Abstract
Objective
To evaluate the presurgical orthodontic tooth movement of mandibular teeth after dental decompensation for skeletal Class III deformities on the basis of vertical skeletal patterns.
Methods
This cohort was comprised of 62 patients who received presurgical orthodontic treatment. These patients were divided into 3 groups according to their vertical skeletal patterns. Changes in the positions of the mandibular central incisor, canine, premolar, and 1st molar after presurgical orthodontic treatment were measured using a cone-beam computed tomography (CBCT) superimposition method.
Results
The incisors moved forward after dental decompensation in all 3 groups. The canines in group I and the 1st premolars in groups I and III also moved forward. The incisors and canines were extruded in groups I and II. The 1st and 2nd premolars were also extruded in all groups. Vertical changes in the 1st premolars differed significantly between the groups. We also observed lateral movement of the canines in group III and of the 1st premolar, 2nd premolar, and 1st molar in all 3 groups (p < 0.05).
Dental compensation manifests to varying degrees in the majority of patients undergoing orthognathic surgery. In patients with skeletal Class III deformities, the natural compensatory mechanism compels the maxillary dentition to flare buccolabially, while lingual tipping of the incisors and posterior segments is generally observed in the mandibular dentition. Johnston et al.1 reported that if incisor decompensation during presurgical orthodontic treatment is inadequate, the surgical outcome can be unsatisfactory. Capelozza Filho et al.2 similarly reported a correlation between the extent of incisor decompensation, lower anterior facial height, mandibular setback surgery, and postoperative mandibular excess. Therefore, the extent of incisor decompensation obtained during presurgical orthodontic treatment dictates the magnitude of surgical change and is a major factor in determining the success or failure of treatment outcomes. Thus, achievement of dental decompensation during presurgical orthodontic treatment is indispensible to maximizing surgical correction and ensuring dental stability.3
However, achieving adequate decompensation is sometimes difficult, due to neuromuscular function, bite force, periodontal health, and mandibular symphyseal thickness among other factors. In patients with strong masticatory muscles, it is difficult to achieve extrusion of the buccal segments during leveling of the curve of Spee. Even if the curve of Spee is left preoperatively, the space between the premolar teeth can easily be corrected postoperatively by extruding these teeth, as there are no occlusal contacts to oppose the tooth movement.4
For cases with a narrow symphysis, Wehrbein et al.5 have suggested that pronounced sagittal incisor movement and de-rotation are critical risk factors critical to progressive lingual and labial bone loss. In addition, Chung et al.6 found that the width of the symphyseal region and the alveolar height were significantly lower in patients with open bite than in those with a negative overjet. There are limitations to tooth movement within the alveolar bone. Moreover, the range of tooth movement can differ depending on vertical facial skeletal patterns.
Dentoalveolar compensation has been described relative to a variety of factors, including anteroposterior and vertical facial skeletal patterns. Therefore, clinicians need to understand the phenomenon of post-decompensation tooth movement in order to accurately predict orthognathic surgery outcomes. In this regard, Ahn and Baek7 investigated dental decompensation in skeletal Class III patients using lateral cephalograms, but treated only the incisor position. Nam et al.8 studied the incisor and 1st molar positions using both lateral cephalograms and cast models. However, with the exception of the incisors, it was very difficult to assess post-decompensation tooth movement using lateral cephalograms. Furthermore, accurate superimposition of their cast models was very difficult.8 Overall, there have been few successful orthognathic surgery studies measuring post-decompensation tooth movement in skeletal Class III patients.
The purpose of the present study was to evaluate, on the basis of vertical skeletal patterns, the presurgical orthodontic tooth movement of the incisors, canines, premolars, and 1st molars after dental decompensation in patients with skeletal Class III malocclusions. For the cases of skeletal Class III malocclusion examined, the null hypothesis was that there were no significant differences in presurgical orthodontic tooth movements after dental decompensation.
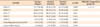
The cohort employed in this retrospective study comprised of 62 patients who had been diagnosed with skeletal Class III malocclusions and received presurgical orthodontic treatment at Pusan National University Hospital. These subjects were divided into 3 groups according to their vertical skeletal patterns (Table 1): group I comprised 22 patients (age, 25.9 ± 5.8 years) with a hyperdivergent skeletal pattern (Frankfort mandibularplane angle [FMA] > 32°); group II, 20 patients (age, 24.3 ± 2.9 years) with a normodivergent skeletal pattern (22° < FMA ≤ 32°); and group III, 20 patients (age, 25.2 ± 6.1 years) with a hypodivergent skeletal pattern (FMA ≤ 21°). The exclusion criteria were as follows: metal restorations (crown, amalgam restoration), severe facial asymmetry (>3 mm difference in chin deviation), missing teeth, greater than 4 mm crowding/spacing, and cleft lip and/or palate. Roth prescription 0.022-inch straight-wire ceramic appliances were fully bonded. This study was reviewed and approved by the Institutional Review Board of Pusan National University Hospital (E-2011068).
Images were obtained using a cone-beam computed tomography (CBCT) scanner (Pax-Zenith 3D; Vatech Co., Gyeonggi-Do, Korea) both before orthodontic treatment (T0) and surgery (T1). At the T1 stage, final archwires were 0.019 × 0.025" stainless-steel wires. The subjects were seated upright for maximum intercuspation and reposed lip without archwires. The scanner settings were as follows: field of view, 20 × 19 cm; tube voltage, 90 kVp; tube current, 4.0 mA; scan time, 24 seconds; isotropic voxel size, 0.30 mm. The CBCT raw data were reformatted to three-dimensional (3D) images using 3D imaging software (Ondemand 3D; Cybermed Inc., Seoul, Korea).
In order to analyze post-decompensation tooth movement, CBCT data images of the symphyseal area and the lower part of the mandible below the root apex taken before orthodontic treatment (T0) and before surgery (T1) were superimposed according to maximization of the mutual information theory (Figure 1).9,10
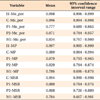
The reference points and planes were defined as indicated in Table 2. The following variables were used to evaluate tooth movement (Tables 2 and 3; Figure 1): anteroposterior changes of each tooth, I1-Me_per, C-Me_per, P1-Me_per, P2-Me_per, M1-Me_per; vertical changes of each tooth, I1-MP, C-MP, P1-MP, P2-MP, M1-MP; and transverse changes of each tooth, I1-MSR, C-MSR, P1-MSR, P2-MSR, M1-MSR.
All variables were obtained from the right side, and 3D cephalometric measurements were performed by 2 investigators, both of whom had been trained in the use of the software and in the identification of pertinent landmarks. The differences between values for each variable obtained at T0 and T1 stages were calculated.
The data were analyzed using a statistical software package program (SPSS ver. 12.0; SPSS Inc., Chicago, IL, USA). All variables were reassessed at 2-week intervals by the same investigator. The intraclass correlation coefficient (ICC) was the measure of the intra-investigator and interinvestigator errors determining reproducibility. A paired t-test was conducted to evaluate tooth movement changes after presurgical orthodontic treatment. To determine the differences in changes in tooth movement according to vertical skeletal patterns, an analysis of variance (ANOVA) with Scheffe's multiple comparison test was used (p < 0.05).
The average ICC was 0.887 (95% confidence interval [CI], lower = 0.803, upper = 0.999). The ICC of P1-Me_per was the lowest, and that of I1-Me_per was the highest (Table 4). There were no significant differences in the anteroposterior skeletal pattern, IMPA, or crowding between groups at stage T0 (p > 0.05, Table 1).
The incisors moved forward after dental decompensation in groups I, II, and III (I1-Me_per) (p < 0.05). The canines also moved forward in group I (C-Me_per), along with the 1st premolars in groups I and III (P1-Me_per). However, there were no significant differences in the extent of anteroposterior change between groups I, II, and III (p > 0.05; Table 5, Figure 2).
The incisors and canines were extruded after presurgical orthodontics in groups I and II (I1-MP). The 1st and 2nd premolars were also extruded in groups I, II, and III (C-MP) (p < 0.05). There were significant differences between the groups with respect to vertical changes in the 1st premolars. The 1st premolar showed less change in group III (P1-MP) than in groups I and II (p < 0.05; Table 5, Figure 2).
For satisfactory treatment outcomes, orthognathic surgery patients clearly require presurgical orthodontic treatment. Capelozza Filho et al.2 reported a correlation between decompensation and the extent of mandibular reduction during surgery, as well as a strong correlation between cephalometric postsurgical mandibular excess and the lower anterior facial height. Precise treatment planning requires information on individual tooth movement and changes in arch dimensions; again, presurgical orthodontic treatment is a necessity.11 In the present study, the CBCT superimposition method was employed to provide a stable reference plane for assessment of mandibular tooth movement.
Ahn and Baek7 reported that incisors moved labially as a result of presurgical orthodontic treatment according to skeletal anteroposterior discrepancy and vertical type in 4 subgroups. Specifically, they concluded that the skeletal anteroposterior discrepancy/vertical type of patients resulted in differences in the extent and pattern of initial compensation, preoperative decompensation, and postoperative compensation of the lower incisors in Class III patients.7 In the present study, the extent of incisor movement between T0 and T1 stages was also determined. In groups I, II, and III, the results for anteroposterior incisor movement were consistent with those of Ahn and Baek.7 However, there were no significant differences between groups (p > 0.05). The vertical skeletal pattern did not affect the extent of labial incisor movement (Table 5, Figure 2).
Regarding vertical incisor movement, groups I and II showed extrusion after dental decompensation. In group III (patients with hypodivergent patterns), the vertical position of the incisors was maintained at the T1 stage. However, there were no significant differences between the groups (p > 0.05); though the incisors were extruded in groups I and II, the extent of vertical movement was no more than 1.5 mm. During dental decompensation, the mandibular incisors tended to move labially in groups I, II, and III and maintained their vertical positioning in the mandibular plane in group III.
We observed that the 1st and 2nd premolars and the 1st molars moved laterally in groups I, II, and III. In group III (patients with the hypodivergent pattern), the C-MSR increased only to the extent of the transverse change (Table 5, Figure 2; p < 0.05). Using cast model analysis, Nam et al.8 similarly reported that the inter-1st and 2nd premolar arch widths increased after surgery. However, they observed no significant differences in the intercanine or inter-1st molar widths. In contrast, the present study reports that the arch width changed during postoperative orthodontic treatment. Regarding canine movement, the hypodivergent skeletal pattern (group III) showed a distinct transverse change after dental decompensation, rather than anteroposterior or vertical changes (Table 5, Figure 2). The only anterior and vertical movements observed were in the hyperdivergent skeletal pattern (group I), and patients with normodivergent skeletal patterns (group II) showed only canine extrusion. In fact, distinct differences in canine movement patterns were apparent between the hyperdivergent and hypodivergent groups. These differences in movement might have been influenced by muscle forces, as patients in the hyperdivergent group typically have a much weaker occlusal force than those in the other groups.12
After dental decompensation, the 1st premolars moved in all 3 reference planes. This movement of the 1st premolars served to relieve crowding and level the mandibular arch with incisors. In contrast, the 1st molars did not show any distinct change, with the exception of an intermolar width increase. The movement of the 2nd premolars was similar to that of the 1st premolars and 1st molars, which is consistent with observations made in previous studies.8,13 However, other studies have not provided information on vertical and anteroposterior movements. The present study found that the skeletal facial pattern affected the vertical change of the 1st premolars. The hypodivergent group showed the least extrusion of the 1st premolars. Pandis et al.14 investigated the effects of leveling the curve of Spee on the inclination of the mandibular incisors and the width of the mandibular arch, concluding that the curve of Spee was mainly "flattened" by proclining the mandibular incisors. For 1 mm of leveling, the mandibular incisors were proclined 4 degrees, without increasing the arch width. Using the continuous archwire technique, Bernstein et al.15 concluded that leveling of the curve of Spee took place via a combination of premolar extrusion and (to a lesser extent) incisor intrusion. Our results also showed that the largest changes were in the incisors anteroposteriorly. However, the curve of Spee was also flattened by premolar extrusion. Furthermore, after dental decompensation, the incisors were not only proclined but also extruded. There have been several studies on incisor movement during leveling of the mandibular arch.16,17 In the present study, the incisors were mostly proclined and extruded or maintained and the premolars were extruded. The incisors and premolars reduced the curve of Spee.
Our results further indicate that the 1st molars maintained their original position after presurgical orthodontic treatment, with the exception of buccoversion. This result did not differ between the groups (Table 5, Figure 2; p < 0.05). The 1st molar, therefore, could be a key tooth with regards to anteroposterior movement for initial surgical treatment objectives.
There have been few successful cephalometric studies evaluating post-decompensation of the mandibular dentition, with the exception of the incisors and 1st molars. Rather, most have been limited to assessing the changes to the curve of Spee.15-17 In the present study, we evaluated post-decompensation mandibular tooth movement using the CBCT superimposition method. Our results indicate that changes to the mandibular arch during presurgical orthodontic treatment of skeletal Class III malocclusion are affected by the incisors, canines, 1st and 2nd premolars, and 1st molars. After dental decompensation, the mandibular arch indeed distinctly changed. Notably, movement of the mandibular incisors and premolars resolved the dental compensation.
The skeletal facial pattern did not affect dental decompensation except for the vertical change in the 1st premolars. Statistically, the hypodivergent group showed the least 1st premolar extrusion. However, this difference in 1st premolar extrusion according to vertical skeletal pattern was clinically insignificant.
Figures and Tables
 | Figure 1Superimposition, reference planes, and measurements for cone-beam computed tomography (CBCT) images. A, Registration areas for CBCT superimposition. B, Reorientation for reference plane settings. C, 3-dimensional cephalometric measurements. |
 | Figure 2Tooth movement (mm) after dental decompensation according to vertical skeletal pattern. Data are mean ± standard deviation. |
Table 5
Comparison of variables among groups according to skeletal patterns and changes between initial (T0) and presurgical (T1) stages

Hyper, Hyperdivergent group; Normo, normodivergent group; Hypo, hypodivergent group; IMPA, incisior mandibular plane angle; I1, incisor tip; Me, menton; Me-per, Me-perpendicular plane; C, canine tip; P1, 1st premolar; P2, 2nd premolar; M1, 1st molar; MP, mandibular plane; MSR, midsagittal reference plane.
*p < 0.05.
Notes
References
1. Johnston C, Burden D, Kennedy D, Harradine N, Stevenson M. Class III surgical-orthodontic treatment: a cephalometric study. Am J Orthod Dentofacial Orthop. 2006. 130:300–309.

2. Capelozza Filho L, Martins A, Mazzotini R, da Silva Filho OG. Effects of dental decompensation on the surgical treatment of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1996. 11:165–180.
3. Jacobs JD, Sinclair PM. Principles of orthodontic mechanics in orthognathic surgery cases. Am J Orthod. 1983. 84:399–407.

4. Proffit WR, Fields HW Jr, Sarver DM. Contemporary orthodontics. 2007. 4th ed. St.Louis: Mosby;705–710.
5. Wehrbein H, Bauer W, Diedrich P. Mandibular incisors, alveolar bone, and symphysis after orthodontic treatment. A retrospective study. Am J Orthod Dentofacial Orthop. 1996. 110:239–246.

6. Chung CJ, Jung S, Baik HS. Morphological characteristics of the symphyseal region in adult skeletal Class III crossbite and openbite malocclusions. Angle Orthod. 2008. 78:38–43.

7. Ahn HW, Baek SH. Skeletal anteroposterior discrepancy and vertical type effects on lower incisor preoperative decompensation and postoperative compensation in skeletal Class III patients. Angle Orthod. 2011. 81:64–74.

8. Nam HJ, Son WS, Park SB, Kim SS. Changes of mandibular dental arch during surgical-orthodontic treatment in skeletal class III malocclusion individuals. Korean J Orthod. 2008. 38:283–298.

9. Maes F, Collignon A, Vandermeulen D, Marchal G, Suetens P. Multimodality image registration by maximization of mutual information. IEEE Trans Med Imaging. 1997. 16:187–198.

10. Choi JH, Mah J. A new method for superimposition of CBCT volumes. J Clin Orthod. 2010. 44:303–312.
11. Cho MY, Choi JH, Lee SP, Baek SH. Three-dimensional analysis of the tooth movement and arch dimension changes in Class I malocclusions treated with first premolar extractions: a guideline for virtual treatment planning. Am J Orthod Dentofacial Orthop. 2010. 138:747–757.

12. Proffit WR, Fields HW, Nixon WL. Occlusal forces in normal- and long-face adults. J Dent Res. 1983. 62:566–570.

13. Lee HK, Son WS. A study on basal and dental arch width in skeletal Class III malocclusion. Korean J Orthod. 2002. 32:117–127.
14. Pandis N, Polychronopoulou A, Sifakakis I, Makou M, Eliades T. Effects of levelling of the curve of Spee on the proclination of mandibular incisors and expansion of dental arches: a prospective clinical trial. Aust Orthod J. 2010. 26:61–65.
15. Bernstein RL, Preston CB, Lampasso J. Leveling the curve of Spee with a continuous archwire technique: a long term cephalometric study. Am J Orthod Dentofacial Orthop. 2007. 131:363–371.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download