Abstract
This article describes the orthodontic treatment of a 31-year-old Korean female patient with gummy smile and crowding. The patient showed excessive gingival display in both the anterior and posterior areas and a large difference in gingival heights between the anterior and posterior teeth in the maxilla. To correct the gummy smile, we elected to intrude the entire maxillary dentition instead of focusing only on the maxillary anterior teeth. Alignment and leveling were performed, and a midpalatal absolute anchorage system as well as a modified lingual arch was designed to achieve posterosuperior movement of the entire upper dentition. The active treatment period was 18 months. The gummy smile and crowding were corrected, and the results were stable at 21 months post-treatment.
In 1983, Creekmore and Eklund1 reported using a metal implant to correct a deep overbite. They placed a surgical vitallium bone screw just below the anterior nasal spine and used elastic thread to elevate the maxillary central incisors by approximately 6 mm while tipping them 25° labially, without causing infection, pain, or other complications from the screw. However, they cautioned that widespread use of this technique would be premature.
Recently, mini-implants have been used to correct gummy smiles or deep overbites through intrusion of the upper incisors.2,3 In 2006, Kim et al.2 applied a segmental intrusive force between the maxillary central incisors by using a mini-implant with segmented wires. In 2010, Lin et al.3 introduced a combined approach using skeletal anchorage to simultaneously control the vertical dimension and to resolve gummy smiles of skeletal origin in adult long-faced patients.
This case report presents the orthodontic treatment of an adult patient whose gummy smile was corrected by intruding the entire maxillary dentition using a midpalatal absolute anchorage system (MAAS) and a modified lingual arch.
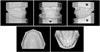
A 31-year-old Korean female patient was concerned about her gummy smile. She showed excessive gingival display in both the anterior and posterior areas, occlusal canting upon smiling, a straight profile, and facial asymmetry from the frontal view (Figure 1). There was no interlabial gap at the resting lip position. The study model revealed bilateral Class I canine and molar relationships with a 3.5 mm overbite, 3.0 mm overjet, and a 1.5 mm midline discrepancy between the maxilla and mandible (Figure 2). There were 0 mm and 1.3 mm arch length discrepancies in the maxillary and mandibular arches, respectively. The patient had no history of trauma or severe disease and no pathologic signs were found within the temporomandibular joint or in the mouth.
Cephalometric evaluation showed a skeletal Class I relationship, a large upper anterior dental height (Is-Is', distance from the incisal edge of the upper central incisor to the palatal plane), and a significantly decreased mandibular plane angle (Figure 3 and Table 1). With reference to the Frankfurt horizontal plane, the upper incisors were within normal limits and the lower incisors were flared.
Our treatment goals consisted of improving the patient's smile esthetics while providing a harmonious occlusion. The treatment objectives included reducing her excessive gingival display, creating a normal overbite and overjet relationship, correcting the dental midline discrepancy, and relieving crowding.
Botulinum toxin type A injections were considered for correction because the patient's gummy smile seemed to be a result of hyperactivity of the elevator muscles of the upper lip. However, this neuromuscular approach for correction was rejected because of the transitory nature of the results. Orthodontic treatment was selected instead.
This patient showed excessive gingival display in both the anterior and posterior areas with a large difference in the gingival heights between the maxillary anterior and posterior teeth. To correct the gummy smile, therefore, we decided to intrude the entire upper dentition instead of focusing only on the upper anterior teeth.
Two treatment options were discussed with the patient. The first was traditional orthodontic treatment combined with Le Fort I surgery to reduce the maxillary height, which would, in turn, reduce the gingival exposure. The second option was orthodontic intrusion of the entire maxillary dentition using miniscrew skeletal anchorage. After a review of the risks and benefits of the two options, the patient chose the latter more conservative method.
The patient was eager to use an invisible orthodontic appliance during the entire treatment period. Therefore, for alignment and leveling, removable clear aligners and lingual brackets were used for the maxilla and mandible, respectively. A screw implant and a modified lingual arch were then used for total intrusion of the maxillary arch.
Fujita lingual brackets were bonded indirectly from the mandibular first molar to first molar, and 0.018-inch slot standard edgewise appliances were placed on the buccal surfaces of the mandibular first and second molars.4,5 A progression through mushroom archwires was initiated, starting with 0.012-inch nickel titanium wire in the occlusal slots of the lingual brackets, and 0.016- × 0.022-inch stainless steel segmental wires were engaged in the buccal standard edgewise appliances. For 5 months, alignment of the mandibular teeth progressed with gradual increases in archwire sizes. After alignment, the lower dental midline shift to the left side had improved, probably because there was more crowding in the left anterior region of the mandible.
For correction of the rotated maxillary right and left lateral incisors, 5 clear aligners made of 0.5 mm Essix A+ (Dentsply, Bradenton, FL, USA) were fabricated and delivered to the patient. After delivery of the fourth aligner, composite resin was added on the mesiolingual surface of the maxillary right lateral incisor. The purpose of the added resin was to facilitate rotation of the lateral incisor. After 5 months of treatment with clear aligners, a clear retainer was used until placement of the modified lingual arch in the maxilla.
After the initial alignment phase, there were occlusal interferences between the modified lingual arch of the maxilla and the mandibular anterior teeth (Figure 4A). Thus, we decided to apply modified intrusive mechanics with a lingual segmented-arch technique6 to open the bite via intrusion of the six mandibular anterior teeth (Figure 5).
After four months of intrusion of the six mandibular anterior teeth, the MAAS was designed to achieve posterosuperior movement of the maxillary dentition using the safe-multifunctional-solid (SMS) screw (BioMaterials Korea Inc., Seoul, Korea) in conjunction with a modified lingual arch (Figure 6). The SMS screw (Figure 7) was implanted at the intersection of a line extending between the upper right and left first molars and the midpalatal suture. An appropriate power arm fabricated with a 0.032- × 0.032-inch stainless steel wire was fixed onto the implanted SMS screw head with a ligature wire. A 0.9 mm stainless steel modified lingual arch appliance, with hooks at the canines and first molars, was bonded from second molar to second molar in the maxillary arch. An elastomeric chain was then suspended from the power arm to the hook on the modified lingual arch, with a force magnitude of 200 to 250 g. A total force of 800 to 1,000 g was applied for 9 months to the maxillary arch.
After an 18-month treatment period, all fixed appliances and the screw implant were removed. As an effective method of retention after intrusion treatment has not yet been developed, a circumferential removable retainer was delivered in the maxilla. For the mandible, a 0.0175-inch multistranded stainless steel lingual fixed retainer was bonded from canine to canine.
The patient's smile esthetics were improved with a harmonious occlusion at the end of treatment (Figures 8 and 9). A Class I occlusion was achieved, and the overbite and overjet were overcorrected to an edge-to-edge bite (Figure 10). The maxillary and mandibular dental midlines were coincident with each other.
Overall superimposition of cephalometric tracings showed posterosuperior movement of the maxillary dentition with little skeletal change (Figure 11). In a regional superimposition, the lower incisors were intruded with a slight proclination while the lower molars were extruded. As a result, the mandible did not rotate counterclockwise. No marked root resorption was seen in the panoramic radiograph (Figure 12).
At the retention visit, the patient reported that she was not compliant with the maxillary removable retainer; however, the 21-month retention records showed good stability without obvious relapse (Figures 13, 14, and 15).
The reasons for a gummy smile include excessive maxillary vertical growth, over-eruption of the maxillary incisors, incomplete anatomic crown exposure, hyperactivity of the elevator muscles of the upper lip, or a combination of these factors.7-9 A gummy smile of skeletal origin requires orthognathic surgery for correction. Dentoalveolar gummy smiles caused by over-eruption of the maxillary incisors can be corrected by intruding the extruded maxillary incisors. The dentogingival type of gummy smile is related to abnormal dental eruption or lack of gingival recession and requires lengthening of the anatomic crown. The neuromuscular type of gummy smile is caused by hypercontractibility or excessive muscle contraction and can be improved temporarily by injecting botulinum toxin type A. As lip incompetency was not observed in this patient, the gummy smile seemed to be a result of hyperfunctional upper lip elevator muscles and was improved using an orthodontic approach mimicking Le Fort I maxillary impaction surgery.
The use of screw mechanics for achieving the effect of a Le Fort I impaction of the maxilla was proposed by Lin et al.,3 in which multiple screws are necessary: two miniscrews (diameter, 2 mm; length, 7 mm) are placed between the roots of the maxillary second premolars and first molars on both sides; two hook screws (diameter, 1.5 mm; length, 9 mm) are inserted into the buccal alveolus between the maxillary first and second molars on both sides; and two hook screws (diameter, 2 mm; length, 7 mm) are placed in the paramedian palatal area 2 mm from the midpalatal suture, near the imaginary midline between the maxillary first and second molars.
In this case report, MAAS using the SMS screw implant accomplished the effect of a Le Fort I impaction of the maxilla with the aid of a modified lingual arch. The SMS screw withstood quite heavy orthodontic forces. An appropriately formed 0.032- × 0.032-inch stainless steel power arm was fixed to the head of the SMS screw and provided the force application points for the required absolute anchorage without using multiple screws. We propose that the MAAS used in this case is a minimally invasive alternative orthodontic approach that mimics Le Fort I maxillary impaction surgery.
The center of resistance of the unit to be moved is the basic point around which the arrangement of a force system is established. By using the center of resistance for the maxillary dentition from second molar to second molar, as defined by Billiet et al.,10 various force systems for maxillary postero-superior intrusion can be established and a number of different clinical situations may arise. If the postero-superior intrusion force passes anterior to the center of resistance for the maxillary dentition, the anterior teeth will intrude more than the posterior teeth and an anterior open bite will occur. On the contrary, if the postero-superior intrusion force is applied posterior to the center of resistance for the maxillary dentition, more intrusion of the posterior than the anterior teeth is generated, resulting in a posterior open bite. The line of action of the postero-superior intrusive force through the center of resistance for the maxillary dentition will generate uniform intrusion in both anterior and posterior teeth. However, in clinically practice, it is difficult to precisely establish the line of action of the postero-superior intrusive force through the center of resistance for the maxillary dentition. Therefore, in this case, both the positioning of the hooks on the modified lingual arch and the shape of the power arm were determined using a lateral cephalogram, so that the applied anterior and posterior forces would move the upper arch posteriorly and superiorly with respect to the center of resistance of the entire upper dentition (Figure 16). In addition, the magnitude of the anterior and posterior forces was adjusted so as not to rotate the maxillary dentition clockwise or counterclockwise. As a result, uniform intrusion of both anterior and posterior teeth occurred with no anterior or posterior open bite resulting during postero-superior intrusion of the maxillary dentition.
In a lingual force system, the intrusive force is applied close to the center of resistance of the lower anterior teeth because of the position of the lingual brackets in relation to the center of the tooth (Figure 17), and the anterior teeth are well intruded with little flaring. However, the lower incisors were intruded with slight proclination in this case. Slight proclination of the lower incisors seemed to occur during alignment because the lower anterior teeth were aligned for five months prior to the intrusive mechanics.
The median and paramedian areas of the posterior palate consist of cortical bone, which is thick and dense enough to support screw implants and can sustain heavy orthodontic forces. These areas have no anatomical structures such as nerves, blood vessels, or roots that can impede the placement of screw implants. Furthermore, most of the soft tissue is keratinized and thinner than 1 mm. Therefore, the posterior region of the mid-palatal suture is safe and solid for inserting screw implants.
Because the histomorphology of the palate shows that the median palatal region is the best location for orthodontic implants, many osseointegrated implants have been used for palatal anchorage.11-13 However, these systems require a waiting period of over two weeks - immediate loading is impossible - and the methods of placement and removal of the implant are rather complicated and time consuming, as well as costly for the patient, because they require surgical intervention.
Recently, miniscrews have been widely used in palatal skeletal anchorage because they are relatively easy to insert and remove, and force can be applied to them almost immediately.14-16 These devices have demonstrated potential for direct or indirect skeletal anchorage to move individual teeth. As shown in this case report, however, the MAAS using the SMS screw can drive heavy orthodontic forces to move whole dental arches in any direction with the assistance of a power arm.
With the advent of absolute anchorage, it has become feasible to perform orthodontic intrusion of the maxillary posterior teeth for correction of the anterior open bite. A number of studies17-19 showed little disparity between orthodontic and surgical approaches, and reported that relapse occurred in most cases during the first year of retention. However, because there is no effective way to retain an intruded tooth, a tooth displaced intrusively is much less stable than one displaced either mesiodistally or rotationally.20 Therefore, each case should be carefully evaluated while considering strategies to improve stability, such as slow intrusive movement, overcorrection, longer retention periods, and active retention methods. Although this patient had not worn the maxillary circumferential removable retainer, the results were stable at 21 months post-treatment. This seemed likely due to slow intrusive movement (9 months) of the maxillary arch.
The MAAS can correct gummy smiles by total intrusion of the maxillary arch and has several advantages: it is a minimally invasive treatment modality that reduces the number of screw implants needed, it withstands heavy orthodontic forces and provides orthodontic forces in any required direction.
Figures and Tables
Figure 4
Photographs of bite opening before (A) and after (B) intrusion of the six mandibular anterior teeth.

Figure 5
Modified intrusive mechanics in the lingual segmented-arch technique. In the occlusal slots of the anterior and posterior lingual brackets, 0.018- × 0.018-inch stainless steel segmental wires were engaged. Additionally, 0.017- × 0.025-inch titanium-molybdenum-aluminum intrusion springs were engaged in the inner lingual slots of the first molar brackets and hooked to the anterior segment between the lateral incisors and canines to intrude the six mandibular anterior teeth.
IS, Intrusive spring; AS, anterior segment; PS, posterior segment; BSS, buccal stabilizing segment.

Figure 6
Midpalatal absolute anchorage system for postero-superior movement of the maxillary dentition. A, Orthodontic force was applied postero-superiorly to the maxillary arch by attaching power chains from the hooks of the power arm to the spurs on the modified lingual arch; B, close-up view.
SMS, Safe-multifunctional-solid screw; M-LA, modified lingual arch; PA, power arm; PC, power chain.

Figure 7
Dimensions of the safe-multifunctional-solid (SMS) screw implant. The SMS screw has a hexagonal head with two cross-shaped 0.032- × 0.032-inch slots. Its diameter is 2 mm and the available lengths are 4 and 5 mm, which can be varied depending on the thickness of the mucosa in the insertion area.

Figure 9
Before (A) and after (B) postero-superior movement of the maxillary dentition. Gummy smile was improved because of the postero-superior movement of the maxillary dentition. Note the decreased distance from the hooks of the power arm to the spurs on the modified lingual arch.
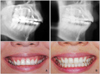
Figure 11
Pretreatment and posttreatment cephalometric superimposition. A, Overall superimposition on the Sella-Nasion plane at Sella; B, regional superimpositions on the palatal plane at ANS and on the mandibular plane at Menton.

Figure 15
Posttreatment and 21-month retention cephalometric superimposition. A, Overall superimposition on the Sella-Nasion plane at Sella; B, regional superimpositions on the palatal plane at ANS and on the mandibular plane at Menton.

Figure 16
Cephalometric radiograph taken after the midpalatal absolute anchorage system was placed in situ. CR, Collective center of resistance of the maxillary dentition; LAIF1, the line of action of the postero-superior orthodontic force distal to the center of resistance of the maxillary arch; LAIF2, the line of action of the postero-superior orthodontic force mesial to the center of resistance of the maxillary arch.
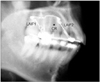
Figure 17
The effect of bracket position and location of the point of force application on tooth movement. In the labial system, the intrusive force against the incisors is applied anterior to the center of resistance and therefore the incisors tend to tip forward as they intrude. Lingual intrusive force is applied close to the center of resistance of the incisors and the incisors are well intruded with little flaring. The possibility of flaring of the incisors is lower with lingual than labial mechanisms.
CR, Center of resistance; Fa, labial intrusive force; Fb, lingual intrusive force; m and M, moment.

Table 1
Cephalometric summary
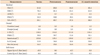
SNA, Sella-nasion-A point; SNB, sella-nasion-B point; ANB, A point-nasion-B point; FMA, Frankfurt-mandibular angle; NPo, nasion-pogonion; FH, Frankfurt plane; FMIA, Frankfurt-mandibular incisor angle; Is-Is', distance from the incisal edge of the upper central incisor to the palatal plane; Mo-Ms, distance from the buccal cusp tip of the upper first molar to the palatal plane.
References
1. Creekmore TD, Eklund MK. The possibility of skeletal anchorage. J Clin Orthod. 1983. 17:266–269.
2. Kim TW, Kim H, Lee SJ. Correction of deep overbite and gummy smile by using a mini-implant with a segmented wire in a growing Class II Division 2 patient. Am J Orthod Dentofacial Orthop. 2006. 130:676–685.

3. Lin JC, Liou EJ, Bowman SJ. Simultaneous reduction in vertical dimension and gummy smile using miniscrew anchorage. J Clin Orthod. 2010. 44:157–170.
4. Hong RK, Sohn HW. Update on the Fujita lingual bracket. J Clin Orthod. 1999. 33:136–142.
5. Hong RK, Kim YH, Park JY. A new customized lingual indirect bonding system. J Clin Orthod. 2000. 34:456–460.
6. Hong RK, Kim TG, Lim SM, Lee CH. Modified intrusive mechanics in lingual segmented-arch treatment. J Clin Orthod. 2005. 39:489–495.
7. Robbins JW. Differential diagnosis and treatment of excess gingival display. Pract Periodontics Aesthet Dent. 1999. 11:265–272.
9. Redlich M, Mazor Z, Brezniak N. Severe high Angle Class II Division 1 malocclusion with vertical maxillary excess and gummy smile: a case report. Am J Orthod Dentofacial Orthop. 1999. 116:317–320.

10. Billiet T, de Pauw G, Dermaut L. Location of the centre of resistance of the upper dentition and the nasomaxillary complex. An experimental study. Eur J Orthod. 2001. 23:263–273.

11. Wehrbein H, Feifel H, Diedrich P. Palatal implant anchorage reinforcement of posterior teeth: A prospective study. Am J Orthod Dentofacial Orthop. 1999. 116:678–686.

12. Byloff FK, Kärcher H, Clar E, Stoff F. An implant to eliminate anchorage loss during molar distalization: a case report involving the Graz implant-supported pendulum. Int J Adult Orthodon Orthognath Surg. 2000. 15:129–137.
13. Bernhart T, Freudenthaler J, Dörtbudak O, Bantleon HP, Watzek G. Short epithetic implants for orthodontic anchorage in the paramedian region of the palate. A clinical study. Clin Oral Implants Res. 2001. 12:624–631.

14. Kyung SH, Hong SG, Park YC. Distalization of maxillary molars with a midpalatal miniscrew. J Clin Orthod. 2003. 37:22–26.
15. Lee JS, Kim DH, Park YC, Kyung SH, Kim TK. The efficient use of midpalatal miniscrew implants. Angle Orthod. 2004. 74:711–714.
16. Park HS. A miniscrew-assisted transpalatal arch for use in lingual orthodontics. J Clin Orthod. 2006. 40:12–16.
17. Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2007. 132:599–605.

18. Lee HA, Park YC. Treatment and posttreatment changes following intrusion of maxillary posterior teeth with miniscrew implants for open bite correction. Korean J Orthod. 2008. 38:31–40.

19. Baek MS, Choi YJ, Yu HS, Lee KJ, Kwak J, Park YC. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010. 138:396.e1–396.e9.

20. Ohtani N. A study of the relapse movement of the intruded teeth and the effects of mechanical retention and gingival transection (author's transl). Nihon Kyosei Shika Gakkai Zasshi. 1980. 39:390–406.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download