Abstract
Objective
To evaluate the changes in cortical bone thickness, alveolar bone height, and the incidence of dehiscence and fenestration in the surrounding alveolar bone of posterior teeth after rapid maxillary expansion (RME) treatment using cone-beam computed tomography (CBCT).
Methods
The CBCT records of 20 subjects (9 boys, mean age: 13.97 ± 1.17 years; 11 girls, mean age: 13.53 ± 2.12 year) that underwent RME were selected from the archives. CBCT scans had been taken before (T1) and after (T2) the RME. Moreover, 10 of the subjects had 6-month retention (T3) records. We used the CBCT data to evaluate the buccal and palatal aspects of the canines, first and second premolars, and the first molars at 3 vertical levels. The cortical bone thickness and alveolar bone height at T1 and T2 were evaluated with the paired-samples t-test or the Wilcoxon signed-rank test. Repeated measure ANOVA or the Friedman test was used to evaluate the statistical significance at T1, T2, and T3. Statistical significance was set at p < 0.05.
Results
The buccal cortical bone thickness decreased gradually from baseline to the end of the retention period. After expansion, the buccal alveolar bone height was reduced significantly; however, this change was not statistically significant after the 6-month retention period. During the course of the treatment, the incidence of dehiscence and fenestration increased and decreased, respectively.
During rapid maxillary expansion (RME), heavy orthodontic forces are transmitted to the maxilla through the teeth,1 and unfavorable changes may occur in the anchor teeth and their supporting tissues, including buccal crown tipping, root resorption, reduction of buccal bone thickness, and marginal bone loss.2-4
Rungcharassaeng et al.4 performed a study on the CBCT records of 30 subjects taken before and after RME, and found that buccal crown tipping, reduction of buccal bone thickness, and marginal bone loss had occurred within 3 months after RME. Kartalian et al.5 compared 25 patients who underwent RME with age- and gender-matched controls using cone-beam computed tomography (CBCT) scans, and showed that the alveoli (but not the teeth) had tipped buccally after RME.
RME has also been reported to produce alveolar bone fenestration and/or dehiscence in the buccal aspects of the maxillary teeth.6,7 Garib et al.6 investigated the periodontal effects of tooth- and tooth-tissue-borne appliances, and found that RME treatment could lead to bone dehiscence in the buccal aspects of the anchor teeth. Baysal et al.8 evaluated root resorption after RME via CBCT and found significant root volume loss in the posterior teeth.
The probing of gingival tissues and radiographic methods are mostly preferred in evaluating the osseous support of the teeth.9 In radiographic methods, bitewing and periapical radiographs are widely used.10 However, radiographic methods have some limitations, including superimposition of the anatomic structures and difficulty in reproducing angles over time.11 Moreover, the destruction of the buccal plate cannot be distinguished from lingual defects.12 Because of these various issues, conventional radiography remains a limited tool for periodontal diagnosis.13
Recently, CBCT was introduced for head and neck applications. The main advantage of CBCT is the ability to evaluate the real anatomy without superimposition of the neighboring structures. CBCT and conventional methods have been compared by linear measurements of periodontal defects, and the methods were found to be comparable in terms of accuracy.14 Notably, CBCT also provides the ability to observe defects in all three dimensions.15
Although the effects of RME on cortical bone thickness and alveolar bone height were investigated in previous studies4,5 by means of CBCT, no study evaluating the follow-up period has been published. Therefore, the aim of this study was to evaluate the effects of RME on cortical bone thickness, alveolar bone height, and the incidence of dehiscence and fenestration after a 6-month follow-up period. For the purpose of this study, the null hypothesis assumed that no significant changes in the cortical bone thickness, alveolar bone height, and incidence of dehiscence and fenestration would occur after RME treatment.
The CBCT records of 20 subjects (9 boys, mean age: 13.97 ± 1.17 years; 11 girls, mean age: 13.53 ± 2.12 years) were obtained from the archives of the Oral and Maxillofacial Radiology Department, Dicle University (Diyarbakır, Turkey). All patients fulfilled the following criteria: 1) bilateral cross-bite related to a maxillary transverse deficiency; 2) no history of previous orthodontic treatment or a systemic disease; and 3) all maxillary teeth were present and fully erupted, with the exception of the third molars. All 20 patients had undergone RME with a Hyrax-type expander as a part of their orthodontic treatment. T1 scans were obtained before the placement of the appliance, and T2 scans were acquired directly after the end of the activation. Of the 20 patients, 10 patients had 6-month retention records (T3).
Ethical approval had already been obtained from the Ethical Committee of Dicle University (DUDFEK 2009/21) for the aims of another study; the patients were not exposed to extra radiation for this retrospective study. Therefore, a second ethical approval was not obtained.
In our department, the expansion protocol using the Hyrax screw is as follows: the appliance consists of an expansion screw welded on the bands on the first premolar and molar teeth. The screw is turned twice a day (once in the morning and in the evening) until the palatal cusps of the upper posterior teeth are in contact with the buccal cusps of the lower posterior teeth. During the retention period, the expansion appliance is left in the mouth for the first 3 months, and is replaced with a transpalatal arch when the expander is removed. Fixed orthodontic treatment is initiated after the retention period.
All tomographs were obtained using i-CAT® (Model 17-19; Imaging Sciences International, Hatfield, PA, USA) by the same operator at the following settings: exposures were made at 5.0 mA and 120 kV for 9.6 seconds, and the axial slice thickness was 0.3 mm. The patients were positioned sitting upright in the CBCT machine, with one strap placed over the forehead to orient the Frankfort horizontal plane parallel to the floor.
The Digital Imaging and Communications in Medicine (DICOM) files were imported into Dolphin 3D (Dolphin Imaging, Chatsworth, CA, USA) for further analysis. In this program, the orientation of each 3-dimensional volumetric data set was standardized by using the Frankfort horizontal line as the x-axis, the transporionic line as the y-axis, and the midsagittal line as the z-axis. The reference planes were defined by using the volumetric rendering view along with the multiple planar views.16
All of the cortical bone thickness and buccal alveolar height (BAH) measurements were performed using Dolphin Imaging 11.0 Premium (Dolphin Imaging) on hard tissue segmentation by one author who was blinded to the patient time points.
The cortical bone thickness of the maxillary canine, the first and second premolars, and the first molar for the left and right segments were measured using the axial clipping function of the software. To measure the cortical bone thickness at 3 different levels, cross-sections parallel to the Frankfort horizontal line were obtained at the trifurcation point, the middle of the distobuccal root, and the apex of the distobuccal root of the right first molar tooth. These levels were defined as the furcation-level, middle, and apical cortical bone thickness. To identify precisely the middle and apical thirds of the root, the length was measured with the program automatically on the coronally clipped images.
The distances between the outer border of the cortical bone and the teeth were measured both buccally and palatally, and defined as the buccal and palatal cortical bone thickness (BCBT and PCBT, respectively) (Figure 1). However, the method was modified in the following situations: if the roots of the upper premolars were shorter than the distobuccal roots of the first molars, the distances between the outer bone plate and the nearest point to the premolar apices were used for the measurements. When the maxillary sinuses spanned around the roots of the teeth, the distance between the apices and the sinus wall was accepted as zero. In the case of tooth rotation, the thickness was evaluated using the nearest point of the root to the bone plate.
The other measurement was the BAH of the maxillary posterior teeth. Using the coronal clipping function of the program, the distance between the cusp tips of the posterior teeth and the buccal alveolar crest was determined separately for the right and left sides (Figure 2). For the first molar teeth, the buccal crest level was determined from the mesiobuccal, middle, and distobuccal aspects of the teeth.
The presence of dehiscence and fenestration was evaluated on the i-CAT® software program according to the method described by Evangelista et al.17 (Figures 3 and 4). The axial inclination of the tooth was placed perpendicular to the horizontal plane, and the total root length was evaluated in cross-sectional slices at the buccal and palatal surfaces. Images that showed no cortical bone around the tooth in at least 3 consecutive views were recorded as having dehiscence or fenestration. The defect was classified as fenestration when the defect did not involve the alveolar crest. When the alveolar crest was more than 2 mm from the cemento-enamel junction, the defect was recorded as dehiscence.18
Figures 5 and 6 show the examples of decrease in buccal cortical plate thickness and increase in the buccal alveolar height of maxillary molar teeth after RME, respectively. The palatal cortical bone thickness at baseline, after RME and after retention is presented in Figure 7.
All statistical analyses were performed with the SPSS 16.0 (SPSS Inc, Chicago, IL, USA). The Shapiro-Wilk and Levene's variance homogeneity tests were used to determine the normality of the data. For comparing the mean values between the T1 and T2 measurements, a paired t-test and the Wilcoxon signed rank test were used for normally and non-normally distributed data, respectively. For the statistical evaluation of the pre-expansion, post-expansion, and 6-month follow-up data, repeated measure ANOVA with Bonferroni correction was used for normally distributed data, while the Friedman tests were used for non-normally distributed data. Statistical significance was set at p < 0.05. The arithmetic mean and standard deviation were calculated for all measurements.
For determining the errors associated with CBCT measurements, 15 tomographs were selected randomly, and their measurements were repeated 4 weeks after the first measurements by the same examiner. Intraclass correlation coefficients were determined for the 2 sets of measurements and were found to be higher than 0.90, indicating that the reliability of all the measurements was acceptable.
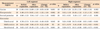
A comparison of the BCBT and PCBT measurements before and after RME treatment is shown in Table 1. With the exception of the apical region of the first and second left premolars, the mesial apical region of the right molar, and the middle region of the right canine, a decrease in the BCBT was observed at the 3 levels for all investigated teeth. For the canine and premolar teeth, the decrease in BCBT was statistically significant only at the furcation level for the right segment. For the second premolar teeth, the decrease was statistically significant in the middle region for both for the left and right segments. In terms of the decrease in BCBT, the first molar mesial and distal roots were the most severely affected among the investigated teeth. The decrease in BCBT was statistically significant for the middle and apical levels of the left segment and for the middle and furcation levels for the right segment.
When the PCBT measurements were evaluated, a general decrease was observed, but the decrease was not symmetrical for the left and right segments. For the canine and second premolar teeth, a decrease was observed on the left side, while an increase occurred at the right side for the middle and apical levels.
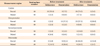
A comparison of the BAH before and after RME is shown in Table 2. The BAH measurements of all investigated posterior teeth were increased. With the exception of the left molar midfurcation level, these differences were found to be statistically significant, indicating the vertical alveolar height decreased immediately after the expansion period.
The descriptive statistics of the BCBT and PCBT measurements and the statistical comparisons of these values at the T1, T2, and T3 time periods are shown in Table 3. Except for the furcation level of the left canine, the BCBT decreased from the baseline to the end of the 6-month follow-up period at all 3 levels. Meanwhile, no significant increase in BCBT was found during retention period (T2 - T3) at the furcation level of the left and right canines and the right premolar and right molar. For the other levels, gradual decreases from T2 to T3 was observed. For the apical part of the canine tooth, a dramatic and statistically significant decrease in the BCBT was observed during the T1 - T3 and T2 - T3 time periods. For the left premolar and molar teeth, no significant decreases were found for the furcation level. Interestingly, for the right segment, no significant difference was recorded for the first premolar teeth. The only statistically significant difference at the furcation level during the T1 - T3 and T2 - T3 time periods was recorded for the right second premolar teeth. At the furcation level of the mesial and distal roots of the first molar, the difference was statistically significant at T2 and recovered at T3.
The PCBT decreases were found to be statistically significant at the apical level for all teeth, with the exception of the left first premolar. The decreases were statistically significant for the right molar teeth at the furcation (T1 - T3), middle (T2 - T3), and apical (T2 - T3) levels.
Comparisons of the BAH measurements from the baseline to the 6-month follow-up are shown in Table 4. The increase in BAH during the treatment period (T1 - T2) was statistically significant for the right canine tooth (p = 0.016). The changes in the T1 - T3 period for the left second premolar and right molar distobuccal level was statistically significant (p = 0.038 and p = 0.035, respectively). No statistically significant difference was found between the T2 - T3 periods.
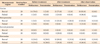
The incidence of alveolar defects in the 20 patients before and after RME are shown in Table 5. Meanwhile, the incidence of baseline, post-treatment, and post-retention alveolar defects in 10 of the patients is presented in Table 6. In general, the incidence of dehiscence was greater for the post-treatment and post-retention values than for the baseline ones after RME. The percentage of fenestrations decreased after treatment.
Because the RME treatment had statistically significant effects on the surrounding alveolar bone, the null hypothesis of this study was rejected.
RME is a common clinical procedure to correct maxillary constriction and arch length discrepancies.4 In adolescents, 65% of the total expansion was shown to be the result of dental movement,19 and it may be thought that RME may have detrimental effects on the teeth and their supporting tissues.
CBCT scanning provides information for RME, not obtainable from other methods especially from a periodontal perspective. Moreover, as the current study was designed in accordance with the principle of ALARA (as low as reasonably achievable), individuals were not exposed to extra radiation beyond the needs for orthodontic treatment. Also an informed consent form signed by the patients' parents, doctor and technician has to be obtained from every patient that goes under CBCT scanning in our university protocol.
Ekström et al.20 found that the mineralization of a midpalatal suture was completed 3 months after RME, and advocated a retention period of 3 to 6 months for a good long-term stability. In the current study, 6-month retention records were obtained from the archive and used in the analyses, since this period was thought to be adequate for the adaptation of the hard and soft tissues.
The force generated by the activation of the appliance initially leads to compression of the periodontal ligament, bending of the alveolar bone, and tipping of the anchor teeth. Afterwards, a gradual opening of the midpalatal suture occurs.21 Hicks22 found that the angulation between the right and left molars increased from 1° to 24° during expansion and showed that these changes are due to alveolar bending and the tipping of the posterior teeth in the alveolar bone. By contrast, Kartalian et al.5 showed no statistically significant dental tipping after RME. Hence, one can conclude that RME may result in the tipping of the maxillary posterior teeth. In the present study, the level of the buccal alveolar crest was lowered in all investigated teeth immediately after RME. These changes may be attributed to the tipping of the maxillary posterior teeth, and this tipping movement may lead to resorption of the crestal alveolar bone. This finding is in accordance with previous studies.23,24
After the retention period, the alveolar bone height did not change, but the buccal cortical bone generally continued to decrease. According to Barber and Sims,25 the residual loads may cause the alveolar bone to be compressed toward the buccal aspect of the anchor teeth, which are held rigidly by the expansion devices used as retainers. Cotton26 stated that post-expansion angular changes of the maxillary molars might be due to the stretched fibers of the attached palatal mucosa. Thus, the roots of the posterior teeth may move buccally, and the thickness of the buccal cortical bone may continue to decrease.
In the palatal portion of the tooth, a trend toward an increase in the PCBT after the active phase of the RME was observed. This finding can be attributed to the buccal tipping of the posterior teeth, which increases the distance between the palatal cortical plate and the root surfaces. Meanwhile, the decreases in PCBT in the retention period may show the compensatory resorption under the periosteum. The thickness of the bone may have been maintained through this compensatory response. Sarikaya et al.27 showed compensatory resorption under buccal periosteum when the maxillary incisors were retracted.
Because of the considerable force needed to break the median palatine suture during RME, an evaluation of the periodontal structures, including the alveolar bone and gingival biotype, is an important aspect of the procedure.17 Evangelista et al.17 compared the presence of alveolar defects (dehiscence and fenestration) in patients with different malocclusions, and found that the maxillary canines and first premolars showed a high prevalence of dehiscence. This finding is of importance for treatments involving RME, since the first premolars, and sometimes the canines, are the supporting teeth for orthopedic devices. In the current study, the incidence of dehiscence on the buccal surface of posterior teeth varied between 2.5% and 55.0%. Additionally, this incidence increased during the use of the tooth-borne RME appliance (range: 10.0 - 72.5%). We think that the effects of dental inclination and the decrease in alveolar bone height are associated with these alveolar defects.
Wainwright7 showed that when the apex of a tooth is moved facially, cortical bone penetration occurs. This penetration is closed with bone deposition on the buccal surface if the apex of the tooth is moved to the opposite direction and retained in that position. In the present study, the incidence of dehiscence and fenestration increased and decreased after RME, respectively. The potential of a fenestration to become a dehiscence28 may explain this increase. Although a general increase was shown in the occurrence of these alveolar defects for the buccal surface of the first molar teeth, the percentage of alveolar defects decreased overall. This decrease is attributed to the horizontal bone loss. Meanwhile, the least amount of alveolar defects was found in the second premolars. It is logical to find greater alveolar defects in the first premolar and molar teeth, as they are the anchor teeth. Although the canines are not anchor teeth, the initial supra-alveolar position of these teeth might cause dehiscence at the buccal surfaces, and these might not recover.
In the present study, CBCT scans were used to evaluate the alveolar defects. As we can measure the bone around the teeth accurately by means of axial and cross-sectional sections, alveolar bone measurements and bone defects may be judged by CBCT. Leung et al.28 evaluated the accuracy and reliability of CBCT for measuring alveolar bone height and alveolar defects by correlating direct and indirect CBCT measurements. The correlation coefficient with direct and CBCT measurements was 0.870 for the bone margin measurements. On the other hand, the detection of fenestrations and dehiscence was more prone to error. For dehiscence, both the sensitivity and specificity were about 0.80. The diagnosis of alveolar defects depends on the length and thickness of the alveolar cortical plate and the visualization of the periodontal ligament space.17 Fuhrmann et al.29 observed that when the cortical thickness is less than 0.5 mm, the CBCT scan is relatively accurate. Nonetheless, these measurements are made in extremely small scales. Therefore, the scoring of these thicknesses can be a possible limitation of our study.
Another limitation of this study is the small sample size. To overcome this limitation, the same author performed all measurements. Moreover, the high accuracy of the quantitative measurements on the CBCT images supports the reliability of the outcomes and makes the small sample size acceptable. Furthermore, to prevent the underestimation of p-values, repeated measure ANOVA, which is a much more powerful statistical approach than independent ANOVA, was used. Future studies with a large sample size are needed for further evaluation.
Figures and Tables
Figure 1
Buccal cortical bone thickness (BCBT) and palatal cortical bone thickness (PCBT) at the level of the trifurcation of the first molar.
Figure 2
Buccal alveolar height (BAH: distance between the cusp tip and the buccal alveolar crest) of the maxillary first molar.

Figure 3
The presence of dehiscence at 3 consecutive views. Arrow shows the localization of dehisence.

Figure 4
The presence of fenestration at 3 consecutive views. Arrow shows the localization of dehisence.

Figure 5
An example of a decrease in the buccal cortical bone thickness of the maxillary right molar.

Figure 7
An example of treatment changes: the palatal cortical bone thickness increased after active expansion and decreased at the end of retention.

Table 3
Comparison of BCBT and PCBT measurements before and after rapid maxillary expansion and following the 6-month retention period

Table 4
Comparison of buccal alveolar height measurements before and after rapid maxillary expansion and following the 6-month observation period

References
1. Langford SR, Sims MR. Root surface resorption, repair, and periodontal attachment following rapid maxillary expansion in man. Am J Orthod. 1982. 81:108–115.

2. Graber TM. Graber TM, editor. Chapter 10. Dentofacial orthopedics. Current orthodontic concepts and tech niques. 1969. Vol 11. Philadelphia: WB Saunders Company.
3. Odenrick L, Karlander EL, Pierce A, Kretschmar U. Surface resorption following two forms of rapid maxillary expansion. Eur J Orthod. 1991. 13:264–270.

4. Rungcharassaeng K, Caruso JM, Kan JY, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007. 132:428.e1–428.e8.

5. Kartalian A, Gohl E, Adamian M, Enciso R. Cone-beam computerized tomography evaluation of the maxillary dentoskeletal complex after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2010. 138:486–492.

6. Garib DG, Henriques JF, Janson G, Freitas MR, Coelho RA. Rapid maxillary expansion-tooth tissue-borne versus tooth-borne expanders: a computed tomography evaluation of dentoskeletal effects. Angle Orthod. 2005. 75:548–557.
7. Wainwright WM. Faciolingual tooth movement: its influence on the root and cortical plate. Am J Orthod. 1973. 64:278–302.

8. Baysal A, Karadede I, Hekimoglu S, Ucar F, Ozer T, Veli I, et al. Evaluation of root resorption following rapid maxillary expansion using cone-beam computed tomography. Angle Orthod. 2012. 82:488–494.

9. Jeffcoat MK. Current concepts in periodontal disease testing. J Am Dent Assoc. 1994. 125:1071–1078.

10. Molander B. Panoramic radiography in dental diagnostics. Swed Dent J Suppl. 1996. 119:1–26.
11. Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006. 77:1261–1266.

12. Rees TD, Biggs NL, Collings CK. Radiographic interpretation of periodontal osseous lesions. Oral Surg Oral Med Oral Pathol. 1971. 32:141–153.

13. Hirschmann PN. Radiographic interpretation of chronic periodontitis. Int Dent J. 1987. 37:3–9.
14. Vandenberghe B, Jacobs R, Yang J. Detection of periodontal bone loss using digital intraoral and cone beam computed tomography images: an in vitro assessment of bony and/or infrabony defects. Dentomaxillofac Radiol. 2008. 37:252–260.

15. Walker L, Enciso R, Mah J. Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2005. 128:418–423.

16. Sanders DA, Rigali PH, Neace WP, Uribe F, Nanda R. Skeletal and dental asymmetries in Class II subdivision malocclusions using cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010. 138:542.e1–542.e20.

17. Evangelista K, Vasconcelos Kde F, Bumann A, Hirsch E, Nitka M, Silva MA. Dehiscence and fenestration in patients with Class I and Class II Division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010. 138:133.e1–133.e7.

18. Persson RE, Hollender LG, Laurell L, Persson GR. Horizontal alveolar bone loss and vertical bone defects in an adult patient population. J Periodontol. 1998. 69:348–356.

19. Krebs A. Midpalatal suture expansion studies by the implant method over a seven-year period. Rep Congr Eur Orthod Soc. 1964. 40:131–142.
20. Ekström C, Henrikson CO, Jensen R. Mineralization in the midpalatal suture after orthodontic expansion. Am J Orthod. 1977. 71:449–455.

21. Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961. 31:73–90.
22. Hicks EP. Slow maxillary expansion. A clinical study of the skeletal versus dental response to low-magnitude force. Am J Orthod. 1978. 73:121–141.
23. Thilander B, Nyman S, Karring T, Magnusson I. Bone regeneration in alveolar bone dehiscences related to orthodontic tooth movements. Eur J Orthod. 1983. 5:105–114.

24. Engelking G, Zachrisson BU. Effects of incisor repositioning on monkey periodontium after expansion through the cortical plate. Am J Orthod. 1982. 82:23–32.

25. Barber AF, Sims MR. Rapid maxillary expansion and external root resorption in man: a scanning electron microscope study. Am J Orthod. 1981. 79:630–652.

26. Cotton LA. Slow maxillary expansion: skeletal versus dental response to low magnitude force in Macaca mulatta. Am J Orthod. 1978. 73:1–23.

27. Sarikaya S, Haydar B, Ciğer S, Ariyürek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop. 2002. 122:15–26.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download