Abstract
Objective
In this study, we aimed to examine the relationship between chin deviation and the positional and morphological features of the mandible and to determine the factors that contributed to chin deviation in individuals with a unilateral cleft lip and palate (UCLP).
Methods
Cone-beam computed tomography (CBCT) images of 28 adults with UCLP were analyzed in this study. Segmented three-dimensional temporomandibular fossa and mandible images were reconstructed, and angular, linear, and volumetric parameters were measured.
Results
For all 28 individuals, the chin was found to deviate to the cleft side by 1.59 mm. Moreover, among these 28 individuals, only 7 showed distinct (more than 4 mm) chin deviation, which was toward the cleft side. Compared to the non-cleft side, the mandibular body length, frontal ramal inclination, and vertical position of the condyle were lower and inclination of the temporomandibular fossa was steeper on the cleft side. Furthermore, the differences in inclination of the temporomandibular fossa, mandibular body length, ramus length, and condylar volume ratio (non-deviated/deviated) were positively correlated with chin deviation.
Conclusions
UCLP individuals show mild chin deviation to the cleft side. Statistical differences were noted in the parameters that represented positional and morphological asymmetries of the mandible and temporomandibular fossa; however, these differences were too small to indicate clinical significance.
Facial asymmetry is considered to be one of the typical morphologic characteristics of individuals with a unilateral cleft lip and palate (UCLP).1-8 Several studies have examined facial asymmetry in UCLP individuals, and studies regarding asymmetry of the maxillary dentoalveolar region around the cleft site, specifically, have reported consistent results.1,2 However, studies regarding asymmetry of the mandible have reported inconsistent results.3-8 Using postero-anterior (PA) cephalograms, Laspos et al.4 found that the mandible was distorted in children with UCLP. Smahel and Brejcha6 examined lateral and PA radiographs of 58 UCLP individuals and reported significant shortening of the mandibular body and ramus with changes in the mandibular shape. Kurt et al.7 reported no statistically significant differences in condylar length or ramal length between the cleft and non-cleft sides; in addition, Son and Kim8 measured the ramal length and mandibular-body length on PA radiographs and found no differences in mandibular morphology between the cleft and non-cleft sides. Recently, Veli et al.9 studied CBCT images of UCLP patients and reported symmetrical mandibles.
The inconsistencies between the results of these previous studies could be attributed to the differences among study subjects, study methods (including the setting of the reference plane), type of radiography used to measure the parameters, and limitations of two-dimensional (2D) radiography based measurements. Additionally, these discordant findings can be attributed to the fact that the mandible is not directly affected by the cleft and that the etiology of mandibular asymmetry is multifactorial, including genetic background and environmental factors.4,10
Chin deviation is an important characteristic in the evaluation of facial asymmetry11,12 - it is affected by asymmetries of the mandible, maxilla, and cranial-base structures such as the temporomandibular fossa.13 Although several studies have examined asymmetry of the maxilla in UCLP individals,1,2 few three-dimensional (3D) studies have been conducted on asymmetries of the mandible and the temporomandibular fossa in adults with UCLP. Therefore, to evaluate lower-face asymmetry, in the present study, we measured chin deviation in individuals with UCLP and examined the factors that contribute to chin deviation. In particular, we constructed 3D images using cone-beam computed tomography (CBCT) and measured the position and shape of the mandible and temporomandibular fossa, which is closely associated with the mandible, in these individuals.
The subjects of this study comprised 28 adults with UCLP (17 men, 11 women; mean age: 22 years 8 months, standard deviation [SD]: 6 years 4 months), who had undergone 3D CBCT for the purpose of pre-orthodontic evaluation at Pusan National University Dental Hospital between January 2007 and August 2011. The cleft was located on the left side in 22 individuals and on the right side in 6 individuals (Table 1). Individuals with a history of facial trauma; orthognathic surgeries, including distraction osteogenesis and orthodontic treatment; or degenerative disease of the temporomandibular joint were excluded from this study. This study was reviewed and approved by the Ethics Committee of Pusan National University Hospital (E-2011048).
To evaluate the geometry of the cranial-base and mandibular structures, CBCT scans were acquired using a DCT Pro (Zenith 3D; Vatech, Seoul, Korea), with the following settings: 60 - 90 kVp, 2 - 10 mA, 24 sec scan time, and 20 × 19 cm FOV. The slice thickness was set at 0.3 mm, gray level depth was 14 bit, and the voxel size was 0.3 × 0.3 × 0.3 mm. The CT data were measured using Simplant software (Materialise; Ann Arbor, MI, USA) and stored in a Digital Imaging and Communications in Medicine (DICOM) file format. Soft tissue was removed from the bony structure by thresholding, and the mandible was detached from the skull base by segmentation. On the reconstructed 3D images, all landmarks on the surface of the skeleton were identified using a digitizer.
To establish the standard orientation of the craniofacial structures, 3D reference planes (horizontal, sagittal, and coronal) were initially set. The horizontal plane was defined as the plane that passed through the bilateral porion (Po) and inferior orbitale (Or) on the non-cleft side (Frankfurt plane, FH plane). The sagittal plane was defined as the plane perpendicular to the horizontal plane passing through the basion (Ba) and the crista gali (Cg) (midsagittal reference plane, MSR plane). The plane perpendicular to the FH and MSR planes (including the Ba) was defined as the Ba-perpendicular plane (coronal plane) (Figure 1).
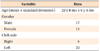
Linear and angular parameters were measured on separate 3D images of the temporomandibular joint and mandible in order to mark the correct positions (Tables 2 and 3).
For the evaluation of lower-face asymmetry, the extent of chin deviation was measured from the menton to the MSR plane, because chin position is an important determinant of facial appearance.11,12,14,15
On separate 3D mandibular images, the ramus length (the distance between the most superior point of the condyle and the most inferior point of the gonion), mandibular body length (the distance between the menton and the most posterior point of the gonion), frontal ramal inclination (FRI, the angle between the midsagittal plane and the lateral ramal line [the line between the most lateral point of the gonion and the condyle]), and lateral ramal inclination (LRI, the angle between the plane perpendicular to the FH plane and the posterior ramal line [the line between the most posterior point of the gonion and the condyle]) were measured (Figure 2).16
The mandibular condyle was separately set, and its position and shape were measured. The lateral and medial poles of the condyle were identified; the distance between them was defined as the condylar width, and the midpoint between them was defined as the condylar center (Cc). The angle between the Ba-perpendicular plane and the condylar axis (the line passing through the medial and lateral poles of the condyle) was measured and defined as the condylar angulation (Figure 3). Furthermore, for measuring the condylar length and volume, a plane perpendicular to the posterior ramal line and passing through the sigmoid notch was drawn and defined as the condylar plane (Figure 4). The mandible above the condylar plane was defined as the mandibular condyle, and the length and volume of the mandibular condyle were measured on both sides.17,18
At the base of the skull, the position, depth, and inclination of the temporomandibular fossa, which is closely associated with the mandibular condyle, were measured. The most superior point of the temporomandibular fossa was defined as the roof of the temporomandibular fossa (RT). Then, the superoinferior (SI) position (the distance between the FH plane and the RT), anteroposterior position (the distance between the coronal plane and the RT), and mediolateral position (the distance between the sagittal plane and the RT) of the temporomandibular fossa were measured on both sides. Furthermore, the distance from the RT to the articular tubercle (AT), parallel to the MSR plane, was measured and defined as the depth of the temporomandibular fossa. In addition, the inclination of the temporomandibular fossa, which is the angle between the FH plane and a line joining the RT to the most inferior point of the AT, was measured (Figure 5).
The data were statistically analyzed using a software program (PASW Statistics 18.0; IBM Co., Armonk, NY, USA). To assess the variability and reproducibility of the results of CBCT analysis, measurements of all the parameters were repeated after 4 weeks. In addition, another examiner measured all of the parameters, and the inter-examiner error was determined. The intraclass coefficient (ICC) was used to assess intra-examiner and inter-examiner agreement. Intra-examiner agreement was excellent (ICC range: 0.946 - 0.988), and inter-examiner agreement represented high reproducibility (ICC range: 0.862 - 0.924).
Subsequently, the Shapiro-Wilk test was conducted to test the normality of the sample (p > 0.05). The differences between the cleft and non-cleft sides were compared by a paired t-test, and p < 0.05 was considered significant. Pearson's correlation analysis and regression analysis were performed to determine the relationship between asymmetries of the temporomandibular fossa and mandible and chin deviation.
Of the 28 subjects, 24 showed chin deviation toward the cleft side and only 4 showed deviation toward the non-cleft side; the mean deviation was 1.59 mm (SD 2.94 mm) toward the cleft side. In addition, only 7 subjects, accounting for 25% of the group, showed a chin deviation of more than 4 mm, which is a significant value with respect to lower-face asymmetry.11 The chin deviations in these 7 individuals were toward the cleft side (Table 4).
The vertical position of the Cc on the cleft side was lower than that on the non-cleft side (p < 0.05). However, the anteroposterior and mediolateral positions of the Cc did not differ between the 2 sides.
Among the morphological parameters of the mandible, the mandibular body length and the FRI were significantly different between the 2 sides (p < 0.05). These 2 parameters were smaller on the cleft side than on the non-cleft side. The characteristics of the ramus length, condylar width, condylar angulation, condylar length, and condylar volume were not significantly different between the 2 sides (Table 5).
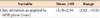
In the temporomandibular fossa area, the vertical position of the temporomandibular fossa was lower on the cleft side than on the non-cleft side (p < 0.05). Moreover, the inclination of the fossa was steeper on the cleft side than on the non-cleft side (p < 0.05), although the depth of fossa did not significantly differ between the 2 sides (Table 6).
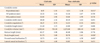
Correlation analysis was performed to investigate the association of mandibular asymmetry with chin deviation in the 28 subjects. Considering that the window-level value appropriate for observation of the condyle varies for each CBCT, the volume ratio (the condyle volume on the non-cleft side/the condyle volume on the cleft side) was used instead of the volume difference. The results of the correlation analysis showed that the differences in the condylar length, condylar volume ratio, mandibular body length, ramus length, and inclination of the temporomandibular fossa were associated with chin position; among all these parameters, the correlation coefficient of the condylar volume ratio was the highest (Table 7).
Multiple regression analysis was conducted to assess the effect of the abovementioned parameters on chin deviation. Comparative analysis of the standardized regression coefficient (β) showed that chin deviation was explained by the differences in the SI position of the Cc, condylar volume ratio, body length, and ramus length (Table 8).
Several studies on UCLP individuals have used 2D radiographs to assess mandibular asymmetry;5-7,10-12 however, only a few have used 3D imaging. Because quantitative measurements are a key element in the diagnosis of asymmetry, 3D structures cannot be appropriately analyzed by using 2D radiography.13 With the development of 3D imaging technology, multiplanar imaging and assessment of 3D data of the maxillofacial region, including the temporomandibular fossa and mandibular condyle, has now become possible.17-21 Three-dimensional reconstruction of CT images can reduce magnification and distortion errors common in 2D radiographs and allow quantitative measurement of structures.22,23
In establishing a reference plane, there are inherent problems due to the external acoustic meatus being a temporal bone landmark that can be affected by deformities. Nevertheless, Kim et al.24 reported that the external acoustic meatus, because it maintains a stable shape, is a suitable reference for analysis of craniofacial asymmetry. Accordingly, we used the external acoustic meatus as a reference when drawing the FH plane.
Our results showed that the mean chin position, which best describes lower-face asymmetry, was deviated to cleft side by approximately 1.59 mm. This result is consistent with that of a study by Son and Kim8, in which the average chin deviation to the cleft side was 1.94°. Generally, lower-face asymmetry is expected to be significant in UCLP individuals, although only 7 of our 28 subjects showed chin deviation greater than 4 mm. Nonetheless, it is important to note that chin deviation in all 7 subjects was to the cleft side. In fact, of the 28 subjects, only 4 showed chin deviation to the non-cleft side. Therefore, we believe that chin position tends to deviate toward the cleft side in UCLP individuals; however, only a few individuals manifest clinically significant deviation.
In the mandible, compared to the non-cleft side, the condyle on the cleft side was located inferiorly by approximately 0.7 mm. Moreover, the mandibular body was shorter and the FRI was smaller on the cleft side than on the non-cleft side. Most of the linear and volumetric parameters were smaller on the cleft side than on the non-cleft side, although only the mandibular-body length and FRI differences were statistically significant. Veli et al.9 examined the mandibles of UCLP individuals using cone-beam CT and reported mandibular symmetry, with the exception of the coronoid unit length. We attribute the differences between this result and our results to the use of different research methods and subjects: their study excluded subjects with chin deviation > 2 mm.
In the temporomandibular fossa area, the RT was inferiorly located on the cleft side. This result is consistent with those of studies conducted by Kyrkanides et al.3 and Laspos et al.4 Moreover, the inclination of the temporomandibular fossa on the cleft side was steeper than that on the non-cleft side. This result is consistent with that of a previous study in which the inclination of the temporomandibular fossa on the deviated side was steeper in patients with mandibular asymmetry.25,26 Further studies must be conducted to clarify whether these differences in the vertical position and inclination of the temporomandibular fossa are caused by remodeling, degenerative changes in the temporomandibular fossa while it adapted to an asymmetric mandible,21,27 or the cranial-base asymmetry of UCLP individuals.
As the location and growth of the mandible is associated with cranial-base structures such as the temporomandibular fossa and the growth direction of the condyle,28 chin deviation to the non-cleft side can be predicted if the temporomandibular fossa on the cleft side is located more inferiorly and if there is no mandibular asymmetry. In the present study, however, no definite chin deviation was shown in 75% of the subjects; indeed, 25% showed deviation toward the cleft side, not the non-cleft side. This result may be attributed to the fact that the difference in the vertical position of the bilateral temporomandibular fossa was clinically insignificant (mean value 0.45 mm); moreover, the anteroposterior and mediolateral positions affected chin deviation. Furthermore, the mandibular-body length and FRI on the cleft side were smaller in this study, which affected chin deviation toward the cleft side. Correlation analysis revealed that most of the factors related to the true mandibular asymmetry were also associated with chin deviation, and the difference in the vertical position of the temporomandibular fossa was less associated with chin deviation.
To confirm that the smaller mandibular-body length and FRI on the cleft side, found in the present study, were caused by mandibular growth in the direction that compensated for the asymmetries of the cranial base and the nasomaxillary complex, or by cleft-related soft tissue problems such as increase in muscular tension attendant on post-operative scarring, further study, for example, on muscle activity and volume, is required.
In our study, although all the parameters were significantly different between the 2 sides, the differences in a few parameters (SI position of RT, SI position of Cc, and mandibular body length) were too small to clinically explain mandibular asymmetry.
For successful orthodontic correction of UCLP, it is important to ascertain the location, range, and severity of craniofacial defects related to the cleft side. The asymmetries of the mandible and temporomandibular fossa can be clinically diagnosed by measuring 3D images of the skull and mandible. If facial asymmetry is observed in a growing patient, asymmetries of the temporomandibular fossa and mandible should be considered in preparing a treatment plan that induces mandibular growth in a direction that compensates for the facial asymmetry. Furthermore, before orthognathic surgery in adult patients with UCLP, a surgery plan should be prepared according to the characteristics of the true mandibular asymmetry.
Asymmetry of the mandible in UCLP individuals has been evaluated by CBCT in few studies. In the present study, we compared the position and morphology of the mandible between the cleft and non-cleft sides in UCLP individuals and evaluated the correlation between structural asymmetries and chin deviation using 3D CBCT images. Our results indicated that UCLP individuals showed chin deviation to the cleft side (1.59 mm), but the deviation was not clinically significant. Only a few subjects (25%) showed significant chin deviation (more than 4 mm) toward the cleft side. Moreover, vertical positions of the temporomandibular fossa (difference: 0.42 mm) and condyle (difference: 0.76 mm) were lower and inclination of the temporomandibular fossa was steeper on the cleft side (difference: 2.77°) than on the non-cleft side. In addition, mandibular-body length (difference: 0.99 mm) and FRI (difference: 3.0°) were smaller on the cleft side. The degree of chin deviation was positively correlated with differences in the temporomandibular fossa inclination, mandibular-body length, ramus length, and condylar volume ratio (non-deviated/deviated). Although these values were statistically significant, the differences were too small to indicate clinical significance.
Figures and Tables
 | Figure 1Three-dimensional reference planes used in this study. A, FH plane and MSR plane. B, Ba-perp. plane.
PoL, Left ponon; PoR, right ponon; OrR, right orbitale.
See Table 2 for the definitions of all other points and planes.
|
 | Figure 2Three-dimensional measurements of mandible. A, Ramus length. B, Mandibular body length. C, Frontal ramal inclination. D, Lateral ramal inclination. See Table 2 for the definitions of all the points, planes, and measurements. |
Table 3
Definitions of the measurements used in this study

See Table 2 for the definitions of all the points and planes.
Table 6
Comparison of the characteristics of the temporomandibular fossa on the cleft/non-cleft sides
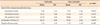
Table 7
Pearson correlation analysis between chin position and characteristics of the temporomandibular fossa and mandible

References
1. Shetye PR, Evans CA. Midfacial morphology in adult unoperated complete unilateral cleft lip and palate patients. Angle Orthod. 2006; 76:810–816.
2. Mølsted K, Dahl E. Asymmetry of the maxilla in children with complete unilateral cleft lip and palate. Cleft Palate J. 1990; 27:184–190.

3. Kyrkanides S, Klambani M, Subtelny JD. Cranial base and facial skeleton asymmetries in individuals with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2000; 37:556–561.

4. Laspos CP, Kyrkanides S, Tallents RH, Moss ME, Subtelny JD. Mandibular asymmetry in noncleft and unilateral cleft lip and palate individuals. Cleft Palate Craniofac J. 1997; 34:410–416.

5. Ishiguro K, Krogman WM, Mazaheri M, Harding RL. A longitudinal study of morphological craniofacial patterns via P-A x-ray headfilms in cleft patients from birth to six years of age. Cleft Palate J. 1976; 13:104–126.

6. Smahel Z, Brejcha M. Differences in craniofacial morphology between complete and incomplete unilateral cleft lip and palate in adults. Cleft Palate J. 1983; 20:113–127.
7. Kurt G, Bayram M, Uysal T, Ozer M. Mandibular asymmetry in cleft lip and palate patients. Eur J Orthod. 2010; 32:19–23.

8. Son WS, Kim MK. Facial asymmetry of unilateral cleft lip and palate patients. Korean J Orthod. 1995; 25:13–18.
9. Veli I, Uysal T, Ucar FI, Eruz M, Ozer T. Cone-beam computed tomography assessment of mandibular asymmetry in unilateral cleft lip and palate patients. Korean J Orthod. 2011; 41:431–439.

10. Bishara SE, Burkey PS, Kharouf JG. Dental and facial asymmetries: a review. Angle Orthod. 1994; 64:89–98.
11. Ahn JS, Hwang HS. Relationship between perception of facial asymmetry and posteroanterior cephalometric measurements. Korean J Orthod. 2001; 31:489–498.
12. Lee GH, Cho HK, Hwang HS, Kim JC. Studies of relationship between P-A cephalometric measurements and vidual facial asymmetry. Korean J Phys Anthropol. 1998; 11:41–48.

13. Hwang HS, Hwang CH, Lee KH, Kang BC. Maxillofacial 3-dimensional image analysis for the diagnosis of facial asymmetry. Am J Orthod Dentofacial Orthop. 2006; 130:779–785.

14. Haraguchi S, Takada K, Yasuda Y. Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 2002; 72:28–35.
15. Michiels G, Sather AH. Determinants of facial attractiveness in a sample of white women. Int J Adult Orthodon Orthognath Surg. 1994; 9:95–103.
16. Hwang HS. Maxillofacial 3-dimensional image analysis for the diagnosis of facial asymmetry. J Korean Dent Assoc. 2004; 42:76–83.

17. Hilgers ML, Scarfe WC, Scheetz JP, Farman AG. Accuracy of linear temporomandibular joint measurements with cone beam computed tomography and digital cephalometric radiography. Am J Orthod Dentofacial Orthop. 2005; 128:803–811.

18. Schlueter B, Kim KB, Oliver D, Sortiropoulos G. Cone beam computed tomography 3D reconstruction of the mandibular condyle. Angle Orthod. 2008; 78:880–888.

19. Christiansen EL, Chan TT, Thompson JR, Hasso AN, Hinshaw DB Jr, Kopp S. Computed tomography of the normal temporomandibular joint. Scand J Dent Res. 1987; 95:499–509.

20. Kobayashi F, Matsushita T, Hayashi T, Ito J. A morphological study on the temporomandibular joint using X-ray computed tomography: relation to anterior disk displacement. Dent Radiol. 1996; 36:73–80.
21. Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol. 2004; 33:196–201.

22. Bergersen EO. Enlargement and distortion in cephalometric radiography: compensation tables for linear measurements. Angle Orthod. 1980; 50:230–244.
23. Fuhrmann RA, Schnappauf A, Diedrich PR. Three-dimensional imaging of craniomaxillofacial structures with a standard personal computer. Dentomaxillofac Radiol. 1995; 24:260–263.

24. Kim YH, Sato K, Mitani H, Shimizu Y, Kikuchi M. Asymmetry of the sphenoid bone and its suitability as a reference for analyzing craniofacial asymmetry. Am J Orthod Dentofacial Orthop. 2003; 124:656–662.

25. Cho JH, Lee KM, Park HJ, Hwang HS. 3-D CT image study of effect of glenoid fossa on menton deviation. J Korean Assoc Maxillofac Plast Reconstr Surg. 2011; 33:337–345.
26. Kawakami M, Yamamoto K, Inoue M, Kawakami T, Fujimoto M, Kirita T. Morphological differences in the temporomandibular joints in asymmetrical prognathism patients. Orthod Craniofac Res. 2006; 9:71–76.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download