Abstract
Objective
The purpose of this study was to evaluate the validity of the 3-dimensional (3D) superimposition method of digital models in patients who received treatment with rapid maxillary expansion (RME) and maxillary protraction headgear.
Methods
The material consisted of pre- and post-treatment maxillary dental casts and lateral cephalograms of 30 patients, who underwent RME and maxillary protraction headgear treatment. Digital models were superimposed using the palate as a reference area. The movement of the maxillary central incisor and the first molar was measured on superimposed cephalograms and 3D digital models. To determine whether any difference existed between the 2 measuring techniques, intra-class correlation (ICC) and Bland-Altman plots were analyzed.
Results
The measurements on the 3D digital models and cephalograms showed a very high correlation in the antero-posterior direction (ICC, 0.956 for central incisor and 0.941 for first molar) and a moderate correlation in the vertical direction (ICC, 0.748 for central incisor and 0.717 for first molar).
The evaluation of orthodontic tooth movement is an important step in the orthodontic treatment process. The superimposition of serial cephalograms has been widely used to measure orthodontic tooth movement.1,2 However, cephalometric superimpositions have several limitations, including tracing errors, radiation exposure, and difficulties in evaluating tooth movements 3-dimensionally.3
Many studies have evaluated orthodontic tooth movement by means of pre- and post-treatment dental casts.4-7 With the development of 3-dimensional (3D) technologies, the use of 3D digital models of dental casts have been investigated for diagnosis and treatment planning.8-11 Also, tooth movements can now be assessed using 3D superimposition of dental casts.12-16 The 3D superimposition of digital models requires a stable reference area. Several studies examined the applicability of the palatal rugae as a reference area for 3D superimposition.7,15,17-19 However, no consensus seems to have been reached on the stability of the palatal rugae in conjunction with growth20,21 or orthodontic treatment.4 In a previous study, we evaluated the possibility of using the palate as reference area for superimposition of 3D digital models based on surface-to-surface matching technology and demonstrated that this method is clinically reliable in extraction cases.12
Maxillary protraction headgear with rapid maxillary expansion (RME) has been used in the treatment of Class III growing patients. This treatment modality can not only cause the forward movement of the maxilla and the maxillary dentition, but also change the shape of the palate.22-24 The superimposition method using the palate as reference area has not been examined in growing patients who have undergone orthopedic treatment, such as RME and protraction headgear treatment. The purpose of this study was to evaluate the validity of the 3D superimposition method using the palate as a reference area in cases of RME and maxillary protraction headgear treatment.
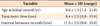
The material consisted of pre- and post-treatment maxillary dental casts and lateral cephalometric radiographs of 30 patients (12 males and 18 females, mean age 9.6 years) who underwent RME and maxillary protraction headgear treatment at Gangneung-Wonju National University Dental Hospital from 1998 to 2007. Inclusion criteria were (1) fully erupted maxillary central incisors and first molars, (2) no inflammatory swelling on the palate, and (3) successful treatment with RME appliances and maxillary protraction headgear. Details of patient ages and treatment periods are summarized in Table 1.
The pre- and post-treatment cephalometric radiographs were manually traced on conventional translucent acetate paper. All bilateral structures were bisected. The coordinate system of Cha et al.12 was used to evaluate tooth movement. On the pre-treatment tracing, the coordinate system was established with the occlusal plane as the X-axis and a line perpendicular to the occlusal plane through the sella as the Y-axis. This coordinate system was subsequently transferred to the post-treatment tracing (Figure 1). The superimposition of cephalograms was performed on the palatal plane with anterior nasal spine (ANS) as the registration point. The antero-posterior and vertical movement of the tip of the central incisors and the mesial cusp tip of the first molars was measured. The radiographic magnification was adjusted to 100%.
The 3D scanning of the maxillary dental casts was performed with a non-contact 3D optical scanner (Orapix, Orapix Co., Seoul, Korea; reliability, ±20 µm). The reconstruction and superimposition of the 3D digital models were performed using 3D reverse modeling software (Rapidform 2002, INUS Technology Inc., Seoul, Korea). On the pre-treatment digital model, the coordinate system was established with the junction of the incisive papilla and palatine raphe as the origin (0, 0, 0), resulting in the X-, Y-, Z-axes and 3 planes (Figure 2). To measure tooth movement, pre- and post-treatment, 3D models were superimposed using the palate as a reference area, which included the palatal rugae and palatal slope separated by 5 mm from the gingival margins of the bilateral posterior teeth, and did not extend distally beyond the line in contact with the distal surfaces of the bilateral first molars (Figure 3). The measuring points were the midpoint on the edge of the upper central incisor and the mesio-buccal cusp tip of the upper first molar (Figure 2). The anteroposterior and vertical movement of the central incisors and the first molars were measured.
To reduce the error in identifying the measuring points, all measurements were performed twice by the same investigator at an interval of 2 weeks, and the average values of the measurements were used. The intra-examiner correlation coefficients of cephalometric variables were greater than 0.934, and those of 3D variables were greater than 0.996.
The antero-posterior and vertical tooth movements measured on cephalometric radiographs were compared with those determined using the superimposed 3D models. Bland-Altman plots using 95% limits of agreement (average differences ± 1.96 of the standard deviation of the differences) and intra-class correlation (ICC) were generated to determine whether a significant difference existed between the 2 measuring techniques. Data were processed with SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA).
The ICC values between 3D variables and cephalometric variables are listed in Table 2. ICC was the highest (0.956) for the antero-posterior movement of the incisors and the lowest (0.717) for the vertical movement of the first molars. ICC values for the antero-posterior movement of the first molars and the vertical movement of the incisors were 0.941 and 0.748, respectively.
Figure 4 shows Bland-Altman plots of difference against means for tooth movements as determined cephalometrically and by 3D model superimposition. The Bland-Altman 95% limits of agreement for antero-posterior movement of the central incisors were -1.3 mm to 0.8 mm, with a range of ±1.1 mm from the mean difference of -0.2 mm (Figure 4A), and those for vertical movement of the central incisors were -1.5 mm to 3.1 mm, with a range of ±2.3 mm from the mean difference of 0.8 mm (Figure 4B). In the first molars, the Bland-Altman 95% limits of agreement between cephalograms and 3D models were -1.3 mm to 1.1 mm, with a mean difference of -0.1 mm antero-posteriorly, and -1.3 mm to 2.1 mm with a mean difference of 0.4 mm vertically (Figure 4C and 4D).
The importance of establishing stable reference structures for measuring the changes in tooth movement during treatment or growth cannot be overemphasized. Many studies have reported the stability of the palatal rugae as reference points for pre- and post-treatment dental comparisons on model casts.4,5,7,18,24 Schwarze24 advocated the use of the posterior medial rugae points in evaluating antero-posterior changes of the buccal teeth. van der Linden18 reported that the lateral ends of the first rugae were stable. Almeida et al.5 suggested that the transverse offsets and distances between the medial rugae points were generally stable, particularly for the first rugae. In studies measuring antero-posterior molar movement, Hoggan and Sadowsky7 and Jang et al.15 reported that the median end of the third palatal rugae could be used as a reliable landmark.
Recently, we also reported that the palate can be used as a reference area to assess tooth movement in adult extraction cases.12 However, the 3D superimposition method of palatal registration, which is a type of best-fit method,12 has not been confirmed as a reliable method in cases of growth and orthopedic treatment. In cases of RME treatment, palatal depth is known to be reduced as a result of inferior displacement of the palatal shelves.25-28 Therefore, it is not surprising that the regional registration technique has not yet been confirmed as an accurate method in cases which a significant change of the palatal shape occurs during growth and/or orthopedic treatment.
In the present study, despite the changes in the palate after RME and maxillary protraction treatment, the antero-posterior incisor and molar movements measured using 3D superimposed models demonstrated very high correlations (0.956 for the incisors and 0.941 for the molars) with those measured in cephalometric radiographs (Table 2). Additionally, the Bland-Altman 95% limits of agreement between cephalograms and 3D models had a range of ±1.1 mm for the incisors and ±1.2 mm for the first molars (Figure 4A and 4C). These results suggest that the 3D maxillary superimposition method is as clinically reliable for assessing antero-posterior tooth movement in RME protraction headgear cases as in cephalometric superimposition. However, the vertical movement of the upper central incisor and the first molar demonstrated only moderate correlations (Table 2), and in the Bland-Altman plot, the 95% limits of agreement exceeded 2.0 mm (Figure 4B and 4D). These findings are not in accordance with those from our earlier study, which did not find any differences in the vertical variables either.12
The difficulty in differentiating buccal cusps from palatal cusps bilaterally in cephalograms may be one of the reasons for the differences in the vertical measurements between the 2 methods. RME treatment causes extrusion of the palatal cusps as a result of buccal flaring of the maxillary molars27,29 and wedge-shaped opening of the maxillae.26,28,30 Accordingly, future studies will need to consider the possibility of error in the vertical measurements, possibly through the use of landmarks that are temporarily attached to the buccal and palatal cusps of the molars and are recognizable both on the scanned models and cephalograms.
Changes in palatal shape may be another source of error in the 3D superimposition method. Palatal depth was reported to decrease after RME treatment,25,28 despite the increase in arch width. As shown in Figure 3C and 3D, the inclination of the palatal slope was changed. Therefore, the best-fit superimposition in the present study should be carried out at the bottom of the palate to avoid lateral shifting of the pre-and post-treatment models when they are superimposed. This phenomenon may explain our observation that the vertical movements measured on 3D model superimposition were less extrusive than those measured on cephalometric superimposition.
The very high correlation between the 3D superimposition technique used in this study and the superimposition of cephalograms does not mean they are very precise, but neither is superior over the other. For the evaluation of long-term treatment results in growing patients, the best-fit method used in the present study may lead to different results. However, in the absence of stable structures-such as implants-this method is currently the best option.
Although the measurements on the 3D digital models and cephalograms were only moderately correlated in the vertical direction and opinions differ with respect to the problem of 3D superimposition on the mandible, this method is still valid with regards to clinical interpretations.
Figures and Tables
 | Figure 1The coordinate system and cephalometric superimposition of the maxilla along the palatal plane registered at anterior nasal spine (ANS). The X-axis was defined as the line through the maxillary central incisor tip and the mesio-buccal cusp tip of the first molar on the initial cephalogram, and the Y-axis as a line perpendicular to X-axis through the Sella. PNS, posterior nasal spine. |
 | Figure 2The coordinate system. A, The X-Z horizontal plane includes the origin, which is the junction of the incisive papilla and palatine raphe and is parallel to the occlusal plane constructed by bilateral mesio-buccal cusp tips of the first molars and the midpoint of the central incisors. B, The X-Y sagittal plane, which is perpendicular to the horizontal plane, is made up of the origin point and one arbitrary point on the mid-palatal suture. C, The Y-Z frontal plane is the section inclusive of the origin and perpendicular to both the sagittal and the horizontal planes. The measuring points were the midpoint on the edge of the upper central incisors and the mesio-buccal cusp tips of the upper first molars. |
 | Figure 3
A, Superimposed models with differences displayed in colors on a millimeter scale. B, Superimposition of pre-treatment model (red) and post-treatment model (blue). Coronal view sectioned at C, the second premolars and D, the first molars. |
 | Figure 4Bland-Altman plots portraying the agreement between cephalometric and 3-dimensional (3D) measurements for A, antero-posterior tooth movement of central incisors; B, vertical tooth movement of central incisors; C, anteroposterior tooth movement of first molars; and D, vertical tooth movement of first molars. Each circle represents the difference between the measurements determined by the 2 methods (Y-axis) relative to the average of tooth movement measured by the 2 methods (X-axis). The thick lines indicate the mean, and the thin lines show the 95% limits of agreement. |
Notes
References
1. Ricketts RM. A four-step method to distinguish orthodontic changes from natural growth. J Clin Orthod. 1975. 9:208–215. 218–228.
2. Pancherz H. A cephalometric analysis of skeletal and dental changes contributing to Class II correction in activator treatment. Am J Orthod. 1984. 85:125–134.

3. Ghafari J, Baumrind S, Efstratiadis SS. Misinterpreting growth and treatment outcome from serial cephalographs. Clin Orthod Res. 1998. 1:102–106.

4. Peavy DC Jr, Kendrick GS. The effects of tooth movement on the palatine rugae. J Prosthet Dent. 1967. 18:536–542.

5. Almeida MA, Phillips C, Kula K, Tulloch C. Stability of the palatal rugae as landmarks for analysis of dental casts. Angle Orthod. 1995. 65:43–48.
6. Bailey LT, Esmailnejad A, Almeida MA. Stability of the palatal rugae as landmarks for analysis of dental casts in extraction and nonextraction cases. Angle Orthod. 1996. 66:73–78.
7. Hoggan BR, Sadowsky C. The use of palatal rugae for the assessment of anteroposterior tooth movements. Am J Orthod Dentofacial Orthop. 2001. 119:482–488.

8. Motohashi N, Kuroda T. A 3D computer-aided design system applied to diagnosis and treatment planning in orthodontics and orthognathic surgery. Eur J Orthod. 1999. 21:263–274.

9. Cha BK, Choi JI, Jost-Brinkmann PG, Jeong YM. Applications of three-dimensionally scanned models in orthodontics. Int J Comput Dent. 2007. 10:41–52.
10. Lim MY, Lim SH. Comparison of model analysis measurements among plaster model, laser scan digital model, and cone beam CT image. Korean J Orthod. 2009. 39:6–17.

11. Lee SK, Kwon OW, Sung JH. A study on the dental arch characteristics of bialveolar protrusion patients using a three-dimensional digital model. Korean J Orthod. 2006. 36:45–54.
12. Cha BK, Lee JY, Jost-Brinkmann PG, Yoshida N. Analysis of tooth movement in extraction cases using three-dimensional reverse engineering technology. Eur J Orthod. 2007. 29:325–331.

13. Commer P, Bourauel C, Maier K, Jager A. Construction and testing of a computer-based intraoral laser scanner for determining tooth positions. Med Eng Phys. 2000. 22:625–635.

14. Hayashi K, Araki Y, Uechi J, Ohno H, Mizoguchi I. A novel method for the three-dimensional (3-D) analysis of orthodontic tooth movement-calculation of rotation about and translation along the finite helical axis. J Biomech. 2002. 35:45–51.

15. Jang I, Tanaka M, Koga Y, Iijima S, Yozgatian JH, Cha BK, et al. A novel method for the assessment of three-dimensional tooth movement during orthodontic treatment. Angle Orthod. 2009. 79:447–453.

16. Miller RJ, Kuo E, Choi W. Validation of Align Technology's Treat III digital model superimposition tool and its case application. Orthod Craniofac Res. 2003. 6:Suppl 1. 143–149.

17. Ashmore JL, Kurland BF, King GJ, Wheeler TT, Ghafari J, Ramsay DS. A 3-dimensional analysis of molar movement during headgear treatment. Am J Orthod Dentofacial Orthop. 2002. 121:18–29.

18. van der Linden FP. Changes in the position of posterior teeth in relation to ruga points. Am J Orthod. 1978. 74:142–161.

19. Cha BK, Lee JY, Bae SH, Park DI. Preliminary study of future orthodontic model analysis: the orthodontic application of 3-dimensional reverse engineering technologies. J Korean Dent Assoc. 2002. 40:107–117.
20. Friel S. Migration of teeth. Dent Rec (London). 1949. 69:74–84.
21. Simmons JD, Moore RN, Erickson LC. A longitudinal study of anteroposterior growth changes in the palatine rugae. J Dent Res. 1987. 66:1512–1515.

22. Geran RG, McNamara JA Jr, Baccetti T, Franchi L, Shapiro LM. A prospective long-term study on the effects of rapid maxillary expansion in the early mixed dentition. Am J Orthod Dentofacial Orthop. 2006. 129:631–640.

23. Phatouros A, Goonewardene MS. Morphologic changes of the palate after rapid maxillary expansion: a 3-dimensional computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2008. 134:117–124.

24. Schwarze CW. Does removal of the tooth germs of the third molars have an influence on the late form of the dental arch? Fortschr Kieferorthop. 1973. 34:387–400.
25. Spillane LM, McNamara JA Jr. Maxillary adaptation to expansion in the mixed dentition. Semin Orthod. 1995. 1:176–187.

26. Jafari A, Shetty KS, Kumar M. Study of stress distribution and displacement of various craniofacial structures following application of transverse orthopedic forces: a three-dimensional FEM study. Angle Orthod. 2003. 73:12–20.
27. Matsumoto M, Yoshii O. A case report of the rapid expansion of the maxillary dental arch by opening the mid palatal suture. Nihon Kyosei Shika Gakkai Zasshi. 1968. 27:166–174.
28. Timms DJ. Rapid maxillary expansion. 1981. Chicago: Quintessence.
29. Wertz R, Dreskin M. Midpalatal suture opening: a normative study. Am J Orthod. 1977. 71:367–381.

30. Biederman W. Rapid correction of Class 3 malocclusion by midpalatal expansion. Am J Orthod. 1973. 63:47–55.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download