This article has been
cited by other articles in ScienceCentral.
Abstract
In this report, we present the case of a girl with delayed odontogenesis of a lower second premolar for which she was followed up for 8.5 years. Congenital absence of permanent mandibular second premolars was observed at the initial radiographic examination at 8 years and 1 month. One year later, during the treatment period, an unexpected odontogenesis of a right second premolar was diagnosed on follow-up radiography. The original treatment plan was revised and a new plan was successfully implemented. Th is unusual case showed that the orthodontist's clinical philosophy must be flexible because unexpected situations can arise, especially when treating growing patients.
Keywords: Agenesis, Dentofacial anomalies, Diagnosis and treatment planning, Pediatric dentistry
INTRODUCTION
The terms congenitally missing, absence, developmental hypodontia, and tooth agenesis are all expressions used to describe the failure of 1 to 5 permanent teeth to form; this is a relatively common occurrence with an incidence of 3 - 8% in the general population.
1,
2 With the exception of third molars, the most frequently observed missing teeth are mandibular second premolars and maxillary lateral incisors. However, one outstanding question remains. When should the final agenesis diagnosis decision be given? To answer this question, orthodontists must know the developmental stages of the permanent dentition.
Odontogenesis of second premolars has been reported to show greater variability than other permanent teeth.
2,
3 While Moorrees et al.
4 showed that the calcification of second premolars are initiated between 2 and 2.5 years of age, Nolla
5 reported that the crypt of mandibular second premolars is usually apparent at 3 years of age. The results of another longitudinal study indicated that second premolar formation is initiated at 3 - 3.5 years of age in most cases.
6 Because of the large variability in odontogenesis, an orthodontist should ideally wait until a patient is 5 - 6 years old before giving the final agenesis diagnosis decision for mandibular second premolars.
Treatment of congenital tooth absence consists of 2 main treatment options: the first option involves replacing the residual space with implants or fixed prostheses and closing the spaces by moving the adjacent teeth into the residual space; the second option is to retain the deciduous tooth if its roots seem adequate, but modify its morphology if necessary. However, if the second op tion is chosen, orthodontists must keep in mind that prosthesis will have to be constructed anyway if the root of a deciduous tooth resorbs later in life. If not contraindicated, closing the space between missing teeth with the patient's own teeth is the most preferable option for both orthodontist and the patient. When this option is chosen, the orthodontist may perform this treatment without hesitation, including the extraction of the mandibular second deciduous molars to permit mesial drift of the first permanent molars spontaneously or orthodontically if the patient is over 6 years old. However, the risk involved in this treatment approach is presented in this case report that demonstrates how we approached orthodontic treatment in an 8.5-year follow-up study of an 8-year-old girl exhibiting late odontogenesis of a mandibular right second premolar.
DIAGNOSIS AND ETIOLOGY
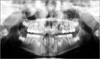
A female patient aged 8 years and 1 month was referred to the Department of Orthodontics in the Faculty of Dentistry at Cumhuriyet University with a major complaint of maxillary anterior crowding. A detailed intraoral examination revealed that the patient was in early deciduous dentition and had a well-aligned mandibular arch and class II molar relationship on both sides; additionally, her maxillary left lateral incisor was in cross-bite. A panoramic radiograph showed that the permanent mandibular second premolars were absent (
Figure 1), and lateral cephalometric evaluations revealed that the patient had a slightly high vertical growth pattern (
Table 1).
TREATMENT OBJECTIVES
The main treatment plan included the following objectives: obtaining a functional occlusion, correcting the cross-bite of the maxillary lateral incisor, and closing the mandibular deciduous second molar space by mesial movement of the permanent first molars.
TREATMENT ALTERNATIVES
Two different treatment alternatives were considered during the case evaluation. The first alternative was to retain the deciduous second molars, as the roots were adequate, and to distalize the maxillary first molars to achieve a class I molar relationship in addition to correcting the cross-bite of the maxillary left lateral incisor. However, the patient had a vertical growth pattern; if the roots of deciduous second molars would resorb later in life, then the residual space would need to be rehabilitated with an implant prosthesis. The second alternative involved the extraction of the deciduous second molars followed by mesialization of the permanent first molars into the extraction space, despite the prolonged treatment time to move the first permanent molar about 8 mm. In this second treatment plan, a class III molar relationship would be established. The case was evaluated in detail and the options were proposed to her parents; finally, the second alternative was chosen considering the vertical growth pattern of the patient and the cost of the implant prosthesis.
TREATMENT PROGRESS
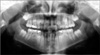
Deciduous second molar extractions were delayed because the patient was in early mixed dentition. The cross-bite of the maxillary left lateral incisor was corrected by using a removable appliance, including a labiolingual spring, for 2 months. The patient was then followed up every 4 months. Interestingly, a developing mandibular right second premolar was clearly observed on a panoramic radiograph approximately 17 months later when the patient was 9 years and 6 months old (
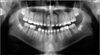
Figure 2). The germ of the maxillary left third molar was also seen at the same time. Following this development, we revised the treatment plan and decided to wait for possible odontogenesis of the permanent left premolar as well as evaluate the calcification process of the right premolar. While there was no evidence of mandibular left second premolar odontogenesis at 2 years after the first appointment (when the patient was 10 years and 2 months old), calcification of the maxillary right third molar and crypt formation of the mandibular right third molar were observed (
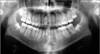
Figure 3). However, at this time the deciduous left second molar roots had resorbed, even though its successor was absent. Three years and 2 months after the first appointment, the mandibular left third molar's crypt formation was observed in addition to advancement of the other third molars and calcification of the mandibular right second premolar. Because the formation of all third molars occurred and there was no evidence of mandibular left second premolar odontogenesis, we considered this premolar to be congenitally absent. Following the revised treatment plan, the deciduous left second molar was extracted and the permanent left first molar was allowed to drift mesially (
Figure 4). In addition, the maxillary left permanent second premolar was also extracted to establish a class I molar relationship. A removable appliance was constructed for both the lower and upper arch, and necessary adjustments were made to achieve parallel movement. After all permanent teeth reached occlusion, except the third molars and mandibular right second premolar, 0.018-inch slot Roth prescription brackets (American Orthodontics) were placed on both arches; leveling started with 0.012-inch nickel-titanium archwires. The spaces were closed, midlines were corrected, class I molar and canine relationships were achieved, and growth pattern remained almost stable after 19 months of fixed appliance therapy (
Table 1). The mandibular right second premolar became exposed within the oral cavity 7 years and 4 months after the initial appointment (
Figure 5) and reached occlusion 15 months after first exposure (
Figure 6).
DISCUSSION
Previous studies have revealed that mandibular second premolars exhibit the greatest variations in differentiation and calcification among all teeth, except for the third molars.
2,
3 Calcification of these teeth usually begins approximately 2 - 2.5 years of age, with 2 standard deviations at less than 3.5 - 4 years of age; crown formation is usually completed by 6 - 8 years.
4 However, the calcification of mandibular second premolars at approximately 5 - 6 years of age is not a rare condition.
6,
7 Second premolar agenesis can usually be confirmed when the patient is 8 - 9 years of age, because reasonably few second premolars form after this age.
6
In the case presented here, initial radiographs showed that the mandibular second premolars were absent when the girl was 8 years and 1 month old. However, we observed that this patient unexpectedly developed late formation of the right second premolar at almost 10 years of age. According to our assessment at that time, we could not presume the possibility of this late formation of second premolars in an 8-year-old girl. Moreover, we were not surprised to find that the patient did not develop second premolars beneath the mandibular second deciduous molars at this age because that is the con genital tooth absence most commonly seen in this region. Consequently, we created a treatment plan that included the extraction of deciduous second molars and mesialization of permanent first molars. Fortunately, this treatment procedure was never followed through; because of the late formation of the right second premolar observed at a subsequent follow-up, and the treatment plan was revised.
In cases where there is an absence of a successor tooth, Lindqvist
8 recommends extraction of the retained mandibular deciduous second molar within the period between 8 years of age and completion of root development for the first permanent molar in order to obtain maximum space closure by bodily drift of the adjacent teeth. However, in a few cases, such as the one reported here, this approach might induce irreversible consequences is the overlying deciduous teeth is not retained until the roots of the successor teeth have formed.
Delay in tooth formation is considered a milder representation of tooth agenesis.
9-
11 One study revealed that, compared to the control group, a group of children affected by hypodontia experienced a significant delay in dental development.
12 Moreover, Rune and Sarnäs
13 presented data suggesting a tendency toward excessive retardation of tooth formation in teeth contralateral to missing teeth. However, a tooth contralateral to the late-developed second premolar was not formed in the case presented in our study.
Studies investigating the genetic and molecular genetic causes of agenesis have begun to identify genes important in tooth agenesis.
9 The transcription factor genes
MSX1 and
PAX9 were the first genes identified for nonsyndromic tooth agenesis.
14,
15 Although both genes affect third molars, a significantly higher frequency of agenesis associated with mutations in
MSX1 than in
PAX9 has been found for second premolars and maxillary first premolars.
9 Third molar agenesis was suggested to be a complex anomaly that may be related to delayed calcification of posterior teeth.
16 However, in the case presented here, all third molars were developed; consequently, this situation demonstrated that there was no association between the developmental absence of third molars and the delayed formation or agenesis of the second premolar. This finding was similar to the results presented by previous case reports.
17-
19 These findings therefore suggest that the cause of the delayed formation of the mandibular right second premolar with a congenital absence of a contralateral premolar might be the result of
MSX1 mutation.
Overall, this case demonstrated that orthodontists should always be aware that unusual circumstances can occur, especially when treating growing patients. To reduce the risk of misdiagnosis, panoramic and periapical radiographs should be carefully evaluated. Furthermore, periapical radiographs should be taken at regular intervals every 6 months in growing patients exhibiting tooth agenesis.
CONCLUSION
Orthodontists should be aware that late tooth formation can occur. Consequently, follow-up radiography should be performed prior to giving a final hypodontia diagnosis decision, especially after deciduous second molar extraction but before space closure.







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download