Abstract
Objectives
To determine the prevalence of incidental maxillary sinus findings in a large sample of orthodontic patients by cone-beam computed tomography (CBCT) with a wide field of view and assess the relationships of such abnormalities with age and gender.
Methods
Five hundred thirteen CBCT scans obtained for orthodontic diagnosis and treatment planning in a Northern Italian population (N = 513; 292 female and 221 male subjects; 1,026 maxillary sinuses) were studied. The frequencies of pseudocysts and mucosal thickening of the maxillary sinus were recorded. Logistic regression analysis was used to determine the influence of age and gender on these abnormalities.
The advent of cone-beam computed tomography (CBCT) represents a great improvement in the field of craniofacial imaging.1 Unlike traditional two-dimensional (2D) radiography, CBCT avoids structural superimposition and image enlargement and distortion, thus allowing precise three-dimensional (3D) visualization of dental and maxillofacial structures at a lower radiation dose than multislice computed tomography (CT).1 Such imaging frequently presents the dentist or orthodontist with incidental findings and may raise concerns about the need for further diagnostic tests or referral to other specialists.2,3
Incidental findings are common in the maxillary sinus.4 Although earlier studies using CBCT for dental diagnostic purposes have already addressed this issue,2,4 only one study using CBCT focused on incidental maxillary sinus findings in orthodontic patients.5 However, the study was limited by the small sample size and imaging with a narrow field of view (FOV), which does not allow accurate assessment of sinus pathology.
The aims of this retrospective study were to determine the prevalence of incidental maxillary sinus findings in a large sample of orthodontic patients by CBCT with a wide FOV and assess the relationships of such abnormalities with age and gender.
This study included 680 CBCT images obtained for orthodontic diagnosis and treatment planning at the Department of Orthodontics, University of Ferrara, Italy, between January 2005 and December 2010. The protocol was approved by the local Institutional Review Board.
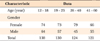
Images of patients with fixed orthodontic appliances, implants, or metallic prosthesis in the maxillary posterior region that could generate scattering phenomena, craniofacial syndromes, or cleft palate were excluded. Finally, 513 CBCT scans of Northern Italian patients (N = 513; 292 female and 221 male subjects; 1,026 maxillary sinuses) were selected. For statistical analysis, the subjects were divided into the following age groups4: 12 - 18, 19 - 25, 26 - 40, and 41 - 60 years. The age and gender distributions are shown in Table 1.
CBCT was performed by using a NewTom 3G volume scanner (QR srl, Verona, Italy) under the following conditions: 12-inch FOV, 110 kV (anterior posterior-latero lateral), 2.00 mA (anterior posterior), 1.00 mA (latero lateral), 5.4-s exposure, and 0.50-mm slice thickness.
The resulting images were elaborated by using NNT NewTom 3G software to obtain the axial sections in which the maxillary sinus could best be distinguished. Then, a line was traced through the greatest mesiodistal dimension of the most suitable sections and various 0.2-mm-spaced coronal sections of the maxilla perpendicular to this line were obtained.
The CBCT scans were reviewed independently by 2 orthodontists trained by a radiologist with experience of over 1,000 NewTom scans at the time of the study. The diagnostic criteria were developed on the basis of the published literature, and in the case of a disagreement, a consensus was reached after a discussion between the observers. Each observer separately performed all the measurements by using the same computer (50-inch liquid crystal display monitors, ASUS VW246H; ASUS, Taipei, Taiwan) and screen resolution (brightness, 300 cd/m2; resolution, 1,920 × 1,080).
Pseudocysts were diagnosed as homogeneous, dome-shaped, noncorticated soft tissue opacities with a smooth and well-defined outline in the maxillary sinus (Figure 1).6,7 For statistical analysis, the pseudocysts were categorized according to their greatest diameter (small, < 1 cm; medium, 1 - 2 cm; large, > 2 cm) and location (right, left, or bilateral).
Mucosal thickening was considered present when the thickness of the sinus mucosa was ≥ 1 mm as measured from the floor of the sinus to the highest border of the mucosa (Figure 2).8 For statistical analysis, this pathology was classified according to the degree of sinus opacification (limited, < 1/3; moderate, 1/3 - 2/3; severe, > 2/3) and location (right, left, or bilateral).
The 2 observers were calibrated for evaluation by together reviewing and discussing the findings of 20 sample CBCT images (10 per pathology) that had been diagnosed as either pseudocysts or mucosal thickening by an experienced radiologist. Each examiner measured and evaluated all the CBCT images twice, on 2 days a week apart. The intra-observer and interobserver agreements were excellent for the linear measurements (intraclass correlation coefficients [ICCs], > 0.92) and very good for the degree of sinus opacification (kappa, > 0.80).
The descriptive statistics are presented as frequencies, and the corresponding 95% confidence intervals (CI) were also calculated. Logistic regression analysis was performed to determine the effects of gender and age on the pathologies. The results are presented in terms of odds ratio increments with respect to a baseline profile, which was set as that pertaining to a 14-year-old female patient. Statistical analyses were performed by using SPSS for Windows software (version 16.0; SPSS Inc., Chicago, IL, USA). The level of significance was set at 0.05.
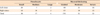
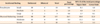
Tables 2 and 3 show the results of the incidental maxillary sinus findings. In total, 258 patients (50.3%) and 317 sinuses (30.9%) had pathologies, with 38.8% and 11.5% of the subjects showing bilateral and unilateral incidental findings, respectively. Pseudocysts were detected in 52 patients (10.1%) and 59 sinuses (5.75%), and 38 of the 59 pseudocysts were small. Further, mucosal thickening was observed in 206 patients (40.1%) and 258 sinuses (25.1%), and 176 of these sinuses presented limited opacification. Either one or both sinuses of 3 (0.6%) and 26 (5.1%) patients showed large pseudocysts and severe opacification, respectively.
Gender was a significant predictor of pseudocysts (p = 0.027), with male subjects showing a 196.3% higher relative risk of this pathology. Age was a significant predictor of mucosal thickening (p < 0.001), with subjects aged 41 - 60 years showing a 401% higher odds ratio than those aged 12 - 18 years.
In this study, 513 CBCT images obtained for orthodontic diagnostic purposes in a Northern Italian population were retrospectively evaluated. Overall, half of the patients had incidental findings in the maxillary sinus. A lower prevalence (19%) in 5,021 Finnish dental patients has been reported by using panoramic radiography,9 which is not as reliable as 3D imaging techniques for diagnosing maxillary sinus pathologies.9,10 The present result is somewhat in accordance with the frequencies (40.0 - 42.5%) reported by using CT and magnetic resonance imaging in the ear-nose-throat field11,12 and is confirmed by the reported prevalence of 56.3% in 1,029 German patients by using CBCT for dental purposes.4
By focusing on CBCT scans for orthodontic purposes, Pazera et al.5 reported a prevalence of 46.8% in 134 Swiss patients (mean age, 17.5 years), but Cha et al.2 reported airway-related findings in only 14.3% of 252 Californian patients (mean age, 18.6 ± 10.1 years). However, direct comparison with the current study is inappropriate because of the different age distribution and geographic origin of the sample. The existing data vary among the studies as a function of different imaging modalities and different age and patient groups. Further, the definitions of pathologic changes vary among the published articles and are sometimes not fully described. In the present work, the diagnostic criteria were predefined and the observers were calibrated to strengthen the reproducibility of the results. Moreover, the ICCs for interobserver and intra-observer reliability were very good, confirming the reliability of the obtained data.
Although pseudocysts, sometimes called mucosal cysts or polypoid mucosal thickening,4,5,8 should be differentiated from mucous retention cysts, which are epithelium-lined true cystic structures usually detected by histologic examination,6,9 many authors use the term "retention cyst" as "pseudocyst."2 Their incidence on panoramic radiographs has been reported to be between 5.8% in an orthodontic population13 and 7.0 - 9.7% in a general dental population.6,9 In the present study, they were diagnosed in 10.1% of the subjects and male patients showed a greater risk, in accordance with previous findings.9,13 The reported incidences on CBCT scans vary between 6.5% and 16.4% in a dental population4,8 and from 3.5% to 19.4% in an orthodontic sample. However, comparisons with the published data should be made cautiously because of the lack of adequate diagnostic criteria.2,4,5
Because the normal thickness of the maxillary sinus mucosa is 0.8 - 1.0 mm,8 we considered a thickness of ≥ 1 mm as evidence of mucosal thickening. The incidence of this pathology on panoramic radiographs has been reported to be between 3% in an orthodontic population and 12% a general dental population.9,10 In the present study, we noted mucosal thickening in 40.1% of the subjects, in accordance with the incidences (38.1% and 42.0%, respectively) reported by Ritter et al.4 and Phothikhun et al.8 among dental patients. This result is higher than the prevalences (23.7% and 7.5%, respectively) reported by Pazera et al.5 and Cha et al.2 in orthodontic patients. Again, the different age and patient groups as well as the different definitions and diagnostic criteria for the pathologic changes may account for these discrepancies. Patients aged 41 - 60 years showed the highest risk of mucosal thickening in the maxillary sinus, supporting previous reports of a higher prevalence of mucosal thickening in older individuals.4,8
So far, no studies have directly and rigorously addressed the prevalence of pseudocysts and mucosal thickening by using CBCT for orthodontic purposes in an Italian population. These sinus abnormalities are benign and self-limiting conditions, generally seen in asymptomatic patients.8 No treatment is required unless they are associated with symptoms or considerable radiographic expansion.8 The high prevalence of incidental maxillary sinus findings in the present study is relevant to orthodontics because of the increasing use of miniscrews as temporary anchorage devices.14,15 As postoperative maxillary sinusitis is one of the most concerning sequelae after sinus perforation,16,17 CBCT evaluation for signs of inflammation in the maxillary sinus before miniscrew placement is very important from both the clinical and the medicolegal points of view. Further research is needed to determine whether these findings can be generalized to a nationally representative sample.
Half of the orthodontic patients showed incidental findings in the maxillary sinus, with 64.4% of the pseudocysts being smaller than 1 cm and 68.2% of the sinuses presenting less than one-third opacification. CBCT scans obtained for orthodontic purposes should be carefully examined in all 3 views (axial, coronal, and sagittal) to exclude any pathologic changes in the maxillary sinus and refer the patient to a specialist if necessary. Detection of signs of inflammation in the maxillary sinus is also relevant when the use of orthodontic miniscrews is planned.
Figures and Tables
References
1. Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E. Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol. 2009. 38:187–195.

2. Cha JY, Mah J, Sinclair P. Incidental findings in the maxillofacial area with 3-dimensional cone-beam imaging. Am J Orthod Dentofacial Orthop. 2007. 132:7–14.

3. Rogers SA, Drage N, Durning P. Incidental findings arising with cone beam computed tomography imaging of the orthodontic patient. Angle Orthod. 2011. 81:350–355.

4. Ritter L, Lutz J, Neugebauer J, Scheer M, Dreiseidler T, Zinser MJ, et al. Prevalence of pathologic findings in the maxillary sinus in cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011. 111:634–640.

5. Pazera P, Bornstein MM, Pazera A, Sendi P, Katsaros C. Incidental maxillary sinus findings in orthodontic patients: a radiographic analysis using cone-beam computed tomography (CBCT). Orthod Craniofac Res. 2011. 14:17–24.

6. Carter LC, Calamel A, Haller A, Aguirre A. Seasonal variation in maxillary antral pseudocysts in a general clinic population. Dentomaxillofac Radiol. 1998. 27:22–24.

7. Carter L, Farman AG, Geist J, Scarfe WC, Angelopoulos C, Nair MK, et al. American Academy of Oral and Maxillofacial Radiology. American Academy of Oral and Maxillofacial Radiology executive opinion statement on performing and interpreting diagnostic cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008. 106:561–562.

8. Phothikhun S, Suphanantachat S, Chuenchompoonut V, Nisapakultorn K. Cone-beam computed tomographic evidence of the association between periodontal bone loss and mucosal thickening of the maxillary sinus. J Periodontol. 2012. 83:557–564.

9. Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. 109:e80–e87.

10. Bondemark L, Jeppsson M, Lindh-Ingildsen L, Rangne K. Incidental findings of pathology and abnormality in pretreatment orthodontic panoramic radiographs. Angle Orthod. 2006. 76:98–102.
11. Gordts F, Clement PA, Buisseret T. Prevalence of sinusitis signs in a non-ENT population. ORL J Otorhinolaryngol Relat Spec. 1996. 58:315–319.

12. Havas TE, Motbey JA, Gullane PJ. Prevalence of incidental abnormalities on computed tomographic scans of the paranasal sinuses. Arch Otolaryngol Head Neck Surg. 1988. 114:856–859.

13. Bósio JA, Tanaka O, Rovigatti E, de Gruner SK. The incidence of maxillary sinus retention cysts in orthodontic patients. World J Orthod. 2009. 10:e7–e8.
14. Kravitz ND, Kusnoto B. Risks and complications of orthodontic miniscrews. Am J Orthod Dentofacial Orthop. 2007. 131:4 Suppl. S43–S51.

15. Papadopoulos MA, Papageorgiou SN, Zogakis IP. Clinical effectiveness of orthodontic miniscrew implants: a meta-analysis. J Dent Res. 2011. 90:969–976.

16. Gracco A, Tracey S, Baciliero U. Miniscrew insertion and the maxillary sinus: an endoscopic evaluation. J Clin Orthod. 2010. 44:439–443.
17. Graham JW, Cope JB. Cope JB, editor. Potential complications with OrthoTADs: classification, prevention, and treatment. OrthoTADs: The clinical guide and atlas. 2007. Dallas: Under Dog Media LP;119–134.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download