Abstract
In the correction of dental Class III molar relationship in skeletal Class II patients, uprighting of the mandibular posterior segments without opening the mandible is an important treatment objective. In the case reported herein, a C-tube miniplate fixed to the lower labial symphysis and connected with a nickel-titanium reverse-curved archwire provided effective uprighting of the lower molars, without the need of orthodontic appliances on the mandibular anteriors. Using this approach, an appropriate magnitude of force is exerted on the molars while avoiding any negative effect on the mandibular anteriors.
Moderate dental Class III malocclusion is commonly associated with a high mandibular plane, anterior open bite, and mesially tipped molars.1-3 The molars may be over-erupted, whereas the mandibular anteriors may be under-erupted. Ideally, the treatment goals would include uprighting the molars without propping open the mandible and increasing facial height. If the incisors are well related in the smile, the treatment goal would be to maintain that relationship. Various treatment modalities have been suggested to achieve these goals, for example, the multiloop edgewise archwire (MEAW) or upper accentuated-curve and lower reverse-curve nickel-titanium (NiTi) archwires combined with intermaxillary elastics.4,5 These methods typically result in some extrusion of the anterior teeth. Class III elastics cause extrusion of the maxillary molars and mandibular anterior teeth, which is inappropriate for patients who are skeletally hyperdivergent or have excessive lower incisor display.
Temporary skeletal anchorage devices (TSADs) have been recommended for the provision of anchorage for uprighting and intrusion of the posterior teeth.6-8 This approach can provide some closure of the mandibular angle and reduction of facial height, without the need of surgical intervention.6,9 However, mini-implant placement between the first and second molar area has a few technical and anatomical limitations. Sufficient interradicular space is crucial for both safety and stability of the mini-implant.10,11 Park and Cho12 reported that the interradicular space at a vertical distance of 7 mm from the cement-enamel junction was less than 2 mm on the maxillary first and second molar area, which would provide less than 1 mm of clearance around the mini-implant. To obtain sufficient clearance, the mini-implant might need to be placed further apically; however, that would lead to placement of the implant head in mucous tissue and subsequently result in inflammation.13 Maxillary sinus invasion and the short height of the mandibular body also limit posterior TSAD placement.
If uprighting of the posterior teeth were possible without the use of intermaxillary elastics or posterior TSADs, the side effects and technical difficulties associated with the correction of dental Class III malocclusion would be minimized. In this report, we introduce a new method of achieving these goals by applying control from the anterior region. The proposed system allows a more dependable and simple placement of a TSAD, and the biomechanics are targeted to the mandibular buccal segments without any application of force on the lower anteriors (Figure 1).
A 12-year-old girl had a chief complaint of posterior open bite (Figure 2, Table 1). She had received previous orthodontic treatment to resolve dental protrusion 2 years earlier at a local clinic. The maxillary and mandibular second molars were removed, with the goal of distalizing the entire dentition and correcting mandibular deficiency, using a twin block-type removable appliance with a posterior bite block (Figure 2F). However, the treatment resulted in an iatrogenic posterior open bite and mesial tipping of the lower molars after 2 years. She presented at our clinic with a full-cusp Class III molar relationship, posterior open bite, deep mandibular curve of Spee, accentuated curve in the maxillary arch, spacing of the maxillary dentition, and mesially tipped lower molars with no centric relation-centric occlusion (CR-CO) discrepancy. Lip protrusion was obvious in the lateral profile, and facial asymmetry was insignificant. A panoramic radiograph showed the formation of the third molars on both sides (Figure 3A). Cephalometric analysis revealed a skeletal Class I relationship (ANB 3.1°) and normodivergent vertical pattern (FMA 26.5°). The maxillary incisors were proclined excessively (U1 to FH 127.8°), and the mandibular incisors showed normal inclination (IMPA 95.0°) (Figure 3B, Table 1). Residual growth was not significant because the cervical vertebrae maturation indicator (CVMI) stage was 5 and menarche had occurred 2 years ago.
Based on these findings, the patient was diagnosed with skeletal Class I, dental Class III with posterior open bite. Although she had lip protrusion, she refused additional extraction of upper premolars due to the increase in treatment duration and previous experience of 4 second-molars extraction. Therefore, a nonextraction approach for dental correction was selected. The treatment objectives were (1) to upright the mandibular molars without concomitant extrusion, (2) to resolve the posterior open bite, and (3) to achieve a functional Class I occlusion with ideal overbite and overjet.
Based on the above objectives, two treatment options were proposed. First, to upright the mandibular molars, intermaxillary mechanics using MEAW with Class III elastics were proposed. Second, the use of orthodontic mini-implants on the mandibular buccal sides by intraarch mechanics was proposed. However, the main goal of treatment was to upright the lower molars without causing any vertical changes to the mandibular incisors; therefore, a C-tube miniplate fixed to the lower labial symphysis connected with a NiTi reverse-curved archwire was applied first. During uprighting of the lower molars, a spontaneous eruption of the maxillary molars to the mesial direction was anticipated.
The I-type C-tube miniplate (Jin-Biomed Co., Bucheon, Korea) was placed in the symphysis area. Because the device was quite small, and the fixation screws were short, the surgical procedure for C-tube placement was easier than that for conventional miniplates. A 5-mm vertical incision without flap elevation was performed for placement (Figure 4A). After adaptation of the miniplate to the bone contour, it was fixed with two 1.5 × 5-mm self-drilling miniscrews (Figure 4B and 4C). The insertion procedure has been described in a previous article.14 The tube portion exited the tissue near the cervical margin of the lower incisors. Soft tissue irritation did not pose a problem, because it penetrated the attached gingiva, and the position could be adjusted such that it was accommodated in the neutral space between the gingiva and lower lip. The C-tube served to support the archwire, which was to be raised to a brass wire (0.8 mm) extension held by the head part of the tube (Figure 4D-4F). The length of the brass wire extension could be modified to apply the desired magnitude of force on the posterior teeth.
Posterior bonding was limited to the severely tipped mandibular first and second premolars and first molars. The force system was applied from the C-tube and brass wire connector via a 017 × 025-in reverse-curve NiTi archwire. After 3 months, molar uprighting, Class I molar relationship, and bite closure occurred (Figure 5). In addition, the incisors moved in to provide excellent interdigitation with no application of force (Figure 6). The maxillary arch was bonded at 4 months to accomplish space closure. During the last 4 months before debonding, a full-fixed appliance was applied to the mandibular anterior teeth for further finishing and detailing. To maintain the uprighted angulation of lower first molars and second premolars, a segmented archwire was used on the anterior teeth.
The total duration of treatment was 18 months (Figure 7). The molar and canine relationships were corrected from the full-step Class III to the Class I relationship. Posterior open bite was corrected by controlling the inclination of the upper and lower molars, and ideal overbite and overjet were achieved. Serial lateral cephalograms showed the uprighting of the mandibular posterior teeth and flattening of the upper occlusal plane (Figure 8). Serial panoramic radiographs confirmed the uprighting of the mandibular premolars and first molars, and favorable root parallelism. Mesial drifting of the mandibular third molars and a good eruption path of upper third molars followed (Figure 9). Figure 8E and Table 1 show the post-treatment cephalometric findings. Horizontal and vertical skeletal relationship was well maintained. Inclination of the anterior teeth on both arches was not changed. Superimposition of pre- and post-treatment cephalograms revealed that the posterior open bite was corrected mainly with extrusion of the maxillary molars while the mandibular first molars uprighted and intruded slightly. The lower incisors were bodily retracted. One year after debonding, treatment results were stable and satisfactory (Figure 10). In the panoramic radiograph, 4 third molars were well erupted into the second molar space. Superimposition of the post-treatment and one year retention radiographs showed minimal dental movement (Figure 11, Table 1).
Conventionally, the MEAW technique, which involves the use of multiloop gable-bend archwires and vertical elastics in the canine regions, has been an efficient tool for molar uprighting.4 The goals of this technique include reducing the inclination of the occlusal plane, alignment of the maxillary incisors relative to the lip line, and uprighting the axial inclinations of the posterior teeth. The MEAW treatment minimally changes the skeletal pattern in adults.15 Kim16 reported that during MEAW therapy, the maxillary molars are intruded by an average of 0.66 mm, the mandibular molars do not show any significant eruption, and the maxillary incisors are extruded by 0.7 mm. Patients who have an ideal incisor display should not be treated by the extrusive mechanics associated with MEAW.
Enacar et al.5 modified the MEAW technique by using 0.016 × 0.022-in upper accentuated-curve and lower reverse-curve NiTi archwires, instead of the multiloop archwires, and applying intermaxillary elastics in the canine regions. They suggested that the upper accentuated-curve and lower reverse-curve NiTi archwires were simpler and more hygienic to use compared to the multiloop archwires, and that they reduced chair time and did not irritate the soft tissues. The effects of this treatment method were similar to those of the MEAW system in that the inclination of the occlusal plane was corrected, the open bite was corrected by extrusion of the mandibular incisors, uprighting of the maxillary incisors was achieved, and axial inclinations of the posterior teeth were uprighted. Although the configuration of the archwires in the molar region induced tip back and intrusion to the molars, no actual molar intrusion took place. Instead, the molars were extruded while being uprighted.
Our design is similar to MEAW or its modification by Enacar et al.5 However, it can be differentiated based on its 5 unique advantages. First, only limited bonding is required on the posterior teeth. Moreover, forces are targeted to the molar area, without undesired movement of the anterior teeth, if the incisors are in a good position before treatment. Molar uprighting is possible with good restraint of molar extrusion, which is unavoidable with other techniques. In reported cases without the use of TSADs, the maxillary molars generally had a slight extrusion15,17,18 or intrusion (within 1 mm),4 and the mandibular molars were always slightly extruded.4,15,17,18 In our case, the posterior open bite accommodated the extrusion of the maxillary molars, similar to the mechanics of MEAW or Class III elastics. However, in typical skeletal Class II and dental Class III cases without posterior open bite, our mechanics would provide better results by preventing extrusion of maxillary molars that might aggravate skeletal Class II relationship. The amount of intrusive and uprighting force applied to the molars can be adjusted by modifying the length of brass wire connector. Second, indirect anchorage or figure-8-lacing of the premolars provides a supporting fulcrum to maximize the intrusive force on the molar region. Third, the anterior region is favored for TSADs placement over the posterior area1 - access is good, and there are fewer limitations to placement. Fourth, an appropriately installed miniplate causes less soft tissue irritation than does a miniscrew, and it can endure more dynamic orthodontic forces than a miniscrew can; therefore, it is stable even when a long range of action is need. Fifth, Class III elastics are not necessary; therefore, there are fewer negative side effects and less stress on the temporomandibular joint.
In our design, both extrusive and intrusive uprighting are possible depending on the choice of teeth that are bonded in the posterior segment, the magnitude of activation force, and the distance between the ascending ramus and the distal surface of last molar. The molars positioned more distally will receive more intrusive and uprighting force. If the first molar needs intrusion, the clinician should include an attachment on the first premolar, which will produce more intrusion on the molar. If the second molar has no attachment, it will spontaneously tip back and extrude in response to the uprighting of the first molar. An interesting feature of this protocol is the spontaneous retraction of mandibular incisors. The available space achieved by uprighting of the posterior teeth is followed by controlled lingual tipping of the mandibular incisors as a result of lip pressure and the tension of the periodontal fibers between the teeth. Since the buccal intrusive force vectors are not in line with the center of resistance, some buccal expansion may occur. The clinician can control this with archwire adjustments such as constriction of intermolar width and lingual crown torque. Considering that the nonlinear behavior of the periodontal ligament, the morphology of the root, and the alveolar bone are patient specific, the center of rotation could be different between patients, although the same biomechanics are applied. With these potential variations in mind, the force system selected for a specific tooth movement and the outcome must be monitored.
A new biomechanical system is described for the correction of certain types of dental Class III malocclusions, with the goal of distalizing and uprighting mandibular molars without extrusion. The system includes the placement of attachments only on teeth that are targeted for movement, with anchorage supplied by a lower anterior miniplate attached to the labial bone of the symphysis. The forces applied with the reverse-curve NiTi archwire proved very effective for molar uprighting and, if desired, posterior bite closing.
Figures and Tables
Figure 1
Schematic illustration of the molar uprighting protocol. Components include a C-tube plate on the symphysis, bonded target posterior teeth, and a reverse-curve NiTi archwire. A, B, Before activation. The reverse-curve NiTi archwire is engaged to the mesially inclined posterior teeth and rests apical to the head I-type C-tube miniplate. C, D, For activation, the midline of the wire is lifted by attaching it to a brass connector from the C-tube. The dotted pink line illustrates the path of force application of the archwire.

Figure 2
Pre-treatment intraoral photographs. A - E, Posterior open bite resulted from a previous treatment with a twin block-type removable appliance with a posterior bite block (F).

Figure 4
Surgical placement of the C-tube miniplate on the facial surface of the symphysis and engagement of the archwire. A, A 5-mm vertical incision along the midline (flap unnecessary). B, Adaptation of the miniplate. C, Fixation of the C-tube plate using 2 self-drilling miniscrews (diameter 1.5 mm, length 5 mm) and 1 or 2 sutures. D, E, The brass wire (diameter 0.8 mm) connects the tube hole to the 017 × 025-in reverse-curve NiTi archwire. F, Resin capping on the hook of the brass wire to prevent soft tissue irritation.

Figure 5
Treatment progress. A-C, Immediately after bonding; D-F, after 3 months; G-I, and after 4 months; J-L, molar uprighting achieved a Class I molar relationship and spontaneous bite closure.

Figure 6
Detailed changes in the incisors. A, Pre-treatment; B, after 1 month; C, after 4 months; D, after 7 months.

Figure 8
Serial lateral cephalograms A-D, and overall superimposition E, initial (solid line) and post-treatment (dotted line). A, Pre-treatment; B, after 1 month; C, after 4 months. D, Debonding at 18 months; mandibular posterior teeth uprighted, and occlusal plane flatter.

Figure 9
Serial panoramic radiographs. A, Pre-treatment; B, after 1 month; C, after 4 months. D, Debonding at 18 months; mandibular molars were uprighted, and roots parallelism was achieved. Third molar position was improved.

Figure 11
One year retention. A, Lateral cephalogram; B, panoramic radiograph; and C, overall superimposition (post-treatment [solid line] and one year retention [dotted line]).

Table 1
Pre-treatment, post-treatment, and 1-year retention cephalometric results
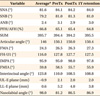
PreTx, Pre-treatment; PostTx, post-treatment.
*For Korean Data from Korean Association of Orthodontists.19
References
1. Kim YS, Cha JY, Yu HS, Hwang CJ. Comparison of mandibular anterior alveolar bone thickness in different facial skeletal types. Korean J Orthod. 2010. 40:314–324.

2. Miyajima K, Iizuka T. Treatment mechanics in Class III open bite malocclusion with Tip Edge technique. Am J Orthod Dentofacial Orthop. 1996. 110:1–7.

3. Lee BR, Kang DK, Son WS, Park SB, Kim SS, Kim YI, et al. The relationship between condyle position, morphology and chin deviation in skeletal Class III patients with facial asymmetry using cone-beam CT. Korean J Orthod. 2011. 41:87–97.

4. Kim YH, Han UK, Lim DD, Serraon ML. Stability of anterior openbite correction with multiloop edgewise archwire therapy: A cephalometric follow-up study. Am J Orthod Dentofacial Orthop. 2000. 118:43–54.

5. Enacar A, Ugur T, Toroglu S. A method for correction of open bite. J Clin Orthod. 1996. 30:43–48.
6. Park YC, Lee HA, Choi NC, Kim DH. Open bite correction by intrusion of posterior teeth with miniscrews. Angle Orthod. 2008. 78:699–710.

7. Moon CH, Lee JS, Lee HS, Choi JH. Non-surgical treatment and retention of open bite in adult patients with orthodontic mini-implants. Korean J Orthod. 2009. 39:402–419.

8. Kim MJ, Park SH, Kim HS, Mo SS, Sung SJ, Jang GW, et al. Effects of orthodontic mini-implant position in the dragon helix appliance on tooth displacement and stress distribution: a three-dimensional finite element analysis. Korean J Orthod. 2011. 41:191–199.

9. Deguchi T, Kurosaka H, Oikawa H, Kuroda S, Takahashi I, Yamashiro T, et al. Comparison of orthodontic treatment outcomes in adults with skeletal open bite between conventional edgewise treatment and implant-anchored orthodontics. Am J Orthod Dentofacial Orthop. 2011. 139:4 Suppl. S60–S68.

10. Kuroda S, Yamada K, Deguchi T, Hashimoto T, Kyung HM, Takano-Yamamoto T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2007. 131:4 Suppl. S68–S73.

11. Asscherickx K, Vande Vannet B, Wehrbein H, Sabzevar MM. Success rate of miniscrews relative to their position to adjacent roots. Eur J Orthod. 2008. 30:330–335.

12. Park J, Cho HJ. Three-dimensional evaluation of interradicular spaces and cortical bone thickness for the placement and initial stability of microimplants in adults. Am J Orthod Dentofacial Orthop. 2009. 136:314.e1–314.e12.

13. Kim SH, Yoon HG, Choi YS, Hwang EH, Kook YA, Nelson G. Evaluation of interdental space of the maxillary posterior area for orthodontic mini-implants with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009. 135:635–641.

14. Chung KR, Kim SH, Kang YG, Nelson G. Orthodontic miniplate with tube as an efficient tool for borderline cases. Am J Orthod Dentofacial Orthop. 2011. 139:551–562.

15. Chang YI, Moon SC. Cephalometric evaluation of the anterior open bite treatment. Am J Orthod Dentofacial Orthop. 1999. 115:29–38.

16. Kim YH. Anterior openbite and its treatment with multiloop edgewise archwire. Angle Orthod. 1987. 57:290–321.
17. Küçükkeleş N, Acar A, Demirkaya AA, Evrenol B, Enacar A. Cephalometric evaluation of open bite treatment with NiTi arch wires and anterior elastics. Am J Orthod Dentofacial Orthop. 1999. 116:555–562.

18. Janson G, Valarelli FP, Beltrão RT, de Freitas MR, Henriques JF. Stability of anterior open-bite extraction and nonextraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2006. 129:768–774.

19. Korean Association of Orthodontists. Cephalometric norm of Korean adults with normal occlusion. 1998. Seoul: Ji-Sung Publishing Co.;589–595.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download