Abstract
Orthodontic closure of old, edentulous spaces in the mandibular posterior region is a major challenge. In this report, we describe a method of orthodontic closure of edentulous spaces in the mandibular posterior region accelerated by piezoelectric decortication and alveolar ridge expansion. Combined piezosurgical and orthodontic treatments were used to close 14- and 15-mm-wide spaces in the mandibular left and right posterior areas, respectively, of a female patient, aged 18 years and 9 months, diagnosed with skeletal Class III malocclusion, hypodontia, and polydiastemas. After the piezoelectric decortication, segmental and full-arch mechanics were applied in the orthodontic phase. Despite some extent of root resorption and anchorage loss, the edentulous spaces were closed, and adequate function and esthetics were regained without further restorative treatment. Alveolar ridge expansion-assisted orthodontic space closure seems to be an effective and relatively less-invasive treatment alternative for edentulous spaces in the mandibular posterior region.
Closing old edentulous spaces in the mandibular posterior region is a major challenge. Successful outcomes are more difficult to achieve in adult patients because of the narrower compact alveolar ridge barrier and tipping of the remaining molars into the edentulous space. The possibility of complications such as root resorption and periodontal defects also increases with the age of the patient and length of the space to be closed.1,2 Some investigators have even asserted that such spaces should not be closed.3 However, spaces longer than 10 mm have been successfully closed in young patients,1 although problems with root parallelism and gingival dehiscence still occur.
Kessler3 suggested that if the buccolingual width of the alveolar ridge is narrower than the alveolus of the second molar, then edentulous spaces should not be closed because this would result in the loss of periodontal tissue. Tooth movement under such problematic conditions may require greater force and result in complications depending on the level of force used.
Various surgical techniques for removal of the cortical bone barrier to ease or accelerate mesial tooth movement into edentulous spaces have been described, especially corticotomy. Most of these techniques are very invasive, limiting the patient's postoperative comfort.4 Nevertheless, their primary aim is to aid in the demineralization of the compact alveolar ridge barrier, thereby optimizing the physiological bone response and accelerating mesial tooth movement.5 Therefore, these techniques could be beneficial for closing mandibular posterior spaces.
Wilcko et al.5 claimed that accelerated tooth movement after corticotomy is not a direct result of the operation but a physiological response of the bone, known as the regional acceleratory phenomenon, which is induced by bone damage. Sebaoun et al.6 suggested that alveolar decortication induces rapid and localized bone turnover and may be the main reason for accelerated tooth movement.
In this report, we describe a method of orthodontic closure of edentulous spaces in the mandibular posterior region accelerated by piezoelectric decortication and alveolar ridge expansion in a young adult patient. The reported treatment protocol is based on relatively newly acquired scientific data on corticotomy procedures.1,2,6,7
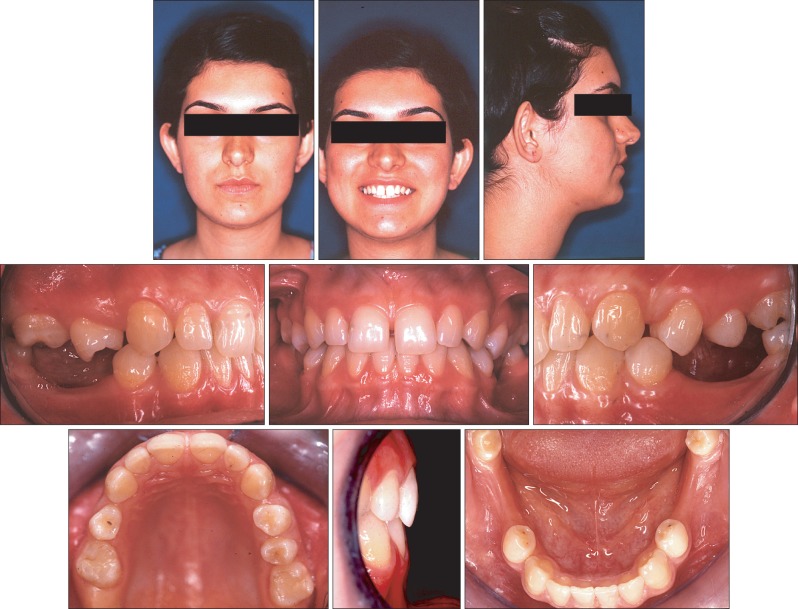
A female patient aged 18 years and 9 months was referred to our clinic because of a complaint of spaces between her teeth. The maxilla had a 5-mm space excess (Figure 1). The patient had diastemas between her maxillary central incisors and distal to the maxillary canines. Her maxillary right second premolar was missing and the maxillary right first premolar was rotated by 90 degrees.
In the mandibular dentition, 15- and 14-mm spaces were present between the first and the second premolars on the right and left sides, respectively, caused by either congenital absence or early loss of the first molars. All the existing second premolars were inclined mesially. Although the canines showed a Class I relationship, all the anterior teeth were slightly retroclined.
Pretreatment facial photographs showed a straight profile, with competent lips and a slightly prominent chin.
The patient had no relevant medical history. Her oral hygiene was satisfactory, and no periodontal problems were observed.
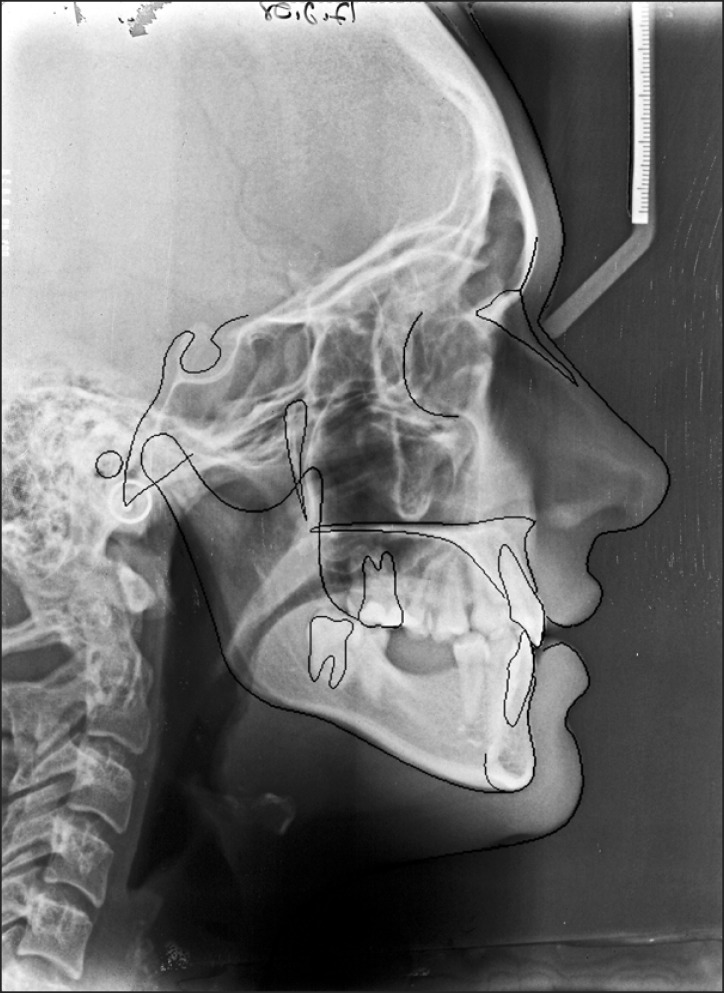
A panoramic radiograph (Figure 2A) showed that her mandibular first and third molars were missing and the mandibular second molars were impacted. The maxillary first and third molars were also missing. Cephalometric evaluation (Figure 3 and Table 1) indicated that the patient had skeletal Class III malocclusion and the vertical cephalometric values were within the normal range. The patient was diagnosed with skeletal Class III malocclusion, hypodontia, and polydiastemas.
Corticotomy was planned to expand the alveolar ridge in the mandibular posterior region and accomplish full closure of the edentulous spaces while decreasing the risks associated with removal of the alveolar ridge barrier. The procedure was similar to that used in previous studies of ridge-split osteotomy, involving buccolingual expansion of the cortical bone, as is used frequently in implant dentistry.7
Bearing in mind the total treatment time required, the first stage of the orthodontic treatment was focused on mandibular space closure with fixed appliances. Because of hypodontia, the aim was to maintain the rotated teeth in the same alignment at the end of the treatment to occupy the maximal possible space. Moreover, retention of severely rotated teeth becomes problematic if tight proximal contacts are not established; in particular, mandibular posterior spaces do not permit the establishment of tight proximal contacts. Finally, a lingual arch and miniscrew implants were planned for anchorage reinforcement.
The following treatment options were considered for mandibular space closure:
1. Restore the edentulous spaces with either bridges or dental implants and extract the impacted second molars.
2. Use dental or mini-anchorage implants for orthodontic space closure without any restorative treatment.
3. Use a protraction headgear for anchorage reinforcement.
4. Autotransplant the second premolars and/or second molars.
5. Perform horizontal alveolar distraction osteogenesis and either fill the spaces with dental implants or close the spaces with orthodontic appliances.
The first option was not chosen because higher occlusive forces in the mandibular posterior region could adversely affect the periodontal tissue around the premolars. The second option was not selected because the excess orthodontic force needed to move the premolars could cause complications such as root resorption or loss of anchorage. The third option was excluded because of the need for extended patient cooperation and the inability to apply continuous forces. The fourth option was not selected because the apices of the second premolars and second molars were completely formed. This option was also discounted because of the young age of the patient, relatively low success with such teeth, relatively low survival rates of such teeth,8 and increased risk of failure. The fifth option was rejected because of its associated risks and poor patient comfort during the expansion process.
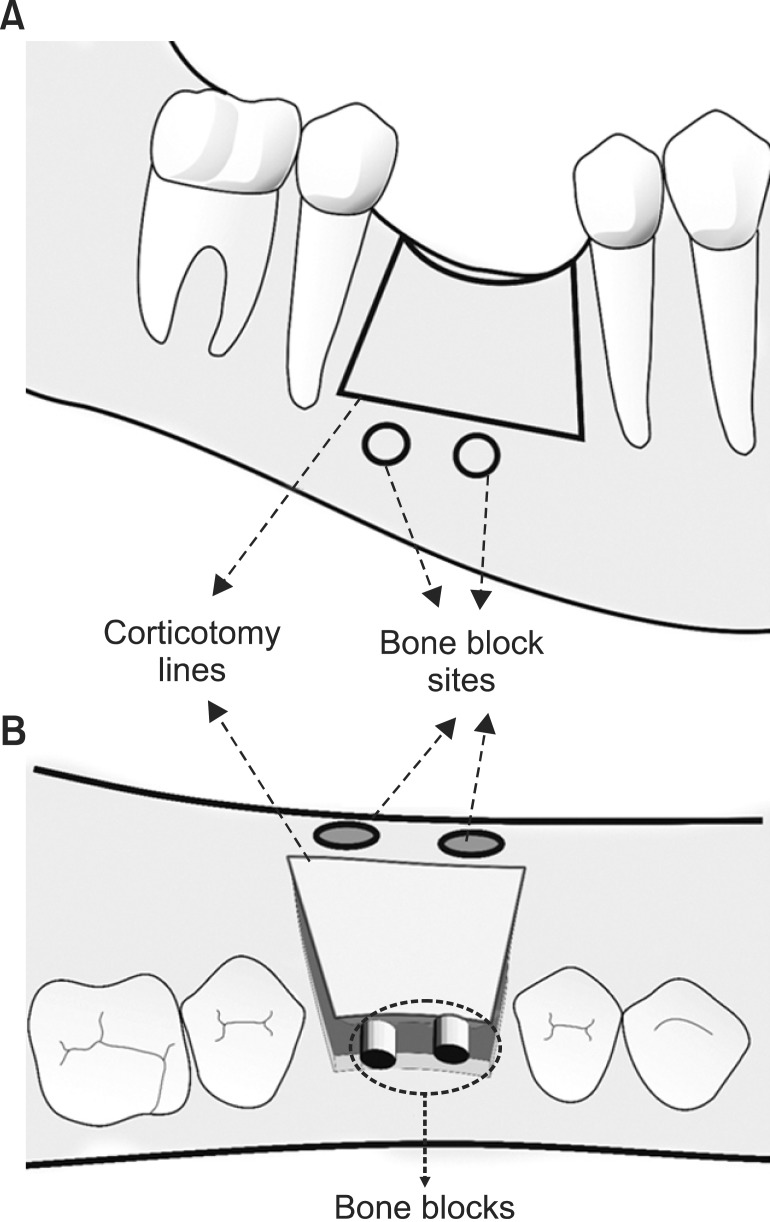
One week before the orthodontic treatment was to be started, 9-mm-deep horizontal osteotomies (Figures 4 and 5) were performed bilaterally with a piezoelectric device (Piezon Master Surgery; Electro Medical Systems, Nyon, Switzerland) on the mandibular alveolar crest 2 mm away from each tooth to facilitate faster mesial movement of the second premolars. Two vertical osteotomies and one horizontal osteotomy were then performed on the buccal side, and two 3-mm-diameter cylindrical bone blocks were removed from this horizontal osteotomy site. The bone blocks were placed in the space on the alveolar crest.
Mandibular orthodontic treatment was started with segmental fixed appliances (0.022-inch slot brackets with MBT prescription) and a lingual arch between the first premolars. After anchorage of the anterior teeth was reinforced by the lingual arch, two mini-anchorage screws were placed between the first premolar and the canine bilaterally. The second premolars were banded, and 0.017 × 0.025-inch stainless steel guidance wires were passively placed between the first and the second premolars. Light closed coil springs were employed for space closure (Figure 5C and 5D). The angles of the guidance wires were changed slowly at each visit after the initiation of guided tooth movement to upright the second premolars.
After alignment of the mandibular second premolars, space closure was continued with tiebacks, which were changed every 4 weeks. When the mandibular left and right second molars erupted into the oral cavity, after 6 and 8 months of orthodontic treatment, respectively, the teeth were bonded with thinner nickel-titanium wires (Figure 2B and 2C).
The mandibular second premolars were moved into the edentulous spaces over 19 months. After the spaces between the first and the second premolars were fully closed, tiebacks were used to move the second molars mesially. Unfortunately, mobility of the miniscrew implants was noticed, so the miniscrews were removed; most of the space between the second molars and the premolars was closed without the added anchorage of miniscrew implants.
Maxillary fixed orthodontic treatment was started 6 months after the mandibular treatment began. Anterior diastemas were closed with power chains. The maxillary right first premolar was stabilized in its rotated position. Class II elastics were used, together with rectangular stainless steel archwires on the maxillary teeth, to protrude the mandibular anterior teeth.
The entire fixed orthodontic treatment period was 2 years and 10 months. Maxillary Hawley and mandibular bonded retainers were used for retention.
At the end of the combined piezosurgical and orthodontic treatments, in the mandibular dentition, the space (approximately 15 mm) between the premolars on the right side was closed and only 1-mm space remained between the premolars on the left side. Adequate space was created for the mandibular second molars and they moved mesially. Therefore, adequate function and esthetics were regained without further restorative treatment. Both the mandibular second premolars and the maxillary right first premolar were left rotated (Figure 6).
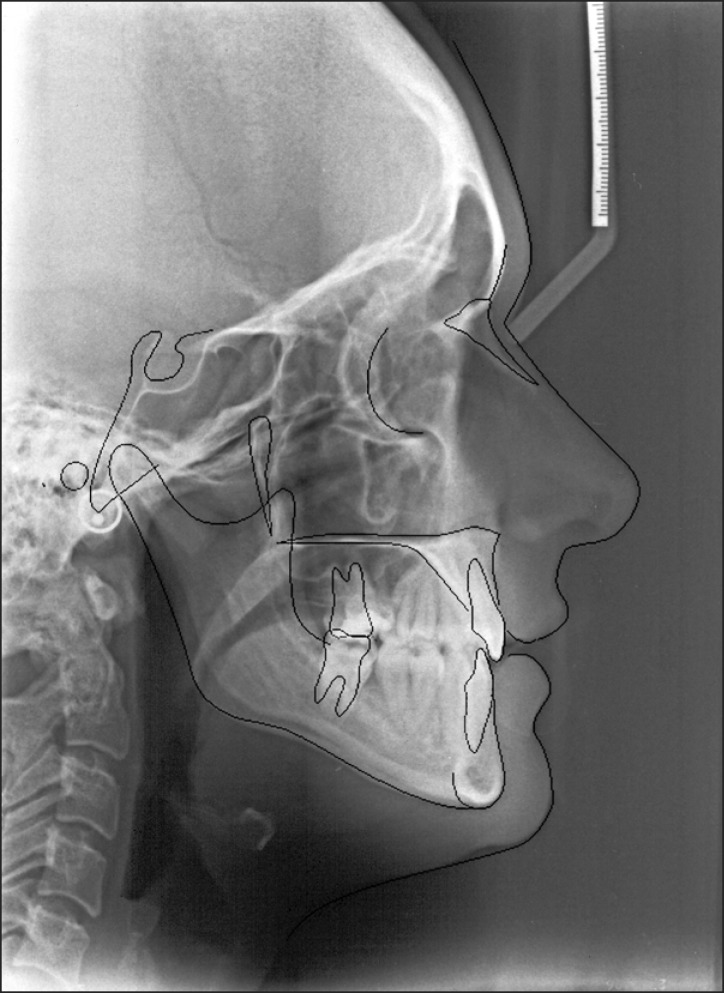
All the incisors were retroclined slightly (Figures 7, 8, and Table 1), despite the miniscrews and lingual arch used for maximal anchorage. This movement affected the soft-tissue profile, and the chin prominence increased. However, no serious esthetic problems occurred, and the patient did not complain about the lip posture.
Corticotomy-facilitated orthodontics was first introduced by Köle9 in 1959. Today, less-invasive techniques have mostly replaced Köle's invasive surgical procedure. However, the objective of the treatment remains the same: weakening the compact bone in some way to ease bone resorption and remodeling in the compact alveolar ridge barrier. Some researchers showed that the total orthodontic treatment time could be reduced to one-third of the conventional orthodontic treatment time by means of corticotomy.10 Corticotomy techniques for accelerating tooth movement generally involve full-size flaps, radicular corticotomy, and supra-apical osteotomy.9,11 These techniques were reported to be useful in some carefully selected cases. However, most of the techniques were difficult to apply for both the patients and the operators, and postoperative comfort was poor.4,6 A greater number of clinical and histological studies are needed to evaluate the effects of all aspects of such treatments adequately.
New techniques with newly developed devices have gained attention because of the disadvantages of the previous operations. Piezosurgical techniques represent one such development.12 We used piezoelectric tools for decortication because piezoelectric devices and minimally invasive surgical techniques promise minimal patient discomfort and greater patient acceptance.13
A similar treatment approach to the aforementioned corticotomy techniques was used for closing edentulous spaces in our case.12,13 However, the surgical technique was less invasive and involved a limited edentulous bone field. Incisions of the buccal wall of the mandible were anticipated to result in increased bone turnover and, therefore, faster tooth movement.13,14
Several studies have shown an increased risk of damage to the surrounding vascular and neural supplies of teeth by corticotomy.15 Most of these risks were not an issue in the present case because the corticotomy lines were a sufficient distance from the roots and other potentially problematic areas.
Following alveolar ridge expansion by corticotomy, the remaining space resembled a fresh extraction site. A previous study showed that faster tooth movement is achievable into a fresh extraction site.16 Moreover, Yu et al.17 found that intentionally creating bone sockets along the direction of tooth movement resulted in a greater extent of tooth movement: the intentional socket group in their study showed greater tooth movement than the extraction socket group. In the present case, the corticotomy lines and space between the expanded cortexes would have acted similar to bone sockets and eased the mesial movement of the mandibular second premolars and second molars. An additional advantage of expanding the alveolus is that it may decrease the risk of gingival recession, which is most likely to occur in areas where the root diameter is greater than the alveolar ridge width.3
Alveolar ridge splitting is used to obtain a wider horizontal dimension especially in the maxillary bone and allow simultaneous dental implant placement.7 The currently described method can be considered a modification of alveolar ridge splitting. After ridge splitting, fixation with miniscrews is optional and the decision depends on the mobility of the buccal cortex. Fixation of the buccal cortex and grafting of the gap between cortical bone walls increase stability and decrease bone loss in alveolar ridge splitting.18 In the present case, two cylindrical bone blocks were used to stabilize the alveolar ridges in their expanded positions, for autogenous bone grafting and achieving stable buccal cortical bone. Although the bone grafts alone provided adequate stabilization in the present case, miniscrews could be used for further stabilization.
Some extent of root resorption was anticipated following the tooth movement. At the end of the orthodontic treatment, small resorption centers were present on the mesial cervical areas of both the mandibular second premolar roots (Figure 2D). A diastema of 1 mm could not be closed between the right first and second premolars in the mandibular dentition. The resorption, periodontal status, and socioeconomic status of the patient forced us to complete the treatment as soon as the results were acceptable.
Miniscrew implants were used for anchorage reinforcement along with a lingual arch. After the miniscrews were removed, the mandibular second molars were moved mesially with the support of the lingual arch. Some degree of anchorage was lost in this part of the treatment and the mandibular incisors retroclined slightly. This also affected the lip posture and both the lips protruded. Anchorage loss could have been prevented if the miniscrew implants could have been maintained through the whole space closure process. This problem could also have been overcome if full-size archwires had been used for torque control for enough time. The early completion of the treatment prevented this kind of torque control.
Both the mandibular second premolars and the maxillary right premolar were stabilized in their rotated positions. Retention of rotated teeth is difficult after orthodontic treatment.19 Relapse is possible if no tight proximal contact exists between teeth. The rotated positions were accepted because the gingival folds between the roots prevented tight contacts. Prosthetic restoration of the rotated teeth was offered to the patient, but she rejected this option. Serious periodontal problems were not encountered at the end of the treatment, except for approximately 1-mm-deep periodontal folds between the first and the second premolars.
The treatment protocol in this case was aimed at tooth movement based on the physiological response of bone to corticotomy and alveolar ridge expansion. Despite the loss of anchorage to some degree, the mandibular edentulous spaces, which otherwise would have remained open, were closed with minimal complications. The results show that orthodontic space closure assisted by alveolar ridge expansion is a viable treatment option especially for old edentulous spaces. This alternative is valuable because it eliminates most of the risks associated with corticotomy.
References
1. Stepovich ML. A clinical study on closing edentulous spaces in the mandible. Angle Orthod. 1979; 49:227–233. PMID: 292345.
2. Hom BM, Turley PK. The effects of space closure of the mandibular first molar area in adults. Am J Orthod. 1984; 85:457–469. PMID: 6587780.

3. Kessler M. Interrelationships between orthodontics and periodontics. Am J Orthod. 1976; 70:154–172. PMID: 1066052.

4. Fischer TJ. Orthodontic treatment acceleration with corticotomy-assisted exposure of palatally impacted canines. Angle Orthod. 2007; 77:417–420. PMID: 17465647.

5. Wilcko MT, Wilcko WM, Bissada NF. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: a synthesis of scientific perspectives. Semin Orthod. 2008; 14:305–316.

6. Sebaoun JD, Surmenian J, Dibart S. Accelerated orthodontic treatment with piezocision: a mini-invasive alternative to conventional corticotomies. Orthod Fr. 2011; 82:311–319. PMID: 22105680.
7. González-García R, Monje F, Moreno C. Alveolar split osteotomy for the treatment of the severe narrow ridge maxillary atrophy: a modified technique. Int J Oral Maxillofac Surg. 2011; 40:57–64. PMID: 20729037.

8. Tsukiboshi M. Autotransplantation of teeth: requirements for predictable success. Dent Traumatol. 2002; 18:157–180. PMID: 12442825.

9. Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959; 12:515–529 concl. PMID: 13644913.
10. Alghamdi AS. Corticotomy facilitated orthodontics: Review of a technique. Saudi Dent J. 2010; 22:1–5. PMID: 23960473.

11. Ren A, Lv T, Kang N, Zhao B, Chen Y, Bai D. Rapid orthodontic tooth movement aided by alveolar surgery in beagles. Am J Orthod Dentofacial Orthop. 2007; 131:160.e1–160.e10. PMID: 17276852.

12. Mittal SK, Sharma R, Singla A. Piezocision assisted orthodontics: a new approach to accelerated orthodontic tooth movement. J Innov Dent. 2011; 1.
13. Dibart S, Sebaoun JD, Surmenian J. Piezocision: a minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend Contin Educ Dent. 2009; 30:342–344. 346348–350. PMID: 19715011.
14. Dibart S, Surmenian J, Sebaoun JD, Montesani L. Rapid treatment of Class II malocclusion with piezocision: two case reports. Int J Periodontics Restorative Dent. 2010; 30:487–493. PMID: 20814602.
15. Düker J. Experimental animal research into segmental alveolar movement after corticotomy. J Maxillofac Surg. 1975; 3:81–84. PMID: 1055773.

16. Häsler R, Schmid G, Ingervall B, Gebauer U. A clinical comparison of the rate of maxillary canine retraction into healed and recent extraction sites--a pilot study. Eur J Orthod. 1997; 19:711–719. PMID: 9458604.
17. Yu JY, Lee W, Park JH, Bayome M, Kim Y, Kook YA. Histologic effects of intentional-socket-assisted orthodontic movement in rabbits. Korean J Orthod. 2012; 42:207–217. PMID: 23112952.

18. Han JY, Shin SI, Herr Y, Kwon YH, Chung JH. The effects of bone grafting material and a collagen membrane in the ridge splitting technique: an experimental study in dogs. Clin Oral Implants Res. 2011; 22:1391–1398. PMID: 21435006.

19. Redlich M, Rahamim E, Gaft A, Shoshan S. The response of supraalveolar gingival collagen to orthodontic rotation movement in dogs. Am J Orthod Dentofacial Orthop. 1996; 110:247–255. PMID: 8814024.

Figure 2
Panoramic radiographs showing the treatment progress. A, Pretreatment stage. B, The mandibular left second molar erupted into the oral cavity and maxillary fixed appliance therapy was started in the sixth month of treatment. C, Both the mandibular second premolars were moved mesially to close the spaces between the first and the second premolars bilaterally. D, Posttreatment stage.
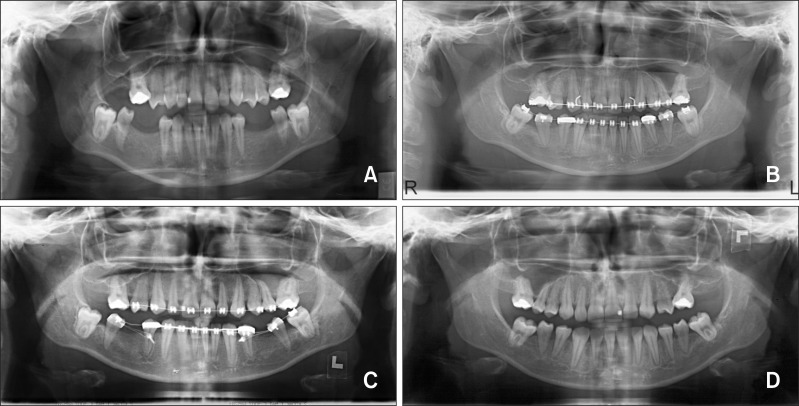
Figure 5
Intraoperative phase. A, Corticotomy lines. B, Cylindrical bone-block placement. C and D, Postsurgical orthodontic mechanics.
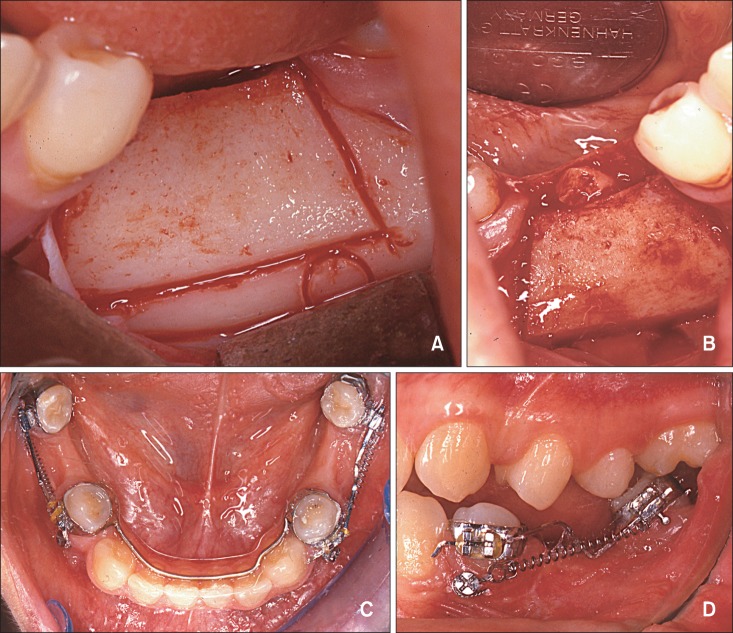
Figure 8
Superimposition of the pretreatment (dotted line) and posttreatment (solid line) cephalometric tracings. A, Maxillary segmental superimposition. B, Mandibular segmental superimposition.
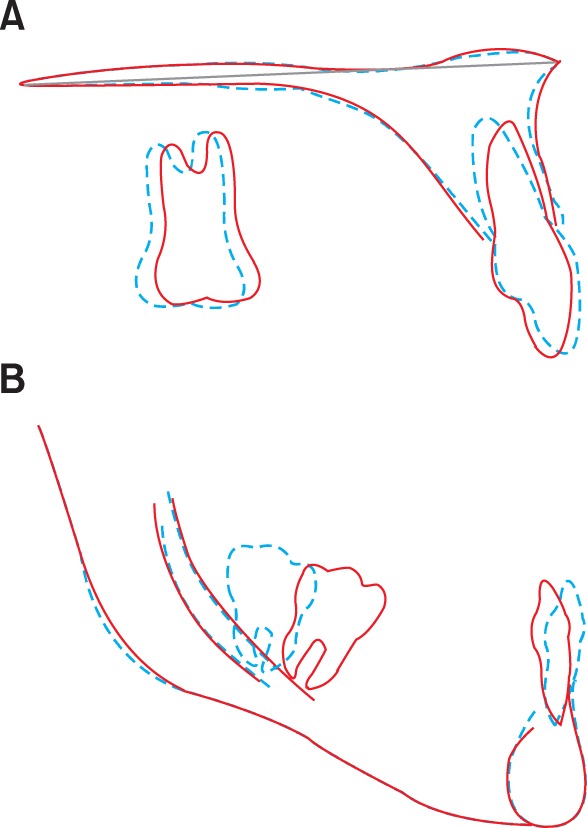
Table 1
Comparison of the pretreatment and posttreatment cephalometric data
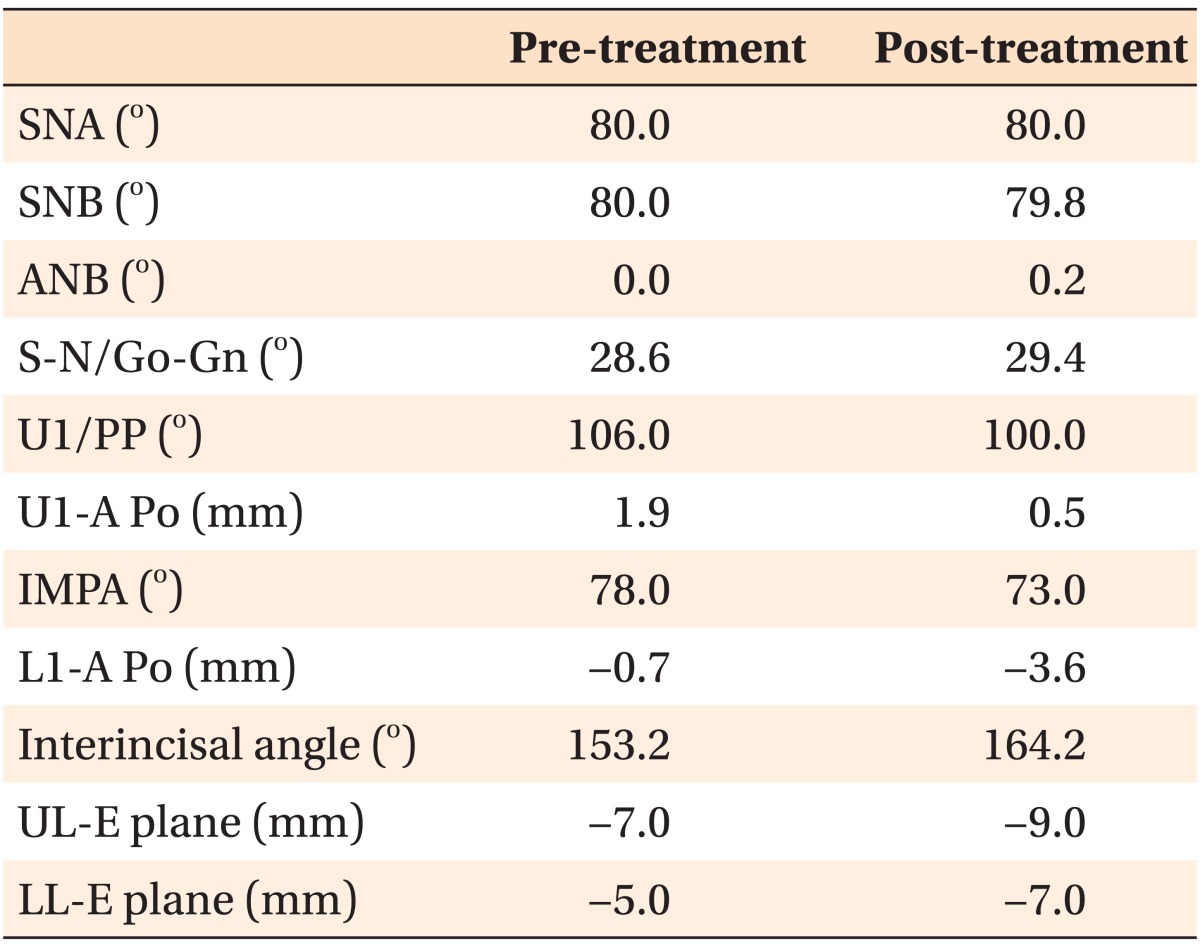
Pre-treatment and post-treatment cephalometric results.
SNA, Sella-nasion-A point angle; SNB, sella-nasion-B point angle; ANB, A point-nasion-B point angle; S-N/Go-Gn, sella-nasion/gonion-gnathion angle; U1/PP, upper incisor/palatal plane angle; U1-A Po, perpendicular distance of upper incisor tip to A-pogonion line; IMPA, incisor mandibular plane angle; L1-A Po, perpendicular distance of lower incisor tip to A-pogonion line; UL-E plane, distance of upper lip to E plane; LL-E plane, distance of lower lip to E plane.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download