INTRODUCTION
Deglutition is a complex neuromuscular function involving structures in the oral cavity, pharynx, larynx, and esophagus. Normal deglutition is generally described in terms of 4 stages: the oral preparatory stage, oral stage, pharyngeal stage, and esophageal stage. While the first 2 stages are under voluntary control, the last 2 are involuntary and under reflexive control.
1-
3
The pharyngeal stage of deglutition is triggered by the propulsion of a bolus from the oral cavity into the pharyngeal cavity. This stage is complex and demands that the following series of events occurs in a timely fashion: superior and anterior displacement of the hyoid bone (HB) and thyroid cartilage, tilt and seal of the epiglottis, closure of the true and false vocal folds, opening of the upper esophageal sphincter (UES), and the contraction of pharyngeal constrictors to propel food or liquid through the pharynx and into the esophagus.
3,
4 Therefore, the anterior and superior displacement of the HB is essential for the protection of the airway during the swallow and for the safe and efficient passage of the bolus into the esophagus.
3,
5,
6 The synergistic occurrence of the contraction and relaxation of the suprahyoid muscles facilitates the displacement of the HB and tongue, pulls the larynx forward and upward, closes the epiglottis, and opens the UES, thereby permitting the bolus to enter the esophagus.
3,
7,
8
The suprahyoid muscles are attached to several craniofacial landmarks, such as the mandibular symphysis, the inferior border of the mandible, the base of the skull, and the tongue. As a result, craniofacial morphology affects the movement of the tongue and HB.
3,
7-
9
Previous studies have examined the impact of several factors, including age,
3,
10 sex,
10-
12 volume,
13,
14 type
15,
16 of material swallowed, and dysphagia,
15,
17 on the amount of HB displacement. For instance, Logemann et al.
10 have reported greater superior displacement among young male subjects than female subjects and greater anterior displacement among older women than younger women. Further, Ishida et al.
16 have reported that swallowing solids causes significantly greater superior and anterior displacement than swallowing liquids and that anterior displacement is significantly greater than superior displacement. Perlman et al.
15 reported that while swallowing solids, dysphagic patients exhibited less anterior and vertical displacement than normal subjects, although no such difference was observed between liquid and paste swallows. Both Cook et al.
13 and Dodds et al.
14 have shown that HB displacement increases with an increase in the bolus volume.
Many studies have demonstrated a significant correlation between craniofacial morphology and HB movement during swallowing.
7,
11,
12,
18-
20 Gay et al.
11 evaluated the swallowing function with bite blocks placed between the molars of male and female subjects. They hypothesized that morphological characteristics, specifically, the larger mandible in men, may play a role in the motor-control strategies employed during swallowing.
11 In another study examining the effects of an orthodontic crib on swallowing, Cuozzo and Bowman
20 determined that the distance between the HB and the mandibular plane increased after the use of the crib. Haralabakis et al.
12 found that the distance between the HB and the palatal plane is significantly greater among men with open bite than men with normal Class I occlusion. Zhou et al.
18 compared the swallowing patterns in adults with normal occlusion and those with skeletal class III malocclusion and determined that the tongue, HB, and mandible were positioned much lower in skeletal Class III patients than in normal individuals. Thus, although the abovementioned studies have demonstrated an association between craniofacial morphology and HB movement/characteristics, the nature of this association has not been explored in detail. Further, it is still unclear whether the degree of mandibular prognathism affects the initial position or movement patterns of the HB.
In addition to several other techniques,
1-
4,
7,
15,
18-
26 dynamic (cine) magnetic resonance imaging (MRI) is a non-invasive method that is now being used in the evaluation of the swallowing function.
1,
22-
25,
27,
28 We used this technique in the current study to determine the maximum swallowing-induced superior and anterior displacement of the HB in subjects with skeletal Class III malocclusion. Since the HB is attached to the mandible by the suprahyoid musculature, the movement of the HB can be affected by the anatomical variations in the size and position of the mandible during swallowing. We hypothesized that the degree of mandibular prognathism would correlate with HB movement.
MATERIALS AND METHODS
This study was initiated after obtaining institutional approval from the Gulhane Military Medical Academy's Ethics Committee. The study participants were selected from among patients referred to the Department of Orthodontics, Gulhane Military Medical Academy, Dental Science Center. Subjects were informed of the study procedure, but not the study aim, and all participants provided written informed consent. Cephalometric analysis was performed, and the subjects were grouped according to the following parameters: SNA angle (formed by the intersection of planes SN and NA), SNB angle (formed by the intersection of planes SN and NB), NVer-A distance (between the line drawn from points N and A perpendicular to FH), and NVer-Pog distance (between the line drawn from points N and Pog perpendicular to FH). The following groups were defined according to the degree of skeletal malformation:
Group 1: Mild Class III group (82° < SNB < 85°; -6 mm < NVer-Pog < 0 mm)
Group 2: Severe Class III group (85° < SNB; 0 mm < NVer-Pog)
Group 3: Class I (control) group (SNB = 80 ± 2°; NVer-Pog = -6 ± 1 mm)
The mild Class III group comprised 19 subjects (11 male, 8 female; age range, 18 - 25 years; mean age, 21.5 years); the severe Class III group, 16 subjects (10 male, 6 female; age range, 17 - 25 years; mean age, 19 years); and the Class I group, 20 patients (10 male, 10 female; age range, 17 - 24 years; mean age, 19.5 years).
None of the subjects had a micrognathic maxilla, bimaxillary protrusion (SNA = 82 ± 2°; NVer-A = 0 ± 1 mm), or a vertical facial high anomaly (S-Go/N-Me = 62 - 65%); further, none of them had any disorders capable of affecting swallowing, such as masticatory difficulty, dysphagia, neurological impairment, or degenerative diseases.
MRIs showing consecutive stages of deglutition were obtained for all participants. The subjects were examined in a supine position using a 1.5-Tesla superconducting MR scanner (The New Intera Nova; Philips Medical Systems, Best, Netherlands) with a standard quadrature head coil and Version 9 software. The system was equipped with magnetic field gradients with a maximum strength of 33 mT/m and a maximum slew rate of 160 T·m
-1 s
-1. In order to increase the signal intensity from the oropharynx and observe soft-tissue motion during bolus propulsion, 10 mL of water delivered with a syringe was used as a bolus. The subjects were instructed to swallow the entire volume when asked. Real-time, balanced turbo-field-echo (B-TFE) images (shortest TR/TE: 2.1/1.09 ms per excitation) were obtained in the midsagittal plane (defined as the section parallel to the interhemispheric fissure and identified by preliminary images), by using a 50° flip angle, 10-mm slice thickness, autoshim, 350 × 350-mm FOV, and a 96 × 96 matrix size. A total of 100 dynamic scans were obtained in 11 seconds. The acquired images were transferred to a system workstation (Easy Vision R4; Philips Medical Systems), and the image analysis and cine-MRI scans were performed offline on a workstation. The images were individually transferred by the image-capture program provided by the vendor and carefully evaluated to identify the anatomical landmarks visible for each patient (
Figures 1 and
2). The same specialist evaluated all the images and selected 4 images that best represented the 4 stages of deglutition. The following criteria were used to define each deglutition stage:
Stage 1 (oral preparatory stage): contact of the tongue tip with the maxillary incisors and/or palatal mucosa
Stage 2 (oral stage): loss of contact of the tongue dorsum with the soft palate
Stage 3 (pharyngeal stage): passage of the bolus head across the posterior/inferior margin of the mandibular ramus
Stage 4 (esophageal stage): passage of the bolus head through the esophageal opening (Figures 3, 4, and 5)
The 4 mid-sagittal images were selected and printed on radiographs, and anatomic landmarks (
Figure 1) and reference lines were plotted (
Figure 2) on the images by the same investigator, in order to assess the HB displacement. The vertical position of the HB was identified by measuring the distances H-S, H-NL, and H-C3RGN and the horizontal position of the HB, by the measurement of the distances H-C3 and H-RGN, as shown in
Figures 1 and
2. In order to minimize the effects of methodological errors in measurement, the measurements were repeated by the same researcher after a 10-day period, and the average of the 2 measurements was recorded. The paired sample t-test was used for the statistical analysis of a random selection of 50% of the samples, and no statistically significant differences were found between the 2 measurements (
p ≥ 0.05).
Statistical analysis was performed using the software MS Excel (Microsoft Co., Redmond, WA, USA) and SPSS for Windows version 15.0 (SPSS Inc, Chicago, IL, USA). The experimental subject was taken as the statistical unit of analysis, and the average values of the measurements made on each subject were processed accordingly. Descriptive values were calculated as means and standard errors. The normality of the distributions for the variables was measured using the Wilk-Shapiro normality test, which showed a normal distribution for vertical and horizontal distances between the HB and reference points. Repeated-measures multiple-way analysis of variance (MW-ANOVA) was used to assess measurements obtained for each stage, and Bonferroni post-hoc tests were performed to analyze any differences. The level of statistical significance was established as p < 0.05.
DISCUSSION
This study employed the relatively simple and noninvasive method of cine-MRI to elucidate the (1) HB location in patients with skeletal Class I occlusion and 2 different magnitudes of Class III malocclusions and (2) the mechanism of HB displacement during the 4 stages of deglutition. To eliminate the effects of age and sex
10 on the swallowing function, we conducted the study on a homogeneous population. Subjects were classified according to anteroposterior dentofacial discrepancies assessed on the basis of the SNA and SNB angles, as measured by Steiner cephalometric analysis. These angles are the most commonly used parameters in similar scientific studies, and their selection for this study was aimed at facilitating comparisons with other studies.
29 Additionally, the NVer-Pog distance was taken into consideration to determine the severity of skeletal Class III malocclusion. Only subjects with mandibular prognathism were included in the Class III groups. Subjects with anteroposterior maxillary deficiencies, retrognathism, or vertical facial anomalies were excluded from the study. Stable S, C3 point, and NL line measurements were considered as indicators of mandibular prognathism. A constant relationship is known to exist between the mandible and the HB.
9,
12 The location of the HB is determined by the musculature attached to the mandible through the influence of genioglossus muscle activity on tongue protrusion.
9 Consistently, this study revealed clear differences in the HB location between subjects with Class I occlusion and those with Class III malocclusions of different severities.
In this study, the deglutition process has been evaluated in 4 stages: oral preparatory, oral, pharyngeal, and esophageal, as is the general practice.
1,
2 Previous studies have been conducted using different bolus volumes
13,
14 and swallowing materials,
16 both of which have an effect on HB displacement. In the present study, however, a standardized bolus of 10 mL of water was used in order to easily identify the swallowing stages and monitor the swallowing patterns.
24
Deglutition has been investigated using a variety of techniques, including videofluoroscopy, cineradiography, surface electromyography (sEMG), electropalatography, electromagnetic articulography, and ultrasonography.
1-
4,
7,
15,
18-
26 Both cineradiography and videofluoroscopy have been reported to be acceptable methods for the assessment of deglutition; however, radiation exposure, the risk of barium aspiration, and the indirect visualization of structures render the use of these techniques questionable.
21,
23 Technical limitations related to skin/electrode impedance and individual variations in muscle depth and size are concerns restricting the use of sEMG.
24,
26 In the case of electropalatography, on the other hand, the acrylic plate base may affect the position and movement of the tongue during deglutition.
24,
25 Similarly, with electromagnetic articulography, the receiver coils may prevent subjects from swallowing normally.
21 Ultrasonography, although noninvasive, cannot be used to examine the pharynx or larynx because of skeletal interference.
24
A new technology known as cine-MRI, or kinetic MRI, helps obtain a series of anatomic images showing periodic motion, and it has been used effectively to evaluate different areas of the body during physiological movement.
1,
2,
23,
24 This promising dynamic diagnostic modality has the advantages of noninvasiveness, absence of radiation exposure, and the ability to image soft-tissue anatomy during motion in a multiplanar mode.
1,
2,
16,
24,
27,
28 Panebianco et al.
28 were able to obtain good-quality images using a temporal resolution of 3 - 4 slices/seconds, thereby demonstrating that dynamic MRI is a very promising tool in the evaluation of normal pharyngeal anatomy and physiology. Further, the availability of turbo fast low-angle shot acquisition provides the best anatomical and functional information available to evaluate the process of swallowing.
1,
24,
28 We chose to evaluate the movement of the HB by using dynamic MRI for its noninvasive nature and reliability, which have been successfully shown in previous studies.
1,
22,
24,
27,
28 Accordingly, a TFE sequence was implemented to evaluate the HB and related pharyngeal structures in the present study.
Despite the fact that the subjects in the present study were placed in the supine position during MRI imaging, the sequences obtained afforded clear visibility of the tongue and surrounding structures both during motion and at rest. Numerous reports in the literature
1,
22,
24,
27,
28 have referred to the use of kinetic MRI techniques for the evaluation of swallowing in the supine position. The tongue position and function may be affected when a subject is in the supine position, since the tongue can slip into the throat, making it difficult to swallow. In an MRI-based study conducted by Gilbert et al.,
22 tongue behavior during swallowing was examined by having subjects draw 5 mL of water into their mouths through a plastic tube and swallowing the entire volume on command while in a supine position. The results of this study were similar to those obtained in previous videofluoroscopy and ultrasonography studies in which the subjects were seated upright during swallowing. Moreover, a study by Pracharktam et al.
30 that used 2-dimensional cephalometry to examine the upper airway passage yielded similar information with subjects in both the supine and upright positions. While it is possible that the position of the subject may have affected tongue functioning in the present study, the effect would have been similar for all subjects, including controls, and would not have influenced intergroup comparisons. Nevertheless, the natural function of the tongue may have been influenced by the position of the subjects in this study and contributed to some extent to the differences between the results of this study and those obtained using other visualization techniques.
21,
27
The HB has previously been described as first moving upward, then forward, and then returning to its original position during swallowing.
17 In the present study, the obtained measurements showed that in all the groups, the HB was positioned most inferiorly at the beginning of the swallow, progressed superiorly from Stage 1 to Stage 2 and from Stage 2 to Stage 3, reached its most superior position at Stage 3, again moved inferiorly from Stage 3 to Stage 4, and then returned to its position at the start of Stage 1. Furthermore, the HB was shown to be positioned most posteriorly at Stage 1, moving anteriorly from Stage 1 to Stage 2, during which it attained its most anterior position; it then progressed posteriorly from Stage 2 through Stages 3 and 4 to return close to its original position at the start of the swallow (
Figure 6). In other words, the general path of motion of the HB during swallowing was similar in all groups, regardless of the nature of the occlusion.
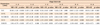
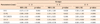
Previous studies have found vertical displacement of the HB to range from 1.3 to 1.9 cm during swallowing.
10,
17 Similar values for the vertical displacement of the HB were obtained in the current study, as indicated by the values of the parameter H-S (range, 99.75 - 110.06 mm in the mild Class III group; 101.17 - 115.11 mm, severe Class III group; and 95.85 - 105.05 mm, Class I group); horizontal displacement, assessed in terms of H-C3, was found to be less than the vertical displacement in all the groups (range, 37.67 - 40.94 mm, 40.06 - 43.56 mm, and 35.70 - 39.05 mm, respectively;
Table 1). These findings are consistent with those reported by Ishida et al.,
16 who found that the upward displacement of the HB during swallowing was less that its forward displacement.
In line with a number of previous studies demonstrating that variations in normal skeletal morphology affect HB movement,
7,
9,
11,
12,
18,
19 this study revealed that skeletal Class III malocclusion influences HB movement. The main finding was that the increase of the HB movement in accordance with the mandible and its related structures, since the initial location of the HB was more lower and frontal in the severe Class III group than the other groups. The paths of the HB and the tongue root were similar, which can be expected, given that the HB is attached to the tongue.
7-
9,
19
With a decrease in the magnitude of the Class III deformity, an increase was noted in the anterior and vertical displacements of the HB during swallowing. On comparing the swallowing patterns in adults, Zhou et al.
18 found that the tongue, the HB, and the mandible were positioned much lower in individuals with normal occlusion than in those with skeletal Class III malocclusion. In their study examining the relationship of the HB and posterior surface of the tongue in prognathism and micrognathia, Yamaoka et al.
9 found significant correlations between the posterior surface of the tongue and the position of the HB in skeletal Class III malocclusion. They also reported that the HB was protruded and positioned more anteriorly in individuals with mandibular protrusion compared to those with retrognathia. The findings of the present study were in agreement with the findings of both these earlier studies. Additionally, our study enabled the elucidation of the dynamic displacement of the HB during each stage of deglutition (
Figure 7).
While Class III malocclusion did not appear to affect the overall pattern of HB motion, the magnitude of skeletal Class III malocclusion was found to influence the degree of HB displacement. As expected, HB displacement was greater in patients with severe Class III malocclusion than those with mild Class III malocclusion as well as controls with normal occlusion. To obtain greater details of the information about the effects of malocclusion on swallowing patterns, it is necessary to conduct cine-MRI studies with larger sample sizes and samples that include different types of malocclusions.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download