Abstract
Objective
To evaluate the antimicrobial effect of different frequencies of brushing with fluoride toothpaste on the levels of salivary mutans streptococci and lactobacilli in children undergoing fixed orthodontic treatment.
Methods
The study included 22 patients scheduled for fixed orthodontic therapy distributed between 2 groups with different hygiene regimes. All the subjects received identical braces, bands, and brackets bonded with the same material. Stimulated saliva samples were obtained before placement of the appliance and at 6, 12, and 18 weeks during the therapy. Saliva samples were cultured on selective microbial agar for the detection of microorganisms.
Results
Salivary mutans streptococci were significantly suppressed throughout the experimental period in the group that brushed 4 times a day as compared to the group that brushed twice a day. Salivary lactobacilli were not significantly affected by the frequency of brushing with 0.32% sodium fluoride (NaF) toothpaste.
Fixed orthodontic appliances hinder cleaning of teeth and favor the retention of dental plaque. Placement of fixed orthodontic appliances results in a change in the intraoral environment, leading to increased bacterial density in dental plaque.1,2 Streptococcus mutans (S. mutans) has been identified as a major cariogenic microorganism in dental plaque.3 Further, Lactobacillus species (spp.) that are encountered in different stages of caries progression are considered secondary invaders of existing carious lesions and encourage caries progression.4 The number of S. mutans can increase by up to 5 fold during orthodontic treatment.2 High numbers of colony-forming units of Lactobacillus spp. have been associated with use of orthodontic appliances and known to play a role in the increased levels of plaque seen in many orthodontic patients.5 In addition to oral hygiene instructions, professional mechanical tooth cleaning and toothbrushing instructions for new orthodontic patients, numerous researchers have investigated the use of antimicrobial agents in orthodontic patients. Some findings suggest that while orthodontic treatment results in increased levels of salivary S. mutans in some individuals, the use of antimicrobials such as chlorhexidine may not have warranted efficacy in all orthodontic patients.6 Aciduric intraoral microflora within dental plaque in orthodontic patients may be managed by dietary counseling, oral hygiene instructions, and judicious administration of fluoride modalities.7 Clinical studies evaluating the effectiveness of fluoride programs in orthodontic patients have shown conflicting results.8,9 During orthodontic treatment, fluoride can be applied to the teeth using various vehicles, including topical (fluoridated toothpaste, mouth rinse, gel, and varnish) and adhesive (fluoride-releasing cements and elastomeric modules and chains) agents. The chosen method for caries prevention largely depends on the individual requirements of each patient and the clinician's judgement.
Fluoride inhibits caries formation by acting on the de- and remineralization processes in dental hard tissues as well as the physiology of microbial cells, including S. mutans, which can indirectly affect tooth demineralization.10 Fluoride exerts antimicrobial activity by directly inhibiting cellular enzymes (direct binding of F- or hydrogen fluoride, or in combination with metals) or by enhancing proton permeability of cell membranes in the form of hydrogen fluoride (acting as a transmembrane proton carrier).11,12 Hydrogen fluoride enters the bacterial cell membrane and dissociates to yield hydrogen and F-. Intracellular F- inhibits glycolytic enzymes resulting in decreased acid production from glycolysis. Additionally, it lowers cytoplasmatic pH, affecting the acid production and acid tolerance of mutans streptococci.11 The complex anticaries mechanism of fluoride depends on the fluoride concentration and pH of the applied fluoride preparation.13
Fluoride-containing toothpaste, as the main antimicrobial caries-preventive measure for orthodontic patients, is often underestimated because its regular application and frequent toothbrushing depends on patient compliance.
The aim of this study was to determine the changes in the salivary levels of mutans streptococci and lactobacilli in patients with fixed orthodontic appliances in relation to the frequency of toothbrushing with standard fluoride toothpaste.
Patients scheduled for fixed orthodontic therapy at the dental clinic of the Department of Orthodontics, Clinical Hospital Zagreb, were invited to participate in this study. All experimental procedures were conducted in accordance with the recommendations of the Declaration of Helsinki for physicians in biomedical research involving human subjects. The study was approved by the Ethics Committee of School of Dental Medicine, University of Zagreb. All the participants and their parents/guardians received written information about the aims and design of this study and were asked to sign written informed consent forms.
The following inclusion criteria were applied in this study: permanent dentition period, i.e., from 12 to 17 years of age; moderate crowding; good general health; completion of general dental care; and consent to participate. The exclusion criteria were as follows: receiving systemic or prolonged prescribed medication or antibiotic therapy and bracket failure during the experimental period. All the subjects were required to establish good oral hygiene status before the beginning of the study and were counseled regarding oral hygiene maintenance and toothbrushing before the treatment and at each visit. None of the subjects used supplementary fluoride, antimicrobial varnish, or mouthwash during the study. A total of 22 subjects met the inclusion criteria and were enrolled in the study. The orthodontic process at each stage was consistent for all subjects.
All subjects received equal braces consisting of 4 bands and 20 brackets from the same manufacturer (Forestadent, Pforzheim, Germany) bonded with the same adhesive material (Transbond XT Light; 3M Unitek, Monrovia, CA, USA) without fluoride. A halogen light source was applied for 20 seconds per each bracket for polymerization. Wire ligatures were used throughout the treatment. All the subjects used commercial toothpaste containing 0.32% sodium fluoride (NaF). The average weight of 1 cm of the toothpaste used was 1.2 g, which contained 3.8 mg of NaF (0.32% × 1.2 g = 0.0038 g).
For microbial analysis of the saliva a Cultura incubator (Ivoclar Vivadent, Schaan, Liechtenstein) and a CRT bacteria testing kit with mitis-salivarius with bacitracin agar, Rogosa agar, NaHCO3 tablets, pipettes, and vials (Ivoclar Vivadent) were used. To analyze the pH of the saliva a hand-held digital pH meter (Piccolo plus ATC pH-meter, Hannah Instruments, Woonsocket, RI, USA), sterile plastic graduated cups, and 0.1 M acetic acid were used.
The subjects voluntarily chose one of 2 different hygiene regimes, on the basis of which they were divided into 2 groups. The first group of subjects (group A) was instructed to brush their teeth twice a day (morning and evening) during the entire experimental period. The second group (group B) was instructed to brush their teeth twice a day (morning and evening) during the weeks before the start of orthodontic therapy, but following placement of the fixed appliances, they were instructed to brush their teeth after every meal (4 times a day: after breakfast, snack, lunch, and dinner). Of the 22 children who participated in this study, 9 agreed to regularly brush their teeth twice a day (morning and evening), while the remaining 13 chose to regularly brush their teeth after every meal throughout the experimental period.
All subjects were counseled regarding oral hygiene maintenance and toothbrushing techniques before the treatment and at every visit (all instructions were done by the same experienced investigator). At each visit, subjects were informed about the differences in their microbial test results from that visit as compared to their previous visit. In case the scores had worsened, the patients were counseled again regarding toothbrushing and encouraged to improve their oral hygiene. In case their scores had improved, the children were complimented. All the subjects used toothpaste containing 0.32% NaF, and all the subjects were instructed to apply 1 cm of toothpaste and brush for 3 minutes at each brushing. Since the average weight of 1 cm of this toothpaste was 1.2 g, it contained 3.8 mg of NaF (0.32% × 1.2 g = 0.0038 g). Thus, group A effectively used approximately 7.5 mg of NaF/day (2 × 0.0038 g) and group B used approximately 15 mg of NaF/day (4 × 0.0038 g).
Saliva samples were collected 2 weeks before the fixed appliance treatment was initiated, and this was considered to be the baseline assessment. Thereafter, samples were obtained at 6, 12, and 18 weeks after the placement of fixed orthodontic appliances.
Samples were collected in the morning between 9 and 12 a.m. under standardized conditions. The subjects were instructed not to eat or drink for at least 1 hour prior to sample collection and to brush their teeth only once in the morning on the day of sample collection. Subjects sat on a dental chair, bent slightly forward, chewed bilaterally on a standardized piece of paraffin wax, and collected the stimulated saliva by spitting for 10 minutes into a sterile plastic cup with 1-mL gradation marks. The volume of the collected saliva was measured in mL, and the salivary flow rate was calculated based on the collection time of 10 minutes (mL/minute).14 The first salivary pH was measured using a handheld digital pH meter with automatic temperature compensation.14 Collected saliva (2 mL) was treated with 0.1 mL of 0.1 M acetic acid, and the pH was measured again.14 The downward pH change was calculated by subtracting the pH of the treated saliva from that of the untreated saliva,14 and the salivary buffer capacity was calculated according to buffer capacity defined as Cbuffer = -Δn(acid)/(V1•ΔpH), where -Δn(acid) is the amount of acid added, V1 is the volume of saliva, and ΔpH is the pH change induced by the addition of acid.
For determination of mutans streptococci levels in the saliva, mitis-salivarius with bacitracin agar was used according to the manufacturer's instructions. Immediately after sample collection, 1 mL of saliva was inoculated on the agar, enclosed in the test vial containing a NaHCO3 tablet, and placed in an incubator at 37℃ (99°F) for 48 hours. The mutans streptococci count per mL of saliva was estimated by comparing the colony density on the growth substrate with the evaluation chart provided by the manufacturer (0, no colonies detected; 1, < 105 colony-forming units (CFU)/mL; 2, ≥ 105 CFU/mL). The same procedure was used to enumerate lactobacilli in the saliva, but selective Rogosa agar, obtained from the same manufacturer, was used instead.
Descriptive statistics and the χ2 test were used to determine age and gender differences, respectively. Friedman analysis of variance (ANOVA) was used to test the overall level of significance from the data for each group of subjects. The non-parametric Wilcoxon matched-pairs test, following the significant results of Friedman ANOVA, was used to determine the significance of changes in individual time points for salivary flow rate, pH, and buffer capacity before and after insertion of the orthodontic appliances, over a period of 18 weeks for both groups. The Mann-Whitney U-test was used to compare the salivary flow rate, pH, buffer capacity, and scores of the microbial tests between the 2 groups at each measurement time.
A generalized linear model was used to analyze scores of the microbial tests for mutans streptococci and lactobacilli between the two groups, and the χ2 test was used for analysis of independent data at each measurement time.
A probability of null hypothesis < 0.05 was considered statistically significant. For statistical analysis, Statistica software (version 8; StatSoft Inc., Tulsa, OK, USA) was used.
A total of 22 subjects met the inclusion criteria for participation in this study. There were 9 boys and 13 girls with a mean age of 14.04 ± 1.56 years (range, 12 - 17 years). The salivary flow rate, pH, buffer capacity, and salivary levels of mutans streptococci and lactobacilli before placement of the fixed orthodontic appliances and at 6, 12, and 18 weeks after the placement were analyzed for gender and age subgroups of the subjects using the χ2 and Spearman rank order correlation tests, respectively. There were no significant differences in these parameters for gender or age.
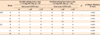
Table 1 presents the salivary flow rate, pH, and buffer capacity of both the groups. The levels of mutans streptococci and lactobacilli in the saliva before and during the 18 weeks of orthodontic therapy are presented in Table 2. The overall level of significance for salivary mutans streptococci and lactobacilli data was analyzed with a generalized linear model (for mutans streptococci, p = 0.019; for lactobacilli, p > 0.05). The χ2 test for salivary mutans streptococci in mL of saliva before and 18 weeks after the placement of orthodontic appliances revealed significant differences between the 2 groups at week 6 (χ2 = 6.14, degree of freedom [d.f.] = 1, p = 0.013) and week 12 (χ2 = 4.20, d.f. = 1, p = 0.04). The χ2 test for lactobacilli per mL of saliva before and 18 weeks after insertion of orthodontic appliances revealed no significant differences between the 2 groups.
The Mann-Whitney U-test revealed that the frequency of brushing with 0.32% NaF toothpaste significantly affected the counts of salivary mutans streptococci between the 2 groups for each time point (Table 2). Salivary mutans streptococci were significantly lower at 6 and 12 weeks in group B than in group A. In group A, the number of CFUs of mutans streptococci in the saliva significantly increased during the experimental period. The Mann-Whitney U-test showed that the brushing frequency had no significant effect on the levels of lactobacilli in the saliva (Table 2). Salivary lactobacilli were not significantly affected by frequency of use of 0.32% NaF-containing toothpaste. In both groups, the number of CFUs of salivary lactobacilli significantly increased throughout the experimental period.
This study provides important information on the effect of the frequency of toothbrushing with fluoride toothpaste on oral health of orthodontic patients undergoing fixed appliance therapy. Despite dietary counseling and the use of antimicrobial agents, fluoridation measures are currently the most promising approach to improve oral hygiene. The results of a 3 years oral hygiene program, including fluoride products, in patients treated with fixed orthodontic appliances showed that caries increments were the highest and gingival health were the poorest in the group using standardized fluoride-free toothpaste.15 Dénes and Gábris16 showed that solely brushing or mechanical cleaning of teeth with fluoride-free toothpaste for orthodontic patients is far less efficient in caries prevention than brushing with fluoride-containing toothpaste. Based on results of that study, we decided not to include fluoride-free toothpaste as a control in our study; instead, we preferred to focus on the differences in the usage frequency of standard fluoride-containing toothpaste. The use of toothpaste and gel with a high fluoride concentration of 1,500 - 5,000 ppm during orthodontic treatment clearly showed a demineralization-inhibiting tendency.9 Although this is beneficial for orthodontic patients, toothpaste or gel with such high fluoride concentrations are not common for daily use; therefore, we focused our study on toothpastes containing 1,450 ppm fluoride (0.32% NaF), which is the common fluoride concentration found in toothpastes for daily use. Toothpastes containing at least 1,000 ppm fluoride can effectively prevent tooth decay in children.15
Similar to the results of some other investigations, our study showed significant increase in the levels of cariogenic mutans streptococci and lactobacilli in saliva soon after commencing fixed orthodontic therapy.14,17 This is due to obstruction of proper tooth cleaning and increased retention of dental plaque around the fixed orthodontic appliances. In agreement with our results, the authors of other studies have reported that orthodontic appliances alter the microbiology of dental plaque and result in an increase in the levels of mutans streptococci, leading to dental enamel decalcification.2,18-20 It has been reported that orthodontic appliances do not considerably alter the levels of mutans streptococci in patients if proper controls are used.21 Few approaches can be adopted for decreasing the levels of mutans streptococci in the saliva during orthodontic treatment. Various studies in high-risk orthodontic patients did not find significant differences in caries increment after repeated application of high- or low-concentration chlorhexidine varnishes.22,23 Other studies on orthodontic patients have documented a reducing effect of chlorhexidine and/or fluorides on caries increment and S. mutans.24,25 The results of our study also confirm the findings of a reducing effect of fluoride on mutans streptococci. In our study we observed that fluorides from the commonly available, widely used fluoride-containing toothpaste causes a decrease in the levels of mutans streptococci in the saliva of orthodontic patients if regularly applied after every meal. In a recent review of the literature regarding topical fluorides, Marinho et al.26 revealed that fluoride toothpastes have a similar degree of effectiveness as mouth rinses or gels in the prevention of dental caries in children. The authors concluded that there is no clear suggestion that fluoride varnish is more effective than mouth rinses and gels, but acceptance among children is likely to be greater for fluoride toothpaste. Our results show that frequent use of fluoride toothpaste by orthodontic patients helped in maintaining lower levels of mutans streptococci in the saliva; therefore, our results are in agreement with those of Alexander and Ripa19 who reported that control of the S. mutans level and adequate oral hygiene in orthodontic treatment is an important and achievable goal. Our results show another interesting observation: the salivary mutans streptococci levels did not differ between the 2 groups (brushing twice a day or 4 times a day) at week 18. Additionally, there was a significant decrease in the salivary pH and a significant increase in the salivary buffer capacity in both groups between weeks 12 and 18. Considering that none of our orthodontic patients received supplementary fluoride, professional cleaning, or other antimicrobial preventive measures, it may be concluded that the decrease in the levels of mutans streptococci in the saliva at week 18 of orthodontic therapy was caused by the intraoral characteristics of patient. Mutans streptococci were successfully inhibited by changes in the salivary pH and buffer capacity which was a physiological response to disturbed intraoral homeostasis. The clinical significance of the decreased levels of mutans streptococci in the saliva at week 18 of orthodontic therapy is yet to be determined. Our results are in accordance with those of the study by Lara-Carrillo et al.27 who found that the frequency of brushing with fluoridated toothpaste was correlated to salivary mutans streptococci at 1 month after placement of appliances but not in the later stages of orthodontic therapy. A sizeable body of evidence from randomized controlled trials firmly establishes the benefits of topical fluorides, although the significance of its delivery modes to orthodontic patients is still unclear.28 A recent study showed that the third application of toothpaste in a day results in increasing F retention in saliva and plaque.29 The reduced levels of salivary mutans streptococci in our orthodontic patients who brushed with fluoride toothpaste 4 times a day may have also resulted from a similar mechanism.
In our study, brushing with fluoride toothpaste did not have any antibacterial effect on Lactobacillus spp. This result is in accordance with similar studies in which long-term use of fluoride mouth rinses have been known to affect the detectable levels of mutans streptococci but not lactobacilli.30 Although it has been shown that the degree of growth inhibition of oral lactobacilli by flouride can vary, its effect may depend on the type of strain, F concentrations,31 as well as environmental pH.32
The clinical significance of the decreased salivary levels of mutans streptococci but not lactobacilli after brushing with fluoride toothpaste for more than three times a day in orthodontic patient is yet to be determined. As Derks et al.9 called for future clinical trials to provide evidence-based advice on the optimal caries-prevention strategy for orthodontic patients, we suggest, on the basis of our results, that the success of antimicrobial preventive measures in orthodontic patients may be significantly improved by strongly encouraging patients to brush their teeth with 0.32% NaF (1,450 ppm fluoride-containing) toothpaste after every meal during their orthodontic therapy. Interdisciplinary work between the cariologist and orthodontist should be promoted further to develop caries prevention strategies for orthodontic patients, who are at a high caries risk.
The difference in daily application frequency of 0.32% NaF-containing toothpaste (4 times vs. 2 times) resulted in a difference in the level of salivary mutans streptococci in children with fixed orthodontic appliances. Therefore, these results demonstrated that higher frequency of fluoride toothpaste application results in lower counts of mutans streptococci in the saliva. Further, we found that the salivary lactobacillus levels in children with fixed orthodontic appliances were not affected by NaF toothpaste.
Figures and Tables
Table 1
Summary of salivary flow rate, pH, and buffer capacity of saliva before (week 0, baseline) and at 6, 12, and 18 weeks after insertion of orthodontic appliances (n = 22)

NaF, sodium fluoride; SD, standard deviation.
*Wilcoxon matched-pairs test was used (following Friedman's ANOVA yielded a significant result) at a significance level of p < 0.05; †When baseline (0) value is compared with the 6, 12, and 18 week data points; ‡When data point of each week is compared with the data point of the preceding week.
References
1. Huser MC, Baehni PC, Lang R. Effects of orthodontic bands on microbiologic and clinical parameters. Am J Orthod Dentofacial Orthop. 1990. 97:213–218.

2. Rosenbloom RG, Tinanoff N. Salivary Streptococcus mutans levels in patients before, during, and after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991. 100:35–37.

4. Kneist S, Schmidt F, Callaway A, Willershausen B, Rupf S, Wicht M, et al. Diversity of Lactobacillus species in deep carious lesions of primary molars. Eur Arch Paediatr Dent. 2010. 11:181–186.

5. Kupietzky A, Majumdar AK, Shey Z, Binder R, Matheson PB. Colony forming unit levels of salivary Lactobacilli and Streptococcus mutans in orthodontic patients. J Clin Pediatr Dent. 2005. 30:51–53.

6. Attin R, Ilse A, Werner C, Wiegand A, Attin T. Antimicrobial effectiveness of a highly concentrated chlorhexidine varnish treatment in teenagers with fixed orthodontic appliances. Angle Orthod. 2006. 76:1022–1027.

7. Section on Pediatric Dentistry and Oral Health. Preventive oral health intervention for pediatricians. Pediatrics. 2008. 122:1387–1394.
8. Benson PE, Parkin N, Millett DT, Dyer FE, Vine S, Shah A. Fluorides for the prevention of white spots on teeth during fixed brace treatment. Cochrane Database Syst Rev. 2004. (3):CD003809.

9. Derks A, Katsaros C, Frencken JE, van't Hof MA, Kuijpers-Jagtman AM. Caries-inhibiting effect of preventive measures during orthodontic treatment with fixed appliances. A systematic review. Caries Res. 2004. 38:413–420.

10. Buzalaf MA, Pessan JP, Honório HM, ten Cate JM. Mechanisms of action of fluoride for caries control. Monogr Oral Sci. 2011. 22:97–114.

11. Koo H. Strategies to enhance the biological effects of fluoride on dental biofilms. Adv Dent Res. 2008. 20:17–21.

12. Marquis RE, Clock SA, Mota-meira M. Fluoride and organic weak acids as modulators of microbial physiology. FEMS Microbiol Rev. 2003. 26:493–510.

13. Rosin-Grget K, Sutej I, Lincir I. The effect of saliva on the formation of KOH-soluble fluoride after topical application of amine fluoride solutions of varying fluoride concentration and pH. Caries Res. 2007. 41:235–238.

14. Chang HS, Walsh LJ, Freer TJ. The effect of orthodontic treatment on salivary flow, pH, buffer capacity, and levels of mutans streptococci and lactobacilli. Aust Orthod J. 1999. 15:229–234.
15. Walsh T, Worthington HV, Glenny AM, Appelbe P, Marinho VC, Shi X. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2010. (1):CD007868.

16. Dénes J, Gábris K. Results of a 3-year oral hygiene programme, including amine fluoride products, in patients treated with fixed orthodontic appliances. Eur J Orthod. 1991. 13:129–133.

17. Kanaya T, Kaneko N, Amaike C, Fukushima M, Morita S, Miyazaki H, et al. The effect of orthodontic appliances on levels of Streptococcus mutans, Streptococcus sobrinus and microbial flora in saliva. Int Congr Ser. 2005. 1284:189–190.

18. Boersma JG, van der Veen MH, Lagerweij MD, Bokhout B, Prahl-Andersen B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors. Caries Res. 2005. 39:41–47.

19. Alexander SA, Ripa LW. Effects of self-applied topical fluoride preparations in orthodontic patients. Angle Orthod. 2000. 70:424–430.
20. Vierrou AM, Manwell MA, Zamek RL, Sachdeva RC, Tinanoff N. Control of Streptococcus mutans with topical fluoride in patients undergoing orthodontic treatment. J Am Dent Assoc. 1986. 113:644–646.

21. Dikeman TL. A study of acidogenic and aciduric microorganisms in orthodontic and non-orthodontic patients. Am J Orthod. 1962. 48:627–628.

22. Jenatschke F, Elsenberger E, Welte HD, Schlagenhauf U. Influence of repeated chlorhexidine varnish applications on mutans streptococci counts and caries increment in patients treated with fixed orthodontic appliances. J Orofac Orthop. 2001. 62:36–45.

23. Lundström F, Krasse B. Caries incidence in orthodontic patients with high levels of Streptococcus mutans. Eur J Orthod. 1987. 9:117–121.

24. Madléna M, Vitalyos G, Márton S, Nagy G. Effect of chlorhexidine varnish on bacterial levels in plaque and saliva during orthodontic treatment. J Clin Dent. 2000. 11:42–46.
25. Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ. Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J Orthod Dentofacial Orthop. 1992. 101:403–407.

26. Marinho VC, Higgins JP, Sheiham A, Logan S. One topical fluoride (toothpastes, or mouthrinses, or gels, or varnishes) versus another for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2004. (1):CD002780.

27. Lara-Carrillo E, Montiel-Bastida NM, Sánchez-Pérez L, Alanís-Tavira J. Changes in the oral environment during four stages of orthodontic treatment. Korean J Orthod. 2010. 40:95–105.

28. Marinho VC. Cochrane reviews of randomized trials of fluoride therapies for preventing dental caries. Eur Arch Paediatr Dent. 2009. 10:183–191.

29. Nordström A, Birkhed D. Effect of a third application of toothpastes (1450 and 5000 ppm F), including a 'massage' method on fluoride retention and pH drop in plaque. Acta Odontol Scand. 2012. [Epub ahead of print].

30. Kaneko N, Yoshihara A, Ida H, Nomura Y, Imai S, Nisizawa T, et al. Influence of a fluoride mouthrinse on mutans streptococci in schoolchildren. Caries Res. 2006. 40:501–507.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download