Abstract
Figures and Tables
 | Figure 1Design of the tongue elevator. Occlusal view (A) and lingual view (B) of a conventional tongue elevator. The acrylic base occupies the entire mouth floor except for the region that can disturb the movement of the lingual frenum. The occlusal rests are placed on the lingual occlusal grooves of the posterior teeth. In a modified tongue elevator (C and D), the volume and height of the resin part are reduced for tongue-tie. |
 | Figure 2Mechanism of the tongue elevator. Tongue position is elevated after application of the tongue elevator (cross-sectional view). Arrows indicate the pressure generated by altered tongue posture with the tongue elevator. |
 | Figure 5Lateral cephalograms. From the left, initial (A); post-treatment (B); 3-year post-treatment showing relapse tendency (C); 8-year follow-up with 4-year application of tongue elevator (D); and 10-year follow-up with 6-year application of tongue elevator, indicating correction of anterior open-bite and good stability (E). |
 | Figure 6Initial treatment mechanics for molar intrusion. Four C-tubes installed in the each posterior area with a transpalatal arch in the upper dentition, and a lingual arch in the lower arch. |
 | Figure 9Superimpositions of lateral cephalograms. A, Pretreatment (solid line) and post-treatment (dotted line); B, Post-treatment (solid line) and 3-year post-treatment (dotted line) images showing relapse tendency; C, 3-year post-treatment (solid line) and 8-year follow-up (dotted line) with 4-year application of tongue elevator; D, 8-year follow-up (solid line) and 10-year follow-up (dotted line) with 6-year application of tongue elevator, showing good retention. |
 | Figure 12Re-treatment with a tongue elevator. After relapse occurred, a tongue elevator was used in the lower arch (A and B), and a wrap-around removable retainer with occlusal rests and reduced resin plate was used in the upper arch (C and D); Frontal view of the tongue while wearing the tongue elevator (E and F). |
 | Figure 13Facial and intraoral photographs at 8-year follow-up with 4-year application of tongue elevator. |
 | Figure 14Facial and intraoral photographs at 10-year follow-up with 6-year application of tongue elevator. |
Table 1
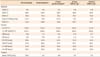
*Relapse; †4-year application of tongue elevator; ‡6-year application of tongue elevator.
ANB, A point-nasion-B point angle; SNA, sella-nasion-A point angle; SNB, sella-nasion-B point angle; Pog to N-Perp, distance of pogonion to the nasion-perpendicular line to Frankfurt horizontal plane; FMA, Frankfurt horizontal plane-mandibular plane angle; U1-FH, upper incisor-Frankfurt horizontal plane angle; L1-MP (IMPA), lower incisor-mandibular plane angle; OB, overbite; OJ, overjet; U1-PP, perpendicular distance of the maxillary incisor tip to the palatal plane; U6-PP, perpendicular distance of the mesial cusp tip of the maxillary first molar to the palatal plane; L1-MP, perpendicular distance of the mandibular incisor tip to the mandibular plane; L6-MP, perpendicular distance of the mesial cusp tip of the mandibular first molar to the mandibular plane; TPD, tongue-to-palate distance.
According to Ozbek et al.21, reference lines were drawn and eight different TPDs from the tongue tip were determined by measuring the distances between the points formed with the lines intersecting the dorsum of the tongue and the palatal curvature.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download