INTRODUCTION
In general, orthognathic surgery is preceded by presurgical orthodontic treatment such as dental alignment, dental decompensation, and arch coordination to determine the prognosis, treatment plan, and safety of the surgical procedure.
1,
2 However, orthodontic treatment prior to orthognathic surgery has disadvantages such as discomfort in mastication for the duration of the treatment and deterioration in facial form due to dental decompensation.
To overcome the disadvantages of presurgical orthodontic treatment, recent studies have reported orthognathic surgery methods that precede orthodontic treatment or shorten its duration.
3,
4,
5,
6,
7,
8,
9,
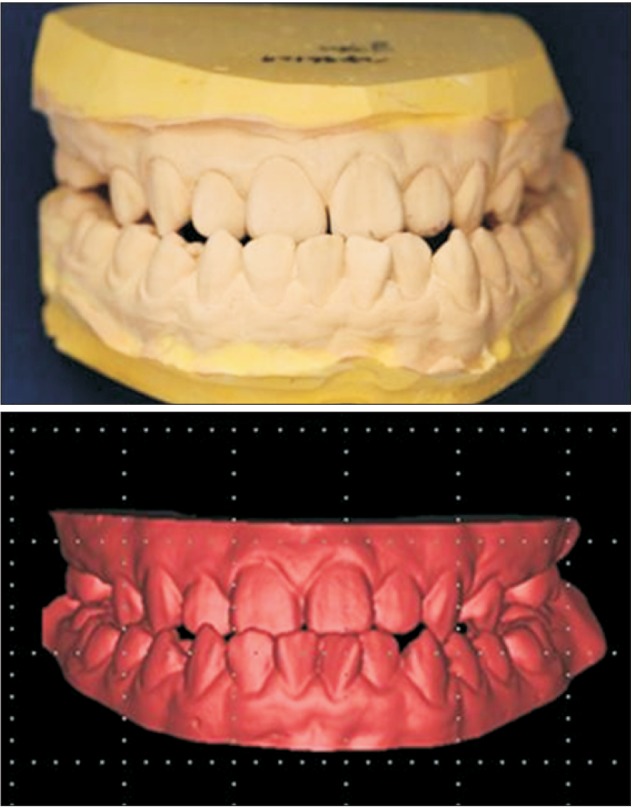
10 In the surgeryfirst approach, dental alignment is evaluated based on a cast model set up, a surgical procedure is outlined based on the degree of movement of the maxilla and mandible, and model surgery is performed to produce a surgical wafer.
3 However, the surgery-first approach has a tendency toward high error rates as it involves an extra remounting step that can increase the chance of error.
11 Recently, the development of a three-dimensional (3D) rapid prototyping technique has enabled a 3D virtual setup,
12 3D surgical simulation,
13 and the production of a surgical wafer,
14 which may reduce the chance of errors by eliminating the need for laboratory procedures such as mounting. Combining the 3D technique with the surgery-first approach is expected to result in more accurate and predictable diagnoses, treatment plans, and outcomes.
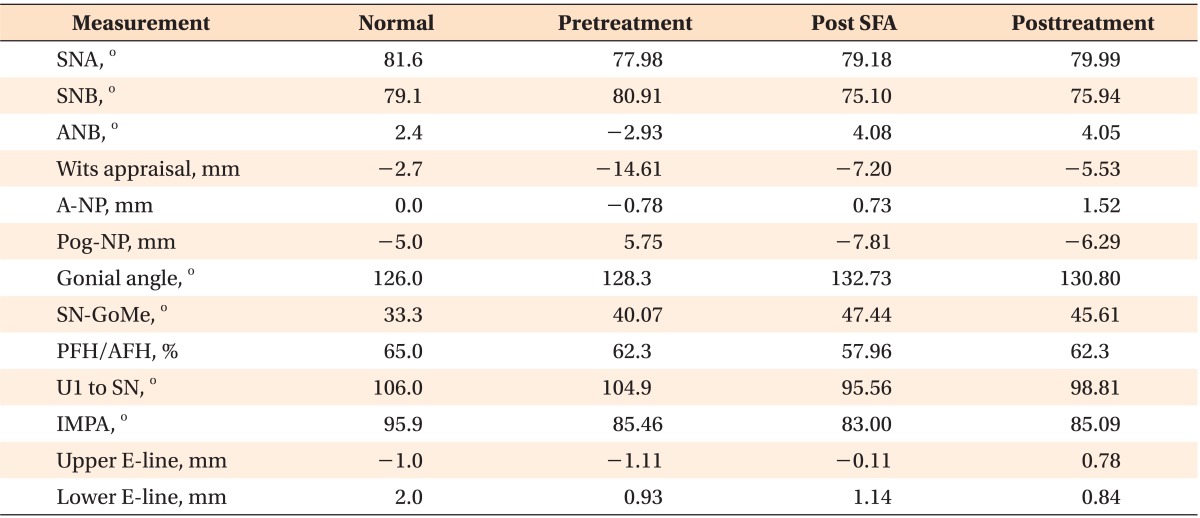
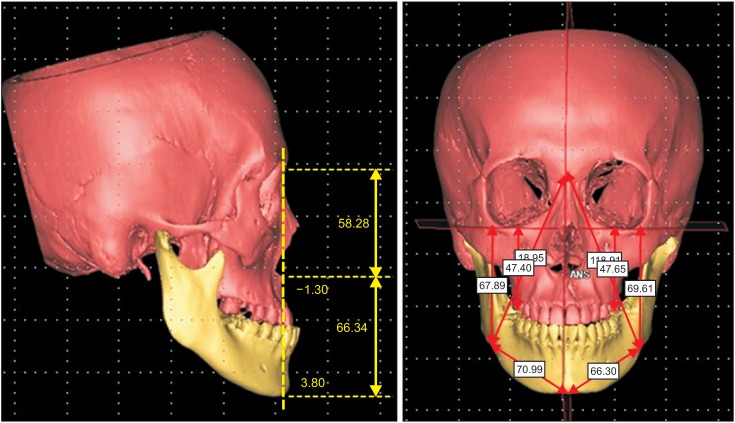
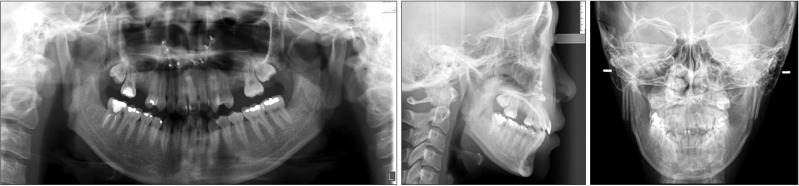
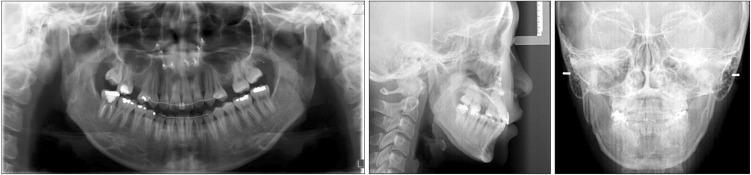
The authors report a case of skeletal Class III malocclusion. The diagnosis and treatment plan were carried out through a 3D virtual setup and 3D surgical simulation, and a surgical wafer was produced using the stereolithography technique. Thus, the surgery-first approach was incorporated into the treatment process without presurgical orthodontic treatment, and a favorable treatment outcome was eventually achieved.
Go to :

TREATMENT ALTERNATIVES
The first treatment option was orthodontic treatment with orthognathic surgery, which involves arch coordination, dental decompensation, and resolution of crowding through the conventional method of presurgical orthodontic treatment followed by postsurgical orthodontic treatment. The second treatment option was the surgery-first approach, which involves orthognathic surgery followed by postsurgical orthodontic treatment. The third treatment option was camouflage, which involves extraction of the mandibular first premolar. Camouflage would resolve the patient's chief complaint of anterior crossbite, but it would result in no improvement in facial form and worsening of the lingual inclination of the mandibular anterior teeth.
In this patient, the surgery-first approach was chosen, as the patient desired fast resolution and improvement of the facial form; in addition, occlusion was stable enough for the surgery-first approach, horizontal and vertical disharmony was low, and additional tooth extraction was not indicated.
Go to :

DISCUSSION
The patient described herein had skeletal Class III malocclusion, and the diagnosis and treatment plan were established through a 3D virtual setup and 3D surgical simulation. The surgical wafer was produced using the stereolithography technique, and the treatment was carried out using the surgery-first approach.
Recently, a number of reports regarding surgical orthodontic treatment without preoperative orthodontic treatment (
i.e., the surgery-first approach) have been published.
3,
7,
8,
9,
15,
16
The advantages of the surgery-first approach are as follows: high patient satisfaction due to immediate improvement of facial profile at the beginning of the treatment,
3,
6,
7,
16 shorter duration of treatment
3,
7,
15 due to rapid tooth movement,
17,
18,
19 and the possibility of physiologic decompensation
3,
6,
7 through facilitation of the soft tissue as a result of improvement in the maxillary and mandibular discrepancy.
However, the surgery-first approach has the following disadvantages: the inability to use presurgical occlusion as a guide, difficulty in obtaining stable occlusion after surgery,
7 and need of a clinician's experience for the exact prediction of tooth movement in presurgical orthodontic treatment and the exact prediction of the approach notwithstanding structural discrepancies.
3 Therefore, the surgery-first approach is mainly chosen when there are at least 3 stable occlusal contact points, a minor curve of speed and vertical problem, minor or no transverse discrepancy, and when there is no indication for extraction.
3,
6
To achieve predictable results in orthognathic surgery, the following factors must be considered: 1) the exact diagnosis, 2) accuracy of laboratory procedures in the model surgery and production of surgical tools, and 3) skill of the oral and maxillofacial surgeon. To reduce errors in the process of establishing the diagnosis and treatment plan, recent studies have been conducted using the 3D virtual technique.
20,
21
The development of computer-aided surgery has facilitated a reduction in the duration of presurgical orthodontic treatment. Kang et al.
10 reported the results of orthognathic surgery with reduced duration of presurgical orthodontic treatment. After 3D analysis, the occlusion of the final surgical wafer was determined, followed by superimposition of the current occlusion status. Then, the surgery plan was finalized through 3D virtual surgery, and the entire process of making the surgical wafer was carried out on a computer. Cevidanes et al.
13 reported that computer-aided surgery could make the elaboration of the surgical plan a more flexible process, increase the plan's level of detail and accuracy, yield higher operative precision and control, and enhance documentation of cases.
With the surgery-first approach, the surgical plan is finalized prior to presurgical orthodontic treatment, which requires much effort to ensure a predictable result; a set method has not been established, although various studies have reported this approach. Nagasaka et al.
7 established a plan for the surgery-first approach through a cephalometric radiograph and occlusogram. Villegas et al.
16 and Liou et al.
6 established a surgical plan through model surgery using an initial cast model.
However, if the surgery-first approach is followed without the cast model setup, the range and degree of predictions would increase, which can lead to a reduction in accuracy. Baek et al.
3 established a surgical plan that included the cast model setup process for the prediction and simulation of dentition, decompensation of the whole dentition, and arch coordination. To achieve a more accurate surgical plan in the laboratory, the patient's occlusal status is transferred to a semi-adjustable articulator. Then, the cast model setup that predicts the presurgical orthodontic treatment is initiated, and this becomes the reference for the model surgery to be carried out. Based on the confirmed surgical plan, the cast model setup is replaced by the initial preoperative cast model to produce the intermediate and final surgical wafers.
Sharifi et al.
11 reported the occurrence of errors when the facebow is transferred and the cast is mounted during model planning for orthognathic surgery; the possibility for errors increases even further during substitution of the final setup cast model for the initial preoperative cast model. These errors in laboratory procedures can be overcome by using the 3D virtual technique. The possibility of errors associated with 2D diagnosis can be reduced and a more accurate diagnosis can be facilitated through 3D analysis of the recomposed 3D CT image.
14,
20,
22
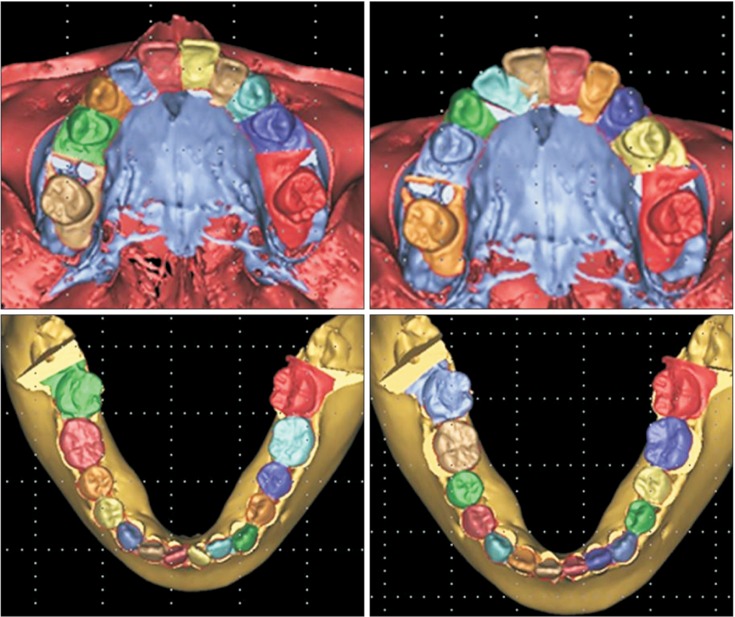
In our case, to obtain predictable results and to reduce errors during the establishment of a diagnosis and treatment plan, 3D diagnosis, 3D digital model setup, and 3D virtual surgery were used, which were facilitated by the initial patient data. For the utilization of the reconstructed CT image, the steps of facebow transfer and articular mounting to transfer the position of the maxilla and mandible to the cranial base were omitted, thereby decreasing the chance of error. The cast model setup to predict the presurgical orthodontic treatment also used 3D digital imaging,
12 and Mimics® 14.0 was used for the surgical simulation. Thus, an accurate treatment plan was established.
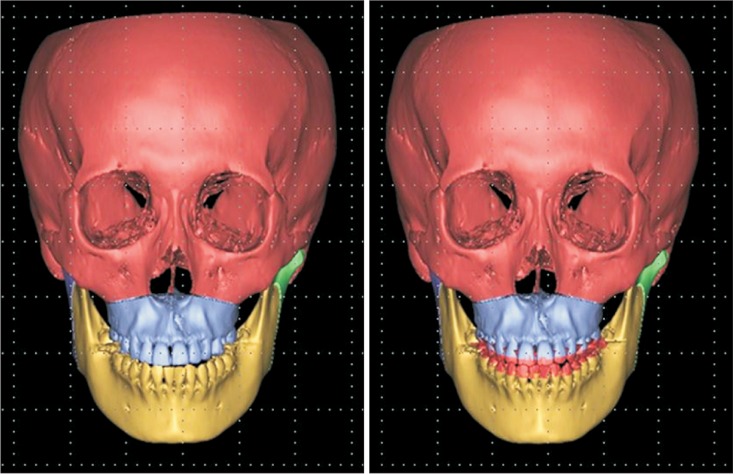
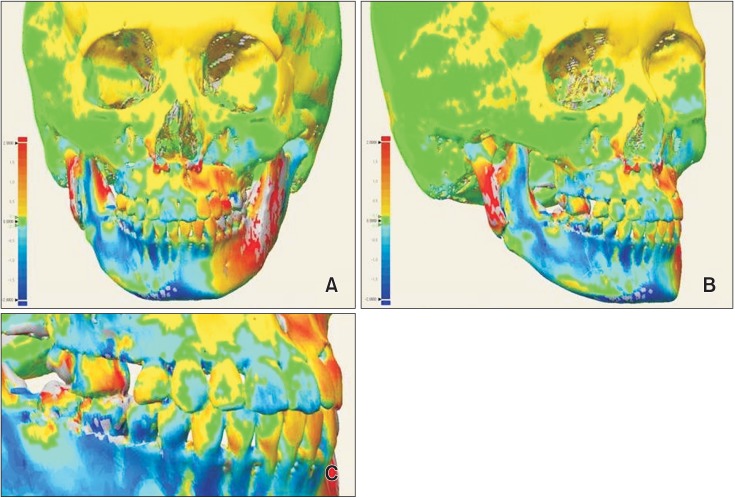
Consequently, no errors are encountered when the initial digital cast model is replaced by the intermediate and final wafer, because the use of 3D imaging software allows several 3D objects (virtual setup cast model and initial digital cast model) to be moved equally at the same time, and 3D objects can be exchanged with each other without replacement of the initial digital cast model by the virtual setup cast model by superimposition. In other words, the initial digital cast model can be substituted by the virtual setup cast model by moving the virtual setup cast model and initial digital cast model at the same time during the surgical simulation. The intermediate and final surgical wafers can also be produced through stereolithographic technology.
10,
23
Using 3D models, all of the procedures for diagnosis and wafer production in the model surgery can be simulated, intermediate assessment can be conducted, and the intermediate and final surgical wafers can be produced. Therefore, errors encountered during laboratory procedures can be minimized.
The cranium in the posttreatment CT images was used as a reference for superimposition of the simulated and posttreatment data, and results were acceptable after evaluation by a color-coded discrepancy map.
The only possibility for error would arise during the superimposition of the scanned initial digital cast model to the dentition of CT image. On the CT image, it is difficult to obtain the precise image because of artifacts on the dentition; therefore, an error can occur because of an unclear reference when the 3D digital cast model, which is transformed from the patient's initial cast model through the optical scanner, is superimposed onto the CT image.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print











 XML Download
XML Download