Abstract
An 8-years old boy with facial asymmetry and unilateral posterior crossbite on the left side received orthopedic and orthodontic treatment. During the first phase of treatment, the narrow maxillary arch was expanded using an acrylic plate. Then, the acrylic plate was used as a bite block with occlusal indentations from the construction bite that was obtained with the incisors in a coincident dental midline. After the position of the mandible was stabilized, the second phase of orthodontic treatment was initiated using fixed appliances for detailing of the occlusion. Skeletal symmetry, ideal occlusion, and coincident dental midlines were thus achieved. Functionally, occlusal force balance and masticatory muscle activity were improved, and the chewing patterns were normalized.
Facial asymmetry, a common occurrence in human beings,1 is affected by several etiologic, environmental, and genetic factors. Furthermore, posterior crossbite is one of the most prevalent malocclusions in primary and early mixed dentitions.2,3 Unilateral posterior crossbite commonly causes a functional shift of the mandible toward the crossbite side. Functional displacement of the mandible can cause craniomandibular asymmetry, particularly in growing patients, which becomes a permanent feature.4 This phenomenon may be attributed to an asymmetric function during mastication, which affects the balance in facial growth. To date, several authors have reported imbalanced muscle activity of the masticatory muscles and asymmetric bite forces in children with unilateral posterior crossbite.5,6 Early correction of unilateral posterior crossbite accompanying displacement of the mandible has been recommended,7,8,9 and many successfully treated cases have been reported.10 However, it remains unclear whether imbalanced masticatory functions in a patient with unilateral posterior crossbite can be corrected by early treatment.9
In this report, we present the orthopedic and orthodontic treatment of facial asymmetry and unilateral posterior crossbite in a growing patient. We evaluated the distribution of the occlusal force, electromyographic activity of the masticatory muscles, and chewing patterns before and after treatment.
An 8-years old boy was referred by the pedodontist for orthodontic evaluation. The chief complaint was posterior crossbite on the left side. He had mouth breathing and nail-biting habits, and his dental history was unremarkable.
On examination, he showed mild facial asymmetry with deviation of the mandible to the left side in habitual occlusion (Figure 1), but the facial asymmetry diminished during mouth opening. His facial profile was straight with a deep mentolabial fold. Intraoral examination revealed a mixed dentition, Class II molar relationships, narrow maxillary dental arch, and unilateral posterior crossbite on the left side. The maxillary dental midline coincided with the facial midline; however, the mandibular dental midline was deviated to the left by 4 mm due to the lateral shift of the mandible. The overjet was 5.2 mm, and overbite was 1.9 mm (Figure 2). He had no signs or symptoms of temporomandibular joint disorders.
A panoramic radiograph revealed no specific findings. Lateral cephalometric analysis showed a skeletal Class I relationship with a vertical growth pattern (Table 1). The posteroanterior cephalometric radiograph confirmed significant deviation of menton toward the crossbite side (Figure 3). On the basis of clinical and radiographic examination, the patient's facial asymmetry was considered a result of the posterior crossbite on the left side.
The treatment objectives were to expand the narrow maxillary arch, correct the posterior crossbite on the left side, guide symmetric growth of the mandible, and achieve a normal occlusion.
The treatment plan included two phases. The first phase involved orthopedic treatment to expand the maxillary arch and to lead the mandible to a more symmetric position. The second phase of treatment involved detailing of the occlusion with conventional fixed orthodontic appliances.
During the first phase of treatment a removable acrylic plate was fabricated, which was composed of an expansion screw, clasps on the first deciduous molars and the first molars, and bite blocks on the posterior teeth. The patient was instructed to wear the appliance full-time and to turn the screw two-quarter turns each week (Figure 4). After four months of treatment, 4.5 mm of transverse expansion was achieved, and the posterior crossbite was successfully corrected. Then, the acrylic plate was used as a bite block with occlusal indentations from a construction bite that was obtained with the incisors in a coincident dental midline (Figure 5). After another six months of treatment with the appliance, the mandible appeared to be at the new position; thereafter, for retention, the patient was instructed to wear the appliance night-time until the permanent dentition erupted (Figure 6). Thus, during the first phase of treatment, the patient wore the appliance full-time for 10 months and night-time for 14 months.
During the second phase of orthodontic treatment, fixed edgewise appliances with a 0.022- × 0.028-inch slot were placed in both the arches, and conventional orthodontic treatment was performed to eliminate minor spaces and to optimize the occlusion. After 15 months of fixed orthodontic treatment, the appliances were removed. Then, maxillary and mandibular retention was performed with bonded canine-to-canine fixed retainers.
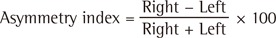
The intraoral photographs obtained after the first phase of treatment are presented in Figure 7. The dental midlines were coincident, and minor spaces between the maxillary and mandibular anterior teeth remained.
After the second phase of treatment, posttreatment examination revealed improved symmetry and a straight facial profile (Figure 8). Intraorally, a Class I molar relationship with optimal overbite and overjet was achieved. The dental midlines were coincident with each other and with the facial midline (Figure 8). The patient showed no clinical symptoms of temporomandibular disorders. Posttreatment panoramic radiographs showed closure of the minor spaces between the anterior teeth, acceptable root parallelism, and developing upper third molars (Figure 9). Cephalometric superimposition showed harmonious growth of the maxilla and mandible, and no significant changes in the skeletal relationship and in the position and inclination of the incisors (Figure 10 and Table 1). As shown in the posteroanterior radiograph and tracings of the submentovertex radiographs, deviation of the mandible and asymmetry in the long axis of the condyle decreased after treatment (Figures 9 and 11).
To evaluate the functional changes associated with correction of facial asymmetry and unilateral posterior crossbite, occlusal balance, muscle activity of the masticatory muscles, and chewing patterns were examined before treatment and after the second phase of treatment.
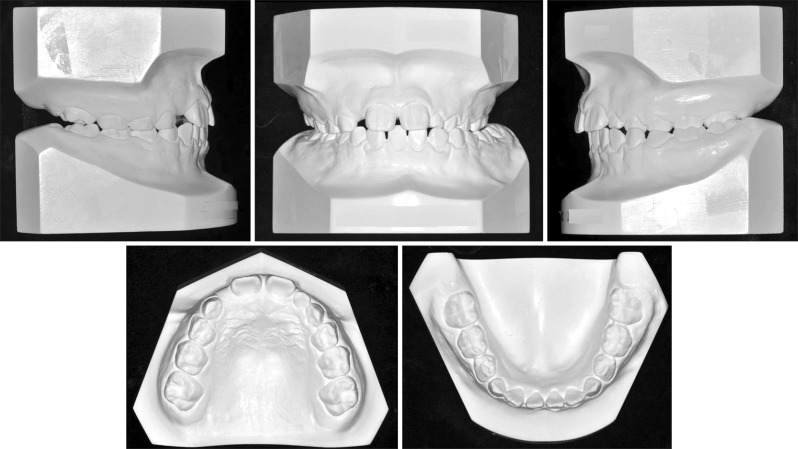
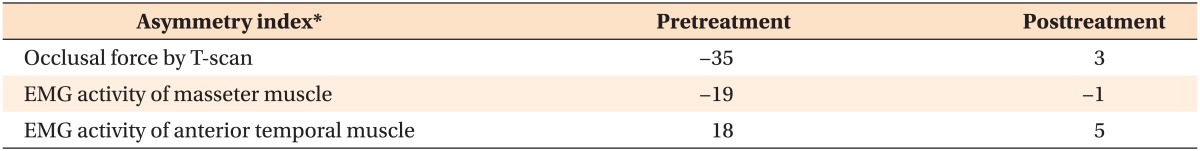
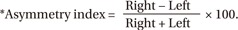
The occlusal contacts and distribution of the bite force in centric occlusion were estimated with the T-scan system (Tekscan Co., Boston, MA, USA), which showed the locations of tooth contact and their relative forces. The values obtained by multiplying the number of contact points and the value of the color scale from the load graph of T-scan were considered to be the occlusal forces on the right and left sides.11 To evaluate the distribution of the occlusal forces, the asymmetry index of occlusal force was calculated using the following formula.
A positive score of the index indicates superiority of the occlusal force on the right side, whereas a negative score indicates superiority on the left side, and zero indicates an even distribution of the occlusal force. In the patient described in this report, the occlusal force was higher on the left side than on the right side pretreatment (asymmetry index was -35), but the difference in occlusal forces between the right and left sides was reduced posttreatment (asymmetry index was 3; Figure 12 and Table 2).
Electromyographic (EMG) examinations were performed during clenching to record the activity of the masseter muscles and anterior temporal muscles before and after treatment with BioEMG-II (Bio-Research Associates Inc., Milwaukee, WI, USA). The asymmetry index of EMG was also calculated using the same formula. The asymmetry indices of EMG for the masseter muscles and anterior temporal muscles were -19 and 18 pretreatment and decreased to -1 and 5 posttreatment, respectively (Figure 13 and Table 2).
The chewing patterns, as revealed by a kinegiograph, were examined with EGN (Bio-Research Associates Inc.). The patient was instructed to chew gum on the left side for approximately 20 cycles, and then to chew the gum on the right side for approximately 20 cycles. The movement of the lower incisors was tracked during chewing movements by a magnet positioned between the lower central incisors. Figure 14 shows the frontal view of the chewing cycles. The pattern of the chewing cycles was extremely narrow at pretreatment, and during left-side chewing, the mandible moved to the right side during the opening and closing periods. At posttreatment, however, the narrow chewing pattern changed to a broad pattern, and the mandible moved downward when the mouth was opened and to the working side when the mouth was closed.
The occurrence of posterior crossbite is associated with persistent intensive finger-sucking habits12 or mouth breathing habits,13 which cause a lowered tongue position and results in narrowing of the maxillary dental arch. The patient described herein had a constricted maxillary arch and consequent unilateral posterior crossbite, with deviation of the mandible to the left side. Posterior crossbite on the left side was treated with an expansion plate, and a symmetric mandibular position was successfully induced using the removable plate with occlusal indentations. The results of early treatment for unilateral posterior crossbite and facial asymmetry were well maintained until the patient transitioned to a permanent dentition. Furthermore, early treatment resulted in harmonious growth of the maxilla and mandible with a symmetric facial profile. Although the treatment duration was long, this interceptive treatment using a removable appliance with a simple design was very effective and reduced the possibility of asymmetric growth of the mandible, thus avoiding complicated treatments in the future.
Children with posterior crossbite often have asymmetric muscular activity.6,14 Our finding was in agreement with those of previous studies: the masseter on the crossbite side was more active than that on the non-crossbite side;5,6 conversely, the anterior temporalis muscle on the crossbite side was less active than that on the non-crossbite side6 during maximal clenching in the posterior crossbite group. This asymmetric muscle activity may be explained by unilateral chewing habits and/or functional displacement of the mandible during maximal bite.6 In our patient, correction of unilateral posterior crossbite and mandibular deviation improved the balance of the masticatory muscles and the occlusal forces (Figures 12 and 13). We believe that symmetric positioning of the mandible facilitated balance in the neuromuscular system and influenced symmetric facial growth. According to previous studies,15,16 however, neuromuscular adaptation to crossbite does not occur immediately after treatment, and the remodeling capacity decreases with age.15 Therefore, early correction and subsequent retention for the posterior crossbite and mandibular deviation is required until the neuromuscular system adapts to the new mandibular position. In our patient, orthopedic treatment was initiated at early mixed dentition (8 years and 6 months of age), and the patient wore the appliance continuously over 10 months for retention after the treatment goal of the first phase was achieved. The posttreatment examinations performed approximately 3 years after correction of the posterior crossbite showed balanced occlusion and harmonious muscle activity. We believe that this duration would be sufficient for the neuromuscular system to stabilize and adapt to the new mandibular position and occlusion.
Occlusal analysis using the T-scan system showed a smaller contact area posttreatment than at pretreatment, although balance of the occlusal contacts was improved after treatment (Figure 12). The reason may be incomplete settling of the teeth immediately after removal of the fixed appliances. However, occlusal forces and occlusal contact areas would be expected to increase during and after the retention period due to settling of the posterior teeth.17
Posterior crossbite can affect the chewing pattern of patients.18,19,20,21 The difference in chewing patterns between the crossbite and non-crossbite sides is especially characterized by a reverse direction of closure, namely, reverse-sequence chewing cycles.20,21 A reverse-sequencing cycle occurs frequently whilst chewing on the crossbite side and on harder foods.19 Ben-Bassat et al.18 reported that the prevalence of the reverse-sequencing pattern before treatment was significantly decreased after correction of the posterior crossbite; however, it remained higher than that of the normal occlusion group. Our patient showed a similar pattern with the reverse-sequencing cycle on the crossbite side before treatment; however, the pattern changed to a normal cycle after treatment. In addition, the extremely narrow chewing cycle, namely, chopper type of chewing stoke, before treatment also changed to a more broad chewing cycle. On the basis of the results of the present study, it is suggested that early correction of posterior crossbite is very important for growing children to develop a normal chewing pattern.
Early correction of posterior crossbite in this patient resulted in functional changes as well as a symmetric facial profile. Treatment of facial asymmetry in growing children is considered necessary and must be initiated as early as possible to avoid asymmetric growth that can be induced by environmental factors.
Facial asymmetry with unilateral posterior crossbite and functional shift of the mandible was successfully treated in a growing patient, resulting in expansion of the maxilla and symmetrical positioning of the mandible. Functional evaluation revealed that the occlusal force balance and masticatory muscle activity were improved, and the chewing patterns were normalized.
References
1. Letzer GM, Kronman JH. A posteroanterior cephalometric evaluation of craniofacial asymmetry. Angle Orthod. 1967; 37:205–211. PMID: 19919216.
2. Kutin G, Hawes RR. Posterior cross-bites in the deciduous and mixed dentitions. Am J Orthod. 1969; 56:491–504. PMID: 5261162.

3. Egermark-Eriksson I, Carlsson GE, Magnusson T, Thilander B. A longitudinal study on malocclusion in relation to signs and symptoms of cranio-mandibular disorders in children and adolescents. Eur J Orthod. 1990; 12:399–407. PMID: 2086260.

4. Schmid W, Mongini F, Felisio A. A computer-based assessment of structural and displacement asymmetries of the mandible. Am J Orthod Dentofacial Orthop. 1991; 100:19–34. PMID: 2069142.

5. Andrade AS, Gavião MB, Derossi M, Gameiro GH. Electromyographic activity and thickness of masticatory muscles in children with unilateral posterior crossbite. Clin Anat. 2009; 22:200–206. PMID: 19031391.

6. Ingervall B, Thilander B. Activity of temporal and masseter muscles in children with a lateral forced bite. Angle Orthod. 1975; 45:249–258. PMID: 1059337.
7. Schröder U, Schröder I. Early treatment of unilateral posterior crossbite in children with bilaterally contracted maxillae. Eur J Orthod. 1984; 6:65–69. PMID: 6583066.
8. Hesse KL, Artun J, Joondeph DR, Kennedy DB. Changes in condylar postition and occlusion associated with maxillary expansion for correction of functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1997; 111:410–418. PMID: 9109586.
9. Kecik D, Kocadereli I, Saatci I. Evaluation of the treatment changes of functional posterior crossbite in the mixed dentition. Am J Orthod Dentofacial Orthop. 2007; 131:202–215. PMID: 17276861.

10. Cunha RF, Delbem AC, Costa L, de Abreu MG. Treatment of posterior crossbite in mixed dentition with a removable appliance: reports of cases. ASDC J Dent Child. 1999; 66:357–360. PMID: 10631894.
11. Garrido García VC, García Cartagena A, González Sequeros O. Evaluation of occlusal contacts in maximum intercuspation using the T-Scan system. J Oral Rehabil. 1997; 24:899–903. PMID: 9467991.

12. Melsen B, Stensgaard K, Pedersen J. Sucking habits and their influence on swallowing pattern and prevalence of malocclusion. Eur J Orthod. 1979; 1:271–280. PMID: 298212.

13. Harvold EP, Vargervik K, Chierici G. Primate experiments on oral sensation and dental malocclusions. Am J Orthod. 1973; 63:494–508. PMID: 4633053.

14. Andrade Ada S, Gameiro GH, Derossi M, Gavião MB. Posterior crossbite and functional changes. A systematic review. Angle Orthod. 2009; 79:380–386. PMID: 19216602.
15. Pirttiniemi PM. Associations of mandibular and facial asymmetries--a review. Am J Orthod Dentofacial Orthop. 1994; 106:191–200. PMID: 8059759.

16. Sonnesen L, Bakke M. Bite force in children with unilateral crossbite before and after orthodontic treatment. A prospective longitudinal study. Eur J Orthod. 2007; 29:310–313. PMID: 17317867.

17. Sultana MH, Yamada K, Hanada K. Changes in occlusal force and occlusal contact area after active orthodontic treatment: a pilot study using pressure-sensitive sheets. J Oral Rehabil. 2002; 29:484–491. PMID: 12028498.

18. Ben-Bassat Y, Yaffe A, Brin I, Freeman J, Ehrlich Y. Functional and morphological-occlusal aspects in children treated for unilateral posterior cross-bite. Eur J Orthod. 1993; 15:57–63. PMID: 8436197.

19. Brin I, Ben-Bassat Y, Blustein Y, Ehrlich J, Hochman N, Marmary Y, et al. Skeletal and functional effects of treatment for unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1996; 109:173–179. PMID: 8638566.

20. Nie Q, Kanno Z, Xu T, Lin J, Soma K. Clinical study of frontal chewing patterns in various crossbite malocclusions. Am J Orthod Dentofacial Orthop. 2010; 138:323–329. PMID: 20816302.

21. Piancino MG, Comino E, Talpone F, Vallelonga T, Frongia G, Bracco P. Reverse-sequencing chewing patterns evaluation in anterior versus posterior unilateral crossbite patients. Eur J Orthod. 2012; 34:536–541. PMID: 21921301.

Figure 1
Pretreatment photographs of facial symmetry of the patient at the age of 8 years and 6 months.
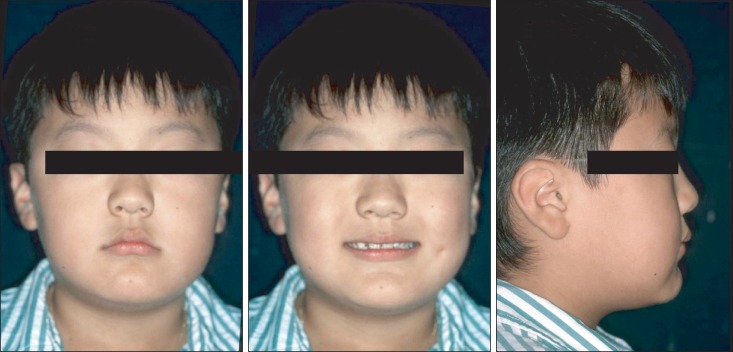
Figure 3
Pretreatment cephalometric and panoramic radiographs obtained at the age of 8 years and 6 months.
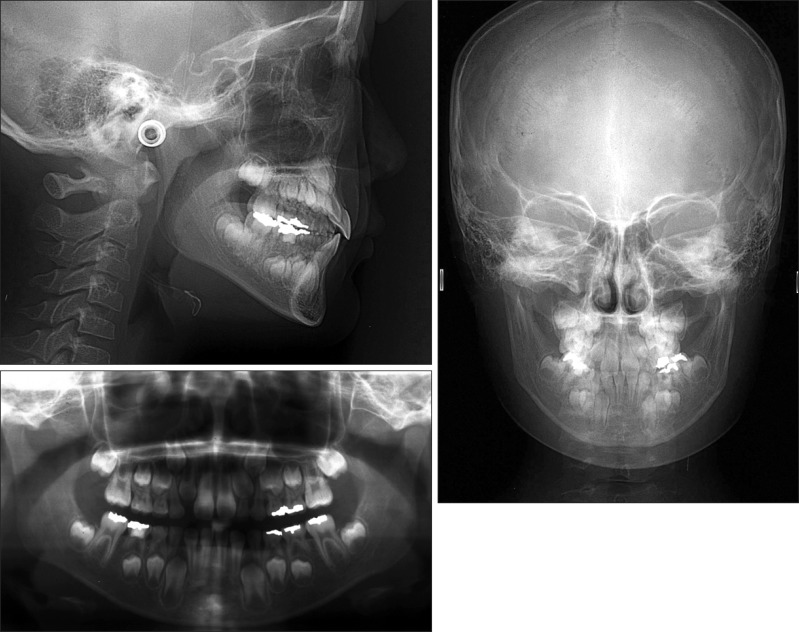
Figure 5
Bite blocks of the expansion plate with occlusal indentations (A, arrow head) were adjusted using the construction bite, which was taken with the incisors in a coincident dental midline (B).
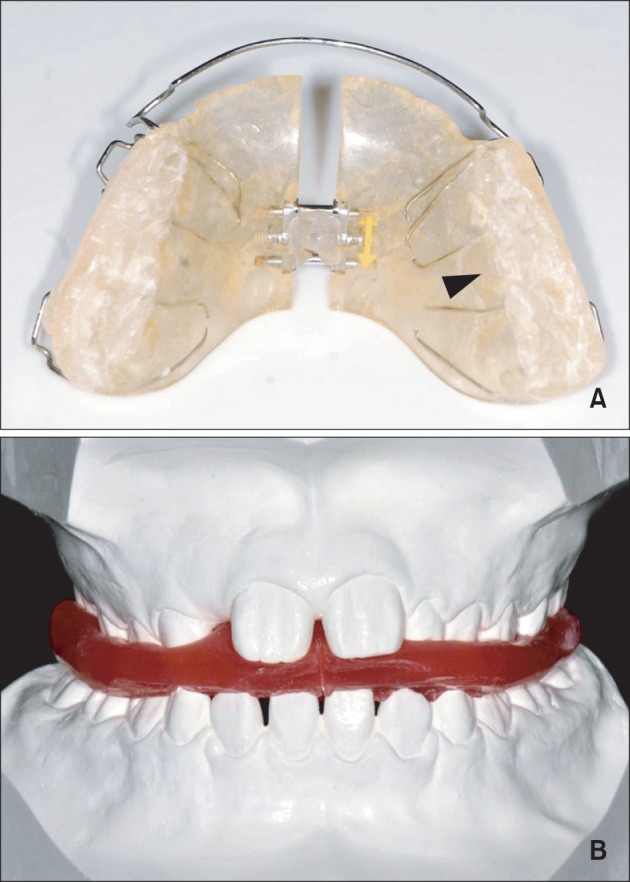
Figure 7
Intraoral photographs obtained after the first phase of treatment (patient age, 10 years and 6 months).

Figure 8
Facial and intraoral photographs obtained after the second phase of treatment (patient age, 13 years and 2 months).

Figure 9
Panoramic and cephalometric radiographs obtained after the second phase of treatment (patient age, 13 years and 2 months).

Figure 10
Superimposed cephalometric tracings at pretreatment (red, at 8 years and 6 months of age), after the first phase of treatment (green, at 10 years and 6 months of age), and after the second phase of treatment (blue, at 13 years and 2 months of age).
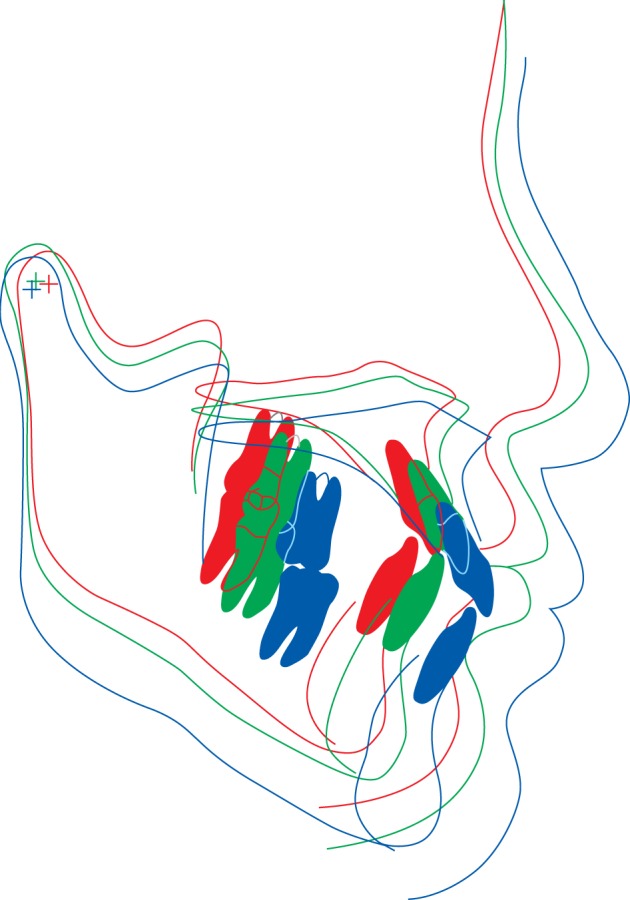
Figure 11
Tracings of submentovertex radiographs. A, Pretreatment (at 8 years and 6 months of age). B, After the second phase of treatment (at 13 years and 2 months of age).
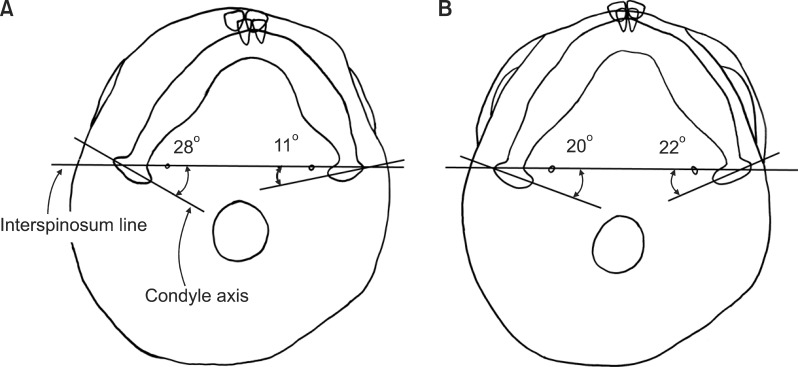
Figure 12
T-scan recordings. A, Pretreatment (at 8 years and 6 months of age). B, After the second phase of treatment (at 13 years and 2 months of age).
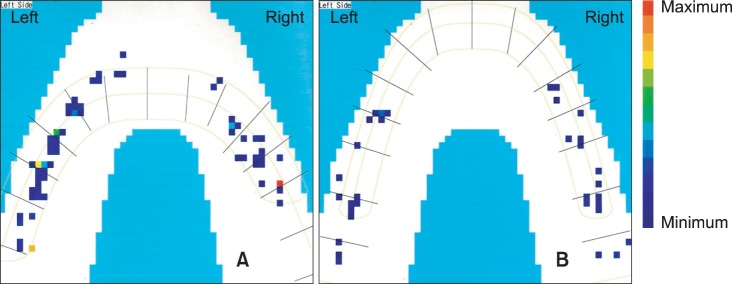
Figure 13
Electromyographic recordings of the anterior temporal muscle and masseter muscle. A, Pretreatment (at 8 years and 6 months of age). B, After the second phase of treatment (at 13 years and 2 months of age).
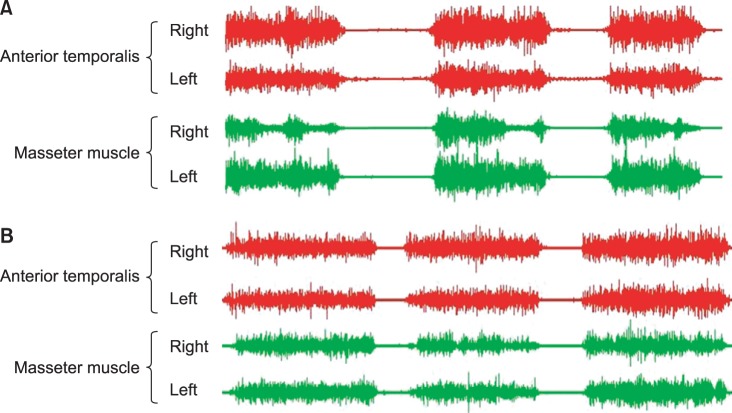
Figure 14
Chewing cycle in the frontal view. The X- and Y-axes represent lateral and vertical movements, respectively. The red line indicates opening and the blue line indicates closing movements. A, Chewing cycles on the right and left side pretreatment. B, Chewing cycles on the right and left side after the second phase of treatment.
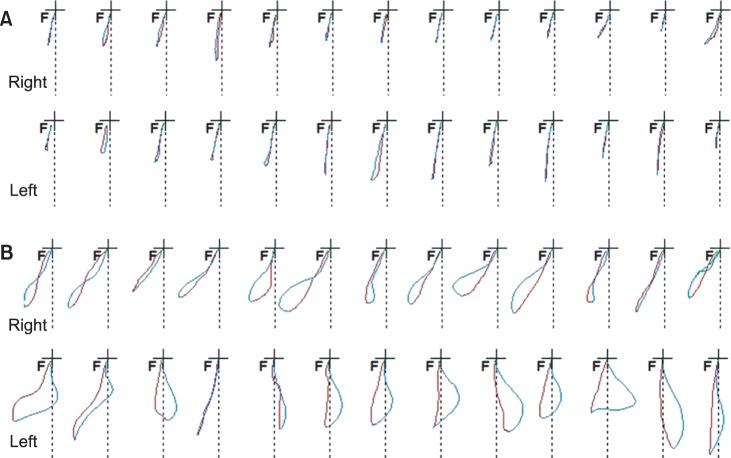
Table 1
Cephalometric measurements
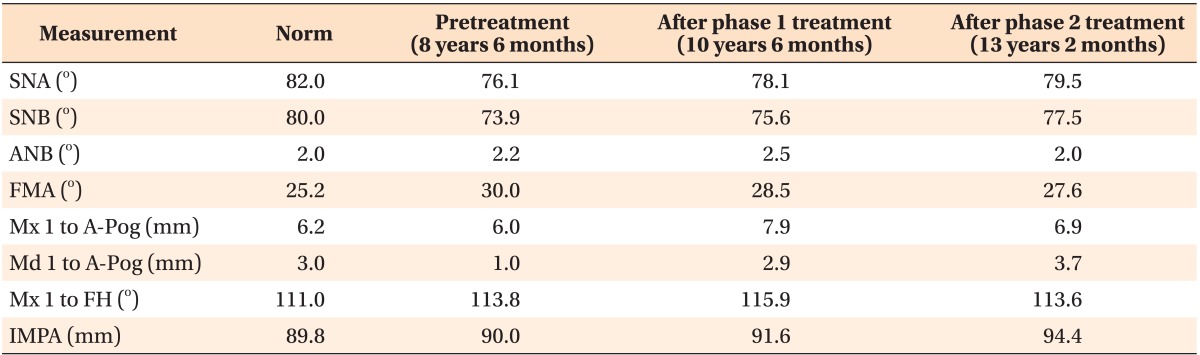
SNA, sella-nasion-A point angle; SNB, sella-nasion-B point angle; ANB, A point-nasion-B point angle; FMA, Frankfurt horizontal plane-mandibular plane angle; Mx 1, maxillary central incisor; Md 1, andibular central incisor; A-Pog, line through A point and pogonion; FH, Frankfurt horizontal plane; IMPA, lower incisor-mandibular plane angle.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download