin Pediatr Dent. 2012; 36:405–409. PMID: 23019841.

12. Ryu JH, Park JH, Vu Thi, Bayome M, Kim Y, Kook YA. Palatal bone thickness compared with cone-beam computed tomography in adolescents and adults for mini-implant placement. Am J Orthod Dentofacial Orthop. 2012; 142:207–212. PMID: 22858330.

13. Favero L, Winkler A, Favero V. Non-compliant maxillary protraction by orthodontic micro-implants. Eur J Paediatr Dent. 2012; 13:244–248. PMID: 22971266.
14. Ludwig B, Glas B, Bowman SJ, Drescher D, Wilmes B. Miniscrew-supported Class III treatment with the Hybrid RPE Advancer. J Clin Orthod. 2010; 44:533–539. PMID: 21280544.
15. Kook YA, Kim SH, Chung KR. A modified palatal anchorage plate for simple and efficient distalization. J Clin Orthod. 2010; 44:719–730. PMID: 21591548.
16. Kook YA, Lee DH, Kim SH, Chung KR. Design improvements in the modified C-palatal plate for molar distalization. J Clin Orthod. 2013; 47:241–248. PMID: 23660818.
17. Lee J, Miyazawa K, Tabuchi M, Sato T, Kawaguchi M, Goto S. Effectiveness of en-masse retraction using midpalatal miniscrews and a modified transpalatal arch: Treatment duration and dentoskeletal changes. Korean J Orthod. 2014; 44:88–95. PMID: 24696825.
18. Kim KY, Bayome M, Park JH, Kim KB, Mo SS, Kook YA. Displacement and stress distribution of the maxillofacial complex during maxillary protraction with buccal versus palatal plates: finite element analysis. Eur J Orthod. 2015; 37:275–283. PMID: 25090997.

19. Feng X, Li J, Li Y, Zhao Z, Zhao S, Wang J. Effectiveness of TAD-anchored maxillary protraction in late mixed dentition. Angle Orthod. 2012; 82:1107–1114. PMID: 22458766.

20. Nienkemper M, Wilmes B, Franchi L, Drescher D. Effectiveness of maxillary protraction using a hybrid hyrax-facemask combination: A controlled clinical study. Angle Orthod. 2014; [Epub ahead of print].

21. Nguyen T, Cevidanes L, Cornelis MA, Heymann G, de Paula LK, De Clerck H. Three-dimensional assessment of maxillary changes associated with bone anchored maxillary protraction. Am J Orthod Dentofacial Orthop. 2011; 140:790–798. PMID: 22133943.

22. Joo MC. Evaluation of Palatal Plate Effects on the speech Articulation using acoustic analysis Dentistry [MSD dissertation]. Seoul: The Catholic University of Korea;2012.
Figure 1
Placement of the modified C-palatal plate. A, the plate fixed on the palate; B, the jig-plate assembly; C, the plate connected to the face mask via elastics.
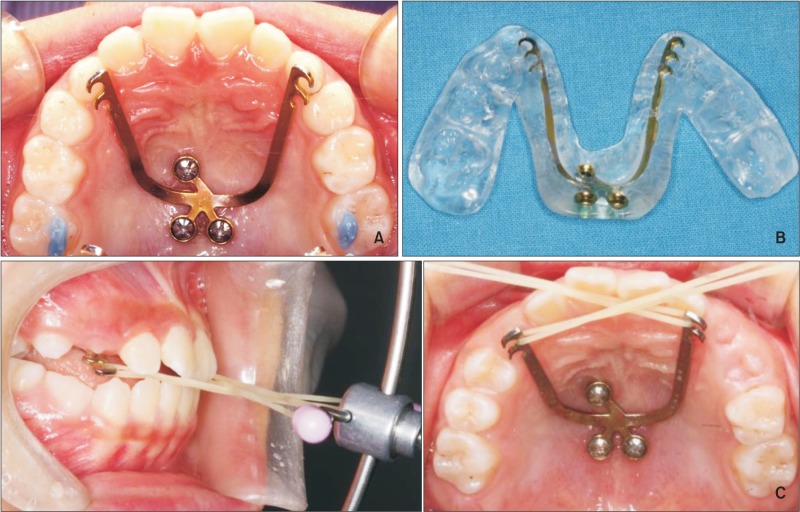
Figure 3
Pretreatment (A) and post-treatment (B) lateral cephalometric radiographs derived from cone-beam computed tomography images.

Table 1
Cephalometric measurements
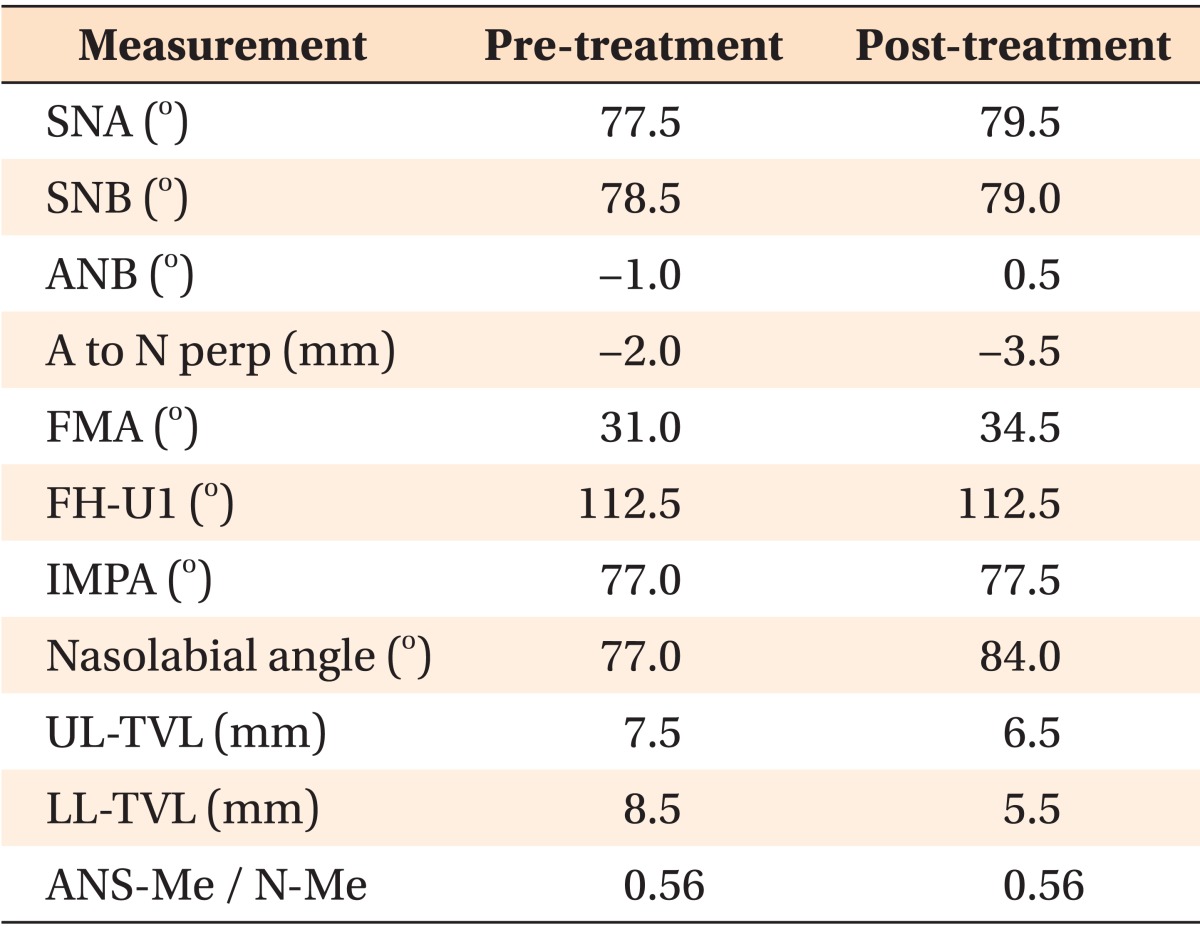
SNA, Sella-Nasion-A point angle; SNB, Sella-Nasion-B point angle; ANB, A point-Nasion-B point angle; FMA, Frankfurt mandibular plane angle; FH-U1, Frankfurt horizontal plane to upper incisor angle; IMPA, lower incisor to mandibular plane angle; UL-TVL, upper lip to true vertical line distance; LL-TVL, lower lip to true vertical line distance; ANS-Me/N-Me, anterior nasal spine to menton distance and nasion to menton distance ratio.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download