Abstract
Objective
The purpose of this study was to investigate the antimicrobial effect of silverized elastomers on mutans streptococci in dental plaque.
Methods
Forty patients undergoing orthodontic treatment were randomly placed into 1 of 2 groups. We examined the maxillary right and left central incisors and premolars, and the mandibular right and left canines of all participants. We ligated the right maxillary and left mandibular teeth of the participants in group 1 with silverized elastomers and ligated their contralateral teeth with conventional elastomers. We ligated the left maxillary teeth and right mandibular teeth of group 2 participants with silverized elastomers. Each participant visited the clinic 4 times at 3-week intervals. We applied the elastomers to the teeth on one side of each patient's mouth during their first visit. During the second visit, the elastomers were removed for microbiological analysis and replaced with steel ligatures. During the third visit, we used silverized elastomers to ligate the teeth contralateral to those treated on the first visit. The elastomers were removed during the fourth visit, and microbiological analyses were performed. We compared the quantity of bacteria on silverized and conventional elastomers at the 0.05 level of significance.
Placement of fixed orthodontic appliances leads to in creased plaque accumulation and proliferation of cariogenic pathogens such as Streptococcus mutans (S. mutans).1,2 These changes may be responsible for decalcification or white spot lesions that lead to incipient caries during orthodontic treatment.3
Various orthodontic materials that contain or release fluoride and that were designed to have an antimicrobial effect on cariogenic pathogens have been used as preventive measures against demineralization and white spot lesions.4 However, the timing and amount of fluoride released by these devices in the oral environment are questionable.5
While elastomeric ligatures are frequently used in orthodontic treatment, they are associated with more bacteria in the plaque than when steel ligatures are used.6 In spite of the introduction of fluoridated elastomers in an effort to overcome these shortcomings, an in vivo study failed to demonstrate the antimicrobial activities of these elastomers.7
A product that releases silver ions from silver-zeolite that is incorporated into an elastomer (Orthoshield Safe T-tie; Ortho Organizers, CA, USA) has been introduced in order to reduce bacterial development around orthodontic appliances. Silver ions have long been used as a broad-spectrum antimicrobial agent in the treatment of wounds and infections.8 Silver ions are also used in dental practice to decrease the activity of cariogenic pathogens, such as S. mutans and other oral streptococci.9,10
Silver-zeolite is a porous crystalline material that is com posed of hydrated sodium aluminosilicate with electrostatically bound Ag+ in its framework.11 This material imparts antibacterial activity to various dental materials through the release of silver ions.12,13 Silver ion-releasing elastomers (silverized elastomer, SE) may help to control the bacterial level in the dental plaque surrounding fixed orthodontic appliances, thereby reducing the risk of iatrogenic demineralization during orthodontic therapy.
As the literature contains little information about the antibacterial effects of SE, we compared the composition of the anaerobic bacteria in the dental plaque that formed on SE to that on a conventional elastomer (CE) in vivo.
The present study was a prospectively performed randomized clinical trial, using a split-mouth crossover design. Forty patients undergoing full fixed orthodontic treatment for at least 3 months were recruited into the study. The patients consisted of 28 females and 12 males with an average age of 21.9 years (standard deviation [SD], 4.2; range, 11.1 - 27.1) (Table 1). We excluded patients who were diabetic; pregnant; used oral antimicrobial agents, such as mouthwash; or took steroids or antibiotics in the 2 months preceding the study. All patients were provided with standardized oral hygiene instructions and Tooth brushing instructions by the same hygienist. In each patient, all molars, anterior teeth, and at least one of the two premolars in every quadrant were bonded. Patients were randomly assigned numbers from 1 to 40 and divided into 1 of 2 groups that differed in the sequence of elastomer application. Ethical approval was obtained from the Institutional Review Board of Korea University Anam Hospital (AnamCTC#2009-192) and written consent was given by all patients or the parents of those patients who were under 18 years of age.
Each patient visited the clinic 4 times with 3 weeks between each visit. During the first visit, patients were scored using the Oral Hygiene Index (OHI-S), which consists of two sub-scales, the Debris Index (DI) and the Calculus Index (CI).14 The subjects of group 1 had SE on the maxillary right central incisor, the maxillary right second premolar (or first premolar if extracted) and mandibular left canine (Figure 1) while the subjects in group 2 had SEs allocated on maxillary left central incisor, maxillary left second premolar (or first premolar) and mandibular right canine. The CEs (Dentalastics, Dentaurum, Isprin gen, Germany) were allocated on teeth contralateral to SEs.
On the second visit, the same practitioner removed the elastomers under aseptic conditions. Each elastomer was placed in a separate carrier bottle containing 1 mL of VMGA III transport medium (Sigma, St. Louis, MO, USA) and sent to the laboratory (Department of Oral Microbiology, School of Dentistry, Kyung Hee University) for microbiological analysis. The practitioner then performed a routine change of wires and tied them with steel ligatures for a washout period.
The third visit consisted of routine orthodontic adjustments and a second application of elastomers. Elastomers were applied to the teeth that were exactly contralateral to those that received elastomers during the first clinic visit.
On the last visit, the elastomers were removed for the second microbiological processes and OHI-S was obtained for the second time.
Each collected elastomer sample was vortexed for 30 seconds and a 6-fold dilution was made by mixing 100 µL of transport medium with VMG I dispersion solution (Sigma) under aseptic conditions. Aliquots were plated onto 3 types of media: Brain-Heart Infusion broth (BD Diagnostic Systems, Sparks, MD, USA) supplemented with 5% sheep blood and 1.5% Micro agar (Duchefa, Haarlem, The Netherlands), Mitis Salivarius Agar (Difco, Sparks, MD, USA), and Mitis Salivarius Agar supplemented with sucrose and bacitracin (Sigma). Plates were incubated for 72 hours at 37℃ under anaerobic conditions (80% N2, 10% H2, 10% CO2) using a Forma Anaerobic System (Thermo Fisher Scientific Inc., Waltham, MA, USA). Cultures were assessed for total anaerobic count (AC), total streptococcal count (SC), and total mutans strep tococci (MS).
The SC was expressed as a percentage of the total AC and MS count was expressed as a percentage of total SC. Mixed-effects analysis of variance was used to examine differences between SE and CE. The independent variables in the model were the fixed factors listed below and the dependent variables were percentage MS and percentage SC. Patients were treated as random variables and the fixed factors included the sequence of elastomer application (group 1 and group 2); visit at which elastomers were collected (second or fourth); the type of elastomer (SE or CE); the type of tooth (central incisor, ca nine, or first or second premolar); bracket type (metal or porcelain); dominant hand for tooth brushing (left or right); gender (male or female); OHI-S (DI and CI); age; and number of days the elastomers were in the mouth. We used OHI-S, age, and days elastomers were in the mouth as covariates in the Spearman's rank correlation analysis we performed to examine the relationships between the dependent variables. SAS® ver 9.1 (SAS, Cary, NC, USA) was used for statistical analysis, and p-values < 0.05 were considered to be statistically significant.
Forty patients were recruited into the study and all of them completed the entire study. Of the 480 elastomers initially applied, 74 were lost between appointments or as a result of microbiologic procedural errors. A total of 198 SEs and 208 CEs were collected. After the first application, elastomers remained in the mouth for an average of 21.8 days (SD, 2.6; range, 16 - 28). After the second application, elastomers remained in the mouth for 21.9 days (SD, 4.8; range, 14 - 41). Colonies recovered from Mitis Salivarius Agar media were confirmed as MS by an accredited public laboratory (Seoul Clinical Laboratories).
The mean bacterial counts of MS, SC, and AC associated with each type of elastomer are shown in Table 2. Mean MS (%) and SC (%) for SE and CE are presented in Table 3. There were no significant differences between SE and CE in the percentage of either MS or SC.
The results of the mixed-effects analysis of variance are shown in Table 4. Elastomers had no significant effect on either MS (p = 0.702) or SC (p = 0.480). Only patient age and number of days elastomers remained in the mouth were significantly associated with SC counts, while MS counts were only significantly associated with gender. No other factors were significantly related to bacterial growth. The Spearman's rank correlation coefficient (rs) we calculated indicated a positive relationship between SC and both patient age and number of days the elastomers remained in the mouth. This means that SC tended to increase as patient age increased or as the duration of elastomer residence in the mouth increased (Table 5).
Silver ions have a strong broad-spectrum bactericidal activity.15 These ions are closely related to a reaction with the thiol groups in vital enzymes or proteins that leads to the inactivation of the proteins. Silver ions also directly interact with DNA, preventing DNA replication.16
Two mechanisms have been proposed for the antimicrobial action of silver-zeolite: silver ions released from the zeolite may act directly against bacterial cells17 or the reactive oxygen species that are generated from the catalytic action of silver ions in the matrix inhibit respiratory enzymes and lead to structural damage in bacteria.18 The latter mechanism is known as oligodynamic action and requires oxygen.9,15 However, silver-zeolite is reported to be effective under anaerobic conditions.19 These two mechanisms have been proposed as successive processes, and regardless of the predominant mechanism, it is evident that silver ions play an important role in the antibacterial action of silver-zeolite.20
In the present study, we investigated the antimicrobial effect of SE on the MS and SC in dental plaque. Considering the antimicrobial activity of silver ions, we hypothesized that the bacterial counts from SE would be lower than those from CE. However, the results showed that there were no significant differences between the percentage of MS or SC in plaque acquired from SEs after a clinically relevant time in the mouth and those in plaque acquired from CEs.
Direct comparisons of these results with those of other studies are difficult because there are no published studies assessing the antimicrobial effect of SE in vivo. Although the exact reason for the lack of antimicrobial effect is unknown, factors such as the time the elastomers were in the mouth, the amount of silver ions released from SE, the physiological condition of the oral cavity, and the physical properties of the elastomer material itself may be important contributors.
Elastomers were in the mouth for an average of 21.9 days. Spearman's rank correlation coefficient indicated that the longer the elastomers are left in the mouth, the higher the SC count is expected to be (rs = 0.230, p < 0.0001). This relationship suggests some explanations for the lack of SE antimicrobial activity in the current study. The release of silver ions from SEs may have been consistent over time, but the concentration of released ions was not sufficient to impede bacterial growth. Alternatively, the concentration of ions released from SEs was initially sufficient to suppress bacterial growth, but the rate of ion release decreased over time in such a way that bacterial populations had recovered by the time samples were collected.
Casemiro et al.21, found that the percentage of silver-zinc-zeolite incorporated into acrylic resins was positively associated with the antimicrobial activity of those resins. This implies that the concentration of silver ions is essential for the antimicrobial action of ion-releasing resins and suggests that the concentration of the silver ion released from SEs in the present study was not sufficient to produce antimicrobial effects.
The constant release of silver ions from silver-zeolite is crucial for maintaining adequate concentrations of these ions for bacterial control over the long term. The authors of a study of the long-term antimicrobial activity of light-activated resin composites10 found that resins with incorporated silver-containing materials (SSAM) inhibit growth of S. mutans in comparison to resin composites that do not contain SSAM. These authors also found that resins with SSAM released little or no silver ions when they were immersed in water for 3 months. They concluded the long-lasting antimicrobial activity of resins with incorporated SSAM may be due to inhibition of S. mutans growth through direct contact with the bacteria, and not by release of silver ions from the composites. The silver-zeolite in SEs contains a limited amount of silver ions that are constantly released into the oral cavity and may become immediately bound to other ions. Thus, reduction or exhaustion of the silver ion supply would occur at some point, decreasing any of antimicrobial activity. In fact, the amount of ion released from temporary filling materials containing silver-zinc-zeolite diminishes over time when these materials are immersed in deionized water.12
As any of antimicrobial activity exhibited by SE is expected to result from silver ions, it is important to understand the rate of ion release from this material. Ahn et al.22 evaluated the amount and pattern of silver ion release into artificial saliva from the same type of SEs that were used in the present study. They found that during the first week, there was a high rate of silver ion release. However, this rate declined over the following 3 weeks.
Given that SEs release silver ions, it is important to determine whether SEs have any antimicrobial effects on S. mutans. Won23 did not find either S. mutans or Porphyromonas gingivalis (P. gingivalis) clear zones around SEs in modified agar disk diffusion tests. SEs were also ineffective in growth inhibition tests when they were in direct contact with S. mutans and P. gingivalis. Won23 speculated that the concentration of the silver ions in the SEs was insufficient for antimicrobial activity.
Berger et al.15 reported that the minimum inhibitory concentration (MIC) of silver ions for various bacterial species was 30 µg/L, while Yoshida et al.10 and Tanagawa et al.24 found that even minute amounts of silver ions that were released from silver-containing resin composites resulted in antimicrobial effects toward S. mutans. Ahn et al.22 calculated that silver ions are released at a rate of only 8.00 - 24.5 µg/L/day from SEs during the first week of immersion in water. The different conditions in each of these studies makes direct comparison among them difficult. Therefore, further silver ion release analysis should be conducted together with MIC tests to verify the lack of antimicrobial activity SEs exhibited in the present study.
Silver ion release from silver-zeolite requires ionic exchange with other cations and is dependent on the concentration of cations in the surrounding solution. In the oral environment, the surrounding solution is saliva.25 This indicates that long-term antimicrobial activity of silver-zeolite can be displayed in solutions with low ionic strength.26 Human saliva contains various inorganic anions as well as cations, and the concentration of cations varies according to systemic balance and condition. This variation in cation concentration affects the release of silver ions into the oral environment.27 Silver and zinc reportedly inhibit bacterial growth.12 The studies showing discordant results with the present study showed ion release in deionized water which would be different from the release behavior of silver ions in saliva. The elastomers in oral cavity would rapidly become coated with salivary proteins and organic-film coating has been cited as one of the main reasons for the clinical failure of silver-coated medical devices.28 The variable physiological environment of the oral cavity may therefore have contributed to the lack of SE antimicrobial effects in the current study.
Unlike steel ligatures, elastomers undergo physical deterioration as they are stretched and come into contact with saliva while they are being placed on orthodontic appliances. Fluoridated elastomers double their weight after 1 month in the mouth.29 One of the reasons suggested for the failure of fluoridated elastomers to produce an antimicrobial effect was that any plaque-inhibiting effect from the fluoride is cancelled by deterioration of the physical properties of the elastomers, leading to a higher bacterial load in fluoridated elastomers.7
For optimal clinical benefit, elastomeric ligatures should be replaced monthly.29 In the present study, the elastomers were in the mouth for 3 weeks; a clinically relevant period. The physical properties of the elastomer after 3 weeks in the mouth had noticeably deteriorated compared to fresh elastomers. This deterioration may contribute to a reduction in the antimicrobial effect of SE.
The quality and the characteristics of the material surface may also play an important part in bacterial adhesion. Ahn et al.30 evaluated the bacterial adhesion tendency and antimicrobial activity of conventional orthodontic bonding and experimental composite adhesives (ECA) that contained nanofillers with varying concentrations of silver nanoparticles. Bacterial growth was slower on ECAs than on conventional adhesives. Th e authors stated that the differences in growth rate are not explained completely by the antimicrobial activity of silver ions or the amount of silver ions contained in ECA and surface characteristics, such as the surface free energy of the materials should also be considered as contributory factors.
Metafasix technology was designed to reduce bacterial adhesion after application of elastomers through a lubricated and polished elastomeric ligature surface. Elastomers applied using this technology, however, harbor more bacteria than conventional elastomers because the fissures created on the polymer coating provide retentive sites for bacterial growth.31 In the present study, the surface characteristics of SEs may have resulted in a net cancellation of any antimicrobial effects. Further examination of SE surfaces should be carried out to better clarify the impact of surface factors on the antimicrobial effects of SEs.
Even though prolonged release of silver ions is possible, and these ions have antimicrobial effects, the SE used in the present study was not effective in reducing bacterial counts below those seen with CE. However, most of the previous studies of the release or antimicrobial effects of silver ions were performed in vitro and the physiological conditions of in vivo studies may differ. Further in vivo studies should be performed to determine the exact amount and duration of silver ion release from SEs, and an analysis of SE surface characteristics should be undertaken to explain why SEs do not display antimicrobial effects. Understanding the reasons for this lack of antimicrobial effect may allow researchers to enhance the antimicrobial activity of SE by adjusting the method and duration of each elastomer application.
There was no significant difference between the percentages of MS and SC in dental plaque obtained from SE and CE after an average of 21.9 days in the mouth (p > 0.05).
There was a positive relationship between the percentage of SC and both the number of days elastomers were present in the mouth and the age of patients (p < 0.05).
Figures and Tables
Figure 1
Diagram showing the application of elastomeric ligatures during the first visit of patients in group 1.

Table 1
Demographic data of patients undergoing orthodontic treatment with silverized and conventional elastomers
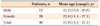
Table 2
Bacterial counts for plaque obtained from conventional and silverized elastomers after 3 weeks in the mouth

Table 3
The rate of bacterial counts for plaque obtained from conventional and silverized elastomers after 3 weeks in the mouth
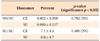
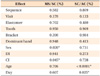
Table 4
Results of the mixed-effects analysis of variance for percentage bacterial counts for plaque obtained from conventional and silverized elastomers after 3 weeks in the mouth
References
1. Scheie AA, Arneberg P, Krogstad O. Effect of orthodontic treatment on prevalence of Streptococcus mutans in plaque and saliva. Scand J Dent Res. 1984. 92:211–217.

2. Rosenbloom RG, Tinanoff N. Salivary Streptococcus mutans levels in patients before, during, and after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991. 100:35–37.

3. Ogaard B. Prevalence of white spot lesions in 19-year-olds: a study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989. 96:423–427.
4. Bowden GH. Effects of fluoride on the microbial ecology of dental plaque. J Dent Res. 1990. 69:653–659.

5. Wiegand A, Buchalla W, Attin T. Review on fluoride-releasing restorative materials--fluoride release and uptake characteristics, antibacterial activity and influence on caries formation. Dent Mater. 2007. 23:343–362.

6. Forsberg CM, Brattström V, Malmberg E, Nord CE. Ligature wires and elastomeric rings: two methods of ligation, and their association with microbial colonization of Streptococcus mutans and lactobacilli. Eur J Orthod. 1991. 13:416–420.

7. Benson PE, Douglas CW, Martin MV. Fluoridated elastomers: effect on the microbiology of plaque. Am J Orthod Dentofacial Orthop. 2004. 126:325–330.

8. Lansdown AB, Sampson B, Laupattarakasem P, Vuttivirojana A. Silver aids healing in the sterile skin wound: experimental studies in the laboratory rat. Br J Dermatol. 1997. 137:728–735.

9. Yamamoto K, Ohashi S, Aono M, Kokubo T, Yamada I, Yamauchi J. Antibacterial activity of silver ions implanted in SiO2 filler on oral streptococci. Dent Mater. 1996. 12:227–229.

10. Yoshida K, Tanagawa M, Matsumoto S, Yamada T, Atsuta M. Antibacterial activity of resin composites with silver-containing materials. Eur J Oral Sci. 1999. 107:290–296.

11. Uchida M. Antimicrobial zeolite and its application. Chem Ind. 1995. 46:48–54.
12. Hotta M, Nakajima H, Yamamoto K, Aono M. Antibacterial temporary filling materials: the effect of adding various ratios of Ag-Zn-Zeolite. J Oral Rehabil. 1998. 25:485–489.

13. Morishita M, Miyagi M, Yamasaki Y, Tsuruda K, Kawahara K, Iwamoto Y. Pilot study on the effect of a mouthrinse containing silver zeolite on plaque formation. J Clin Dent. 1998. 9:94–96.
15. Berger TJ, Spadaro JA, Bierman R, Chapin SE, Becker RO. Antifungal properties of electrically generated metallic ions. Antimicrob Agents Chemother. 1976. 10:856–860.

16. Russell AD, Hugo WB. Antimicrobial activity and action of silver. Prog Med Chem. 1994. 31:351–370.
17. Im K, Takasaki Y, Endo A, Kuriyama M. Antibacterial activity of A-type zeolite supporting silver ions in deionized distilled water. J Antibact Antifung Agents. 1996. 24:269–274.
18. Kourai H, Manabe Y, Yamada Y. Mode of bactericidal action of zirconium phosphate ceramics containing silver ions in the crystal structure. J Antibact Antifung Agents. 1994. 22:595–601.
19. Kawahara K, Tsuruda K, Morishita M, Uchida M. Antibacterial effect of silver-zeolite on oral bacteria under anaerobic conditions. Dent Mater. 2000. 16:452–455.

20. Matsumura Y, Yoshikata K, Kunisaki S, Tsuchido T. Mode of bactericidal action of silver zeolite and its comparison with that of silver nitrate. Appl Environ Microbiol. 2003. 69:4278–4281.

21. Casemiro LA, Gomes Martins CH, Pires-de-Souza Fde C, Panzeri H. Antimicrobial and mechanical properties of acrylic resins with incorporated silver-zinc zeolite - part I. Gerodontology. 2008. 25:187–194.

22. Ahn JS, Hwang EJ, Lee DY, Lim YK. Evaluation of silver ion release from silver-containing elastomers in artificial saliva. J Korea Res Soc Dent Mater. 2010. 37:297–304.
23. Won YA. The antibacterial activities of silver ion releasing elastomers on oral pathogenic microbes [MSc thesis]. 2010. Seoul: Korea University.
24. Tanagawa M, Yoshida K, Matsumoto S, Yamada T, Atsuta M. Inhibitory effect of antibacterial resin composite against Streptococcus mutans. Caries Res. 1999. 33:366–371.

25. Breck DW. Zeolite molecular sieve: structure, chemistry and use. Ion exchange reactions in zeolites. 1973. New York: Wiley.
26. Uchida T, Maru N, Furuhata M, Fujino A, Muramoto S, Ishibashi A, et al. Anti-bacterial zeolite balloon catheter and its potential for urinary tract infection control. Hinyokika Kiyo. 1992. 38:973–978.
27. Shannon IL, Suddick RP, Dowd FJ Jr. Saliva: composition and secretion. Monogr Oral Sci. 1974. 2:1–103.
28. Schierholz JM, Lucas LJ, Rump A, Pulverer G. Efficacy of silver-coated medical devices. J Hosp Infect. 1998. 40:257–262.

29. Wiltshire WA. In vitro and in vivo fluoride release from orthodontic elastomeric ligature ties. Am J Orthod Dentofacial Orthop. 1999. 115:288–292.

30. Ahn SJ, Lee SJ, Kook JK, Lim BS. Experimental antimicrobial orthodontic adhesives using nanofillers and silver nanoparticles. Dent Mater. 2009. 25:206–213.

31. Magno AF, Enoki C, Ito IY, Matsumoto MA, Faria G, Nelson-Filho P. In-vivo evaluation of the contamination of Super Slick elastomeric rings by Streptococcus mutans in orthodontic patients. Am J Orthod Dentofacial Orthop. 2008. 133:4 Suppl. S104–S109.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download