Abstract
Objective
A national survey was conducted to assess orthodontic residents' current concepts and knowledge of cleft lip and palate (CLP) management in Korea.
Methods
A questionnaire consisting of 7 categories and 36 question items was distributed to 16 senior chief residents of orthodontic department at 11 dental university hospitals and 5 medical university hospitals in Korea. All respondents completed the questionnaires and returned them.
Results
All of the respondents reported that they belonged to an interdisciplinary team. Nineteen percent indicated that they use presurgical infant orthopedic (PSIO) appliances. The percentage of respondents who reported they were 'unsure' about the methods about for cleft repair operation method was relatively high. Eighty-six percent reported that the orthodontic treatment was started at the deciduous or mixed dentition. Various answers were given regarding the amount of maxillary expansion for alveolar bone graft and the estimates of spontaneous or forced eruption of the upper canine. Sixty-seven percent reported use of a rapid maxillary expansion appliance as an anchorage device for maxillary protraction with a facemask. There was consensus among respondents regarding daily wearing time, duration of treatment, and amount of orthopedic force. Various estimates were given for the relapse percentage after maxillary advancement distraction osteogenesis (MADO). Most respondents did not have sufficient experience with MADO.
An interdisciplinary team approach is usually required in order to achieve optimal treatment results for cleft patients. The success of this team approach depends on the expertise provided by team members in each discipline as well as the broad base of general knowledge about the cleft possessed by each member.1
A majority of cleft patients have severe dental problems, Class III malocclusion with maxillary hypoplasia, and a vertical growth pattern compared to that of noncleft normal patients.2-4 For cleft patients, orthodontic treatment should be started at an early age to provide presurgical infant orthopedics, to monitor facial growth and dental eruption, to determine the appropriate timing of surgical procedures, to position tooth-bearing bony segments as a framework for surgery, and to correct debilitating occlusal abnormalities.5 However, inadequacies in exposure to interdisciplinary teaching and the limited number of cases that are started and completed can be major problems in orthodontic training programs.6
Although there have been numerous surveys on cleft management,7-11 these studies have primarily focused on surgical care and alveolar bone grafting. Within the field of orthodontics, studies have investigated the motivation of individual orthodontists, the availability of cleft management program, the relationship of clefts to malocclusion, and the concerns related to public and private insurance.2,5,6,12,13 However, few studies have included a national survey on the concepts and knowledge of cleft management. Therefore, the purposes of this study were to assess the Korean orthodontic residents' current concepts and knowledge of cleft management as a reference or baseline for future surveys and to investigate any existing consensus in an effort to establish standard orthodontic training programs for cleft patients in Korea.
The questionnaire consisted of seven categories and 36 items covering basic information, presurgical infant orthopedics, methods and timing of cleft repair operation, early orthodontic treatment, maxillary expansion and alveolar bone graft, maxillary protraction with facemask, and maxillary advancement distraction osteogenesis. Respondents were able to provide more than one answers to several questions regarding the timing and method of specific treatment modalities.
The questionnaires were distributed to 16 senior residents of orthodontic department at 11 Dental University Hospitals (all of Dental University Hospital in Korea) and five major Medical University Hospitals in Korea. All respondents completed the questionnaires and returned them.
All of the major orthodontic training programs used an interdisciplinary team approach. Of the respondents, 75% reported that they are working with oral and maxillofacial surgeons (OMFS), while 25% reported that they are working with both OMFS and plastic surgeons (PS).
Nineteen percent of the respondents stated that they were using PSIO appliances at their university hospital to treat cleft patients (Table 1). The preferred PSIO appliances were the passive type appliance (Hotz plate, 40%) and the presurgical nasoalveolar molding appliance (PNAM, 40%). The active type appliance (Latham appliance) was only used by 20% of respondents (Figure 1). The PSIO appliance was applied to cleft babies either at their first visit to the clinic, regardless of age (67%) or at least 1 month after birth (33%; Table 1).
In terms of the operation timing of cleft lip (CL) repair, the majority of respondents replied that their surgeons performed cheiloplasty when infants were between 10 weeks and 3 months of age (46%) or between 3 and 6 months of age (23%; Figure 2A). Regarding the operation method of CL repair, 54% and 39% of them stated that their surgeons were using the Millard method in unilateral and bilateral CL repair, respectively. However, 39% and 61% of them, respectively, were unsure of the method preferred by their surgeons (Figure 2B and C).
In response to a question about the operation timing of cleft palate (CP) repair, 39% of the respondents answered that their surgeons performed palatorraphy between 12 to 18 months of age, while 38.5% of them were unsure (Figure 3A). Regarding the stage for CP repair, 54% of the respondents reported that their surgeons performed a two-stage repair, while 39% of them were unsure (Figure 3B). For the operation method of CP repair, 33% of the respondents replied that their surgeons used the von Langenbeck method, while 53% of them were unsure as to the method used by their surgeons (Figure 3C).
Early OT was started at the deciduous dentition (20%), early mixed dentition (40%), or late mixed dentition (26%; Figure 4A). Although various answers were provided, the two major goals of early OT, as reported on the multiple-choice questions, were correction of the anterior crossbite (88%) and resolution of the anterior mal-alignment (69%; Figure 4B).
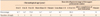
Diverse appliances were used for maxillary expansion of the cleft patients (quad-helix appliance, 44%; rapid maxillary expansion [RME] appliance, 38%; and removable plate, 31%) according to multiple-choice selections. Various answers were reported for the amount of cleft gap expansion between the upper permanent central incisor and deciduous canine (Table 2). These findings indicate that there is no consensus on the amount of cleft gap expansion that should be completed before ABG.
Regarding the ABG stage, 69% of the respondents replied that their surgeons preferred the secondary ABG, while none of them preferred the primary or tertiary ABG. However, 31% of them were unsure as to their surgeons' preference of the ABG stage (Table 3). In terms of the criteria of ABG timing, the preferred age and root development stage of the upper permanent canine (UPC) were between 9 and 12 years of age and between 1/2 and 3/4 of root development (73% and 93% of the respondents, respectively; Table 3). However, most of the respondents (88%) considered the root development status of both the upper permanent lateral incisor and canine to be more important than chronological age (Figure 5).
According to 93% of the respondents, the donor site for ABG was the iliac bone (Table 4). While 47% of the respondents replied that the particulated cancellous bone and marrow was used for ABG as autogenous bone graft material, 40% of them were unsure (Table 4). These findings indicate that further education of orthodontic residents is required to ensure appropriate knowledge of ABG materials.
For the estimate of the percentage of spontaneous eruption of UPC after ABG, 20% of the respondents thought that the probability was greater than 75%, whereas 53% of them were unsure (Figure 6A). Regarding the estimate of the percentage of window opening and forced eruption of the UPC after ABG, 33% of respondents answered that the probability was greater than 75%. However, 40% of them were unsure (Figure 6B). These findings indicate that there is no consensus among orthodontic residents regarding whether the UPC is erupted spontaneously after ABG.
As a preferred anchorage device for MP-FM, 67% of the respondents used RME appliance (Figure 7A). When the FM was used with RME, 50% of the respondents replied that MP was performed simultaneously with maxillary expansion, while 42% of them indicated that maxillary protraction was performed after completion of the maxillary expansion (Figure 7B). The infra-zygomatic crest was the preferred site for installation of the skeletal anchorage system for MP-FM in 69% of the respondents (Figure 7C).
Regarding the case experience of MADO for cleft patients, 31% of the respondents replied that they had experience with MADO for cleft patients, and all of them responded that the number of MADO cases was between one and five. These findings indicate that there is a significant difference in MADO experience among the hospitals. In addition, the majority of the respondents do not have sufficient experience with MADO.
When asked about the timing of MADO, 60% of the respondents replied that MADO should be performed when the cleft patients are between 10 and 15 years of age; whereas 40% of respondents indicated that MADO should be performed when the cleft patients are between 16 and 20 years of age (Figure 8A). The device types used for MADO were the intra-oral type in 60% of the respondents and the extra-oral type in 40% of them. The criteria for differential diagnosis of maxillary advancement with LeFort I osteotomy between conventional orthognathic surgery (COS) and MADO in cleft patients was identified as 5 to 7 mm by 60% of respondents and 7 to 9 mm by 40% of respondents (Figure 8B).
For the estimate of relapse percentage after maxillary advancement using COS in cleft patients, 40% of the respondents replied 21 to 30%, while 40% of them were unsure (Figure 8C). In addition, for MADO in cleft patients, the results were clearly diverse with 40% stating that they were unsure (Figure 8C). These findings indicate that there is no consensus regarding the relapse percentage after maxillary advancement when using either of these two techniques in cleft patients.
Since respondent's estimate of the percentage of cleft patients who require COS or MADO in spite of growth modification were extremely varied (Figure 8D), long-term follow-up studies will be needed to clarify.
The finding that all of the major orthodontic training programs in this survey employed an interdisciplinary team approach is distinctly different from that of a previous survey result of Korean PS residents (36%).11 This suggests that accessibility to orthodontic treatment is easier in dental university hospitals than in medical university hospitals. Furthermore, the percentage of cowork with OMFS was higher than that of PS in this study (75% vs. 25%). This appears to be due to the specific relationship between orthodontics and OMFS in dental university hospital in Korea.
The PSIO appliances were used by only 19% of the respondents (Table 1), a considerably lower percentage than that reported by Eom and Lee (61%).11 It is possible that the PS surgeons referred cleft babies only to experienced orthodontists in dental university hospitals or local clinics. Another consideration is that the PSIO appliance is not currently popular with orthodontists in Korea. The PSIO appliances preferred in this study (PNAM, 40% and Hotz plate, 40%; Figure 1) were different from those reported by Eom and Lee (PNAM, 43% and Latham appliance; 30%).11
Regarding the operation timing for CL repair, orthodontic residents in this study have a similar concept with PS residents in the study by Eom and Lee11 (46% vs. 43%, between 10 weeks and 3 months of age, Figure 2A). Although there was no difference in the most preferred operation method of CL repair (the Millard method), there were differences between this study and Eom and Lee11 in the percentages of the Millard method (54% vs. 94% in unilateral CL repair; 39% vs. 54% in bilateral CL repair; Figure 2B and 2C). These differences seem to be due to the percentage of "unsure" respondents in this study (39% in unilateral CL repair; 61% in bilateral CL repair; Figure 2B and 2C).
In determining the timing of CP repair, the balance between maxillary growth and speech development must be taken into consideration. Because there has been a concept of delayed hard palate closure for better long-term outcome of maxillary growth,14 54% of the respondents reported that their surgeons performed a two-stage repair for CP (Figure 3B). However, 90% of the PS residents reported that they closed the hard and soft palate simultaneously.11 In the present study, fewer than 10% of the respondents reported that their surgeon was performing one-stage repair for CP (Figure 3B). The preferred operation method for CP repair showed a difference between responses of the orthodontic residents in the present study (33%, von Langenbeck method, Figure 3C) and those of the PS residents in a previous study (56%, double-opposing Z-plasty).11 Since there were differences in the concept of cleft repair between our study and a previous study11 and a shortage of knowledge on surgical methods on the part of the orthodontic residents (Figures 2 and 3), communication and education regarding the concept and surgical methods of cleft repair are required for orthodontic residents.
For the timing of early OT for cleft patients, 86% of the respondents replied that they started treatment at the deciduous or mixed dentition (Figure 4A), which is similar to the results of Eom and Lee.11 Regarding the concept of ABG stage, all of the respondents in this study, except those that were "unsure", replied that their surgeons preferred the secondary ABG. A similar result was reported by Murthy and Lehman.10 For the criteria of ABG timing, the preferred patient age for ABG was between nine and 12 years of age (73%, Table 3), while Murthy and Lehman10 reported that the preferred patient age for ABG was between six and nine years of age (77%). The reason for this difference seems to be lack of consensus with respect to dental criteria for ABG timing. The majority of respondents in this study (88%) considered that the root development status of both the upper permanent lateral incisor and canine is more important than chronological age when selecting the optimal time for ABG (Figure 5). Most of the respondents in this study replied that the iliac bone was the donor site for ABG (93%, Table 4), which is consistent with the results of Murthy and Lehman10 and Eom and Lee.11
da Silva Filho et al.15 reported that the percentages of spontaneous eruption and window opening/forced eruption of UPC after ABG were 72% and 6%, respectively. This implies that the probability of spontaneous eruption of the UPC was under-estimated by the respondents in the present study because only 20% of the respondents believed that it would be more than 75% (Figure 6A). The possibility of window opening/forced eruption of the UPC was over-estimated by the respondents in this study because 33% of the respondents thought that it would be more than 75% (Figure 6B). These results demonstrate that orthodontic residents lack the proper statistical evidence and/or consensus regarding the eruption status of the UPC after ABG.
FM therapy has been applied to treat growing Class III patients with mild to moderate maxillary hypoplasia. Recently, the skeletal anchorage system has been introduced to maximize the skeletal effects of the treatment and to minimize the unwanted dento-alveolar side effects of the FM therapy.16 Baek et al.16 suggested 500 g of force per side and 12 to 14 hours of daily use for effective FM therapy.
Saelen et al.17 insisted that maxillary advancement of more than 6 mm with COS revealed significant relapse six months after surgery. Therefore, a criterion for differential diagnosis of maxillary advancement with LeFort I osteotomy between COS and MADO in CLP patients may be the amount of advancement that is greater than 6 mm. In this study, 60% of the respondents answered that this criterion was 5 to 7 mm; and 40% replied that it should be 7 to 9 mm (Figure 8B). Although the amount of maxillary advancement in MADO is usually larger than that of COS in cleft patients, the relapse rates of the maxillary advancement with COS and DO are known to be in similar and range between 20% and 25%.18-20 However, 40% of the respondents stated that they were unsure of the relapse rates. Therefore, there was no consensus as to the relapse percentage after maxillary advancement using these two techniques in cleft patients (Figure 8C). Although DeLuke et al.21 reported that 25% of patients required orthognathic surgery because of the anteroposterior discrepancy, there was also no consensus of opinion regarding the percentage of cleft patients who require surgical correction (Figure 8D). This particular discrepancy requires a longitudinal sample study with proper consistent orthopedic and growth modification treatment, and growth evaluation protocols.
Since this study is the first to outline the survey results of cleft management in orthodontic residents, the data obtained from this study can be used as a reference or baseline for future surveys and the establishment of standard orthodontic training programs for the treatment of cleft patients in Korea. In addition, more extensive survey of participants in orthodontic training programs should be performed at regular intervals to assess both basic and current concepts and knowledge in the diagnosis and treatment of cleft patients.
Figures and Tables
 | Figure 2Cleft lip (CL) repair. A, Operation timing; B and C, operation method for unilateral and bilateral CL. |
 | Figure 6Estimates of the percentage of eruption of the upper permanent canine after alveolar bone grafting. A, Percentage of spontaneous eruption; B, percentage of window opening and forced eruption. |
 | Figure 7Maxillary protraction with facemask (MP-FM). A, Preferred anchorage device; B, preferred method of the maxillary expansion when using MP-FM with a rapid maxillary expansion appliance; C, preferred site for installation of the skeletal anchorage system; D, average treatment duration. REM, Rapid maxillary expansion. |
 | Figure 8Surgical correction for cleft patients. A, Timing of maxillary advancement distraction osteogenesis (MADO); B, criteria for differential diagnosis of maxillary advancement with LeFort I osteotomy between conventional orthognathic surgery (COS) and MADO; C, estimates of relapse percentage after COS (gray) and MADO (black); D, estimates of the percentage of cleft patients who require COS and MADO in spite of growth modification. |
Table 1
Percentage of the use of presurgical infant orthopedics (PSIO) prior to cheiloplasty and the timing of the first application of the device
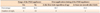
Table 2
Expansion amount of the cleft gap between the upper central incisor and canine in cleft patients before alveolar bone grafting

Table 3
Preferred chronological age and root development stage of the upper permanent canine for the timing of alveolar bone grafting
References
1. Thornton JB, Nimer S, Howard PS. The incidence, classification, etiology, and embryology of oral clefts. Semin Orthod. 1996. 2:162–168.
2. Hongal SG, Ankola A, Nagesh L. Malocclusion and treatment needs of cleft lip and/or palate subjects aged between 12 and 18 years visiting KLE's Hospital, Belgaum, India. Oral Health Prev Dent. 2010. 8:237–242.
3. Baek SH, Moon HS, Yang WS. Cleft type and Angle's classification of malocclusion in Korean cleft patients. Eur J Orthod. 2002. 24:647–653.

4. Seo YJ, Park JW, Kim YH, Baek SH. Initial growth pattern of children with cleft before alveolar bone graft stage according to cleft type. Angle Orthod. 2011. 81:1103–1110.

5. Lewis CW, Ose M, Aspinall C, Omnell ML. Community orthodontists and craniofacial care: results of a Washington state survey. Cleft Palate Craniofac J. 2005. 42:521–525.

6. Noble J, Schroth B, Hechter FJ, Huminicki A, Wiltshire WA. Motivations of Orthodontic Residents in Canada and the US to Treat Patients with Craniofacial Anomalies, Cleft Lip/Palate and Special Needs. Cleft Palate Craniofac J. 2011. [Epub ahead of print].
7. Osborn JM, Kelleher JC. A survey of cleft lip and palate surgery taught in Plastic Surgery Training Programs. Cleft Palate J. 1983. 20:166–168.
8. Brennan PA, Macey-Dare LV, Flood TR, Markus AF, Uppal R. Cleft lip and palate management by U.K. consultant oral and maxillofacial surgeons: a national survey. Cleft Palate Craniofac J. 2001. 38:44–48.

9. Weinfeld AB, Hollier LH, Spira M, Stal S. International trends in the treatment of cleft lip and palate. Clin Plast Surg. 2005. 32:19–23.

10. Murthy AS, Lehman JA. Evaluation of alveolar bone grafting: a survey of ACPA teams. Cleft Palate Craniofac J. 2005. 42:99–101.

11. Eom JS, Lee TJ. Changing trends in cleft lip and palate management taught in training programs in Korea. J Craniofac Surg. 2011. 22:430–433.

12. Tang EL, So LL. Prevalence and severity of malocclusion in children with cleft lip and/or palate in Hong Kong. Cleft Palate Craniofac J. 1992. 29:287–291.

13. Williams AC, Sandy JR, Shaw WC, Devlin HB. Consultant orthodontic services for cleft patients in England and Wales. Br J Orthod. 1996. 23:165–171.

14. Friede H. Maxillary growth controversies after two-stage palatal repair with delayed hard palate closure in unilateral cleft lip and palate patients: perspectives from literature and personal experience. Cleft Palate Craniofac J. 2007. 44:129–136.

15. da Silva Filho OG, Teles SG, Ozawa TO, Filho LC. Secondary bone graft and eruption of the permanent canine in patients with alveolar clefts: literature review and case report. Angle Orthod. 2000. 70:174–178.
16. Baek SH, Kim KW, Choi JY. New treatment modality for maxillary hypoplasia in cleft patients. Protraction facemask with miniplate anchorage. Angle Orthod. 2010. 80:595–603.
17. Saelen R, Tornes K, Halse A. Stability after Le Fort I osteotomy in cleft lip and palate patients. Int J Adult Orthodon Orthognath Surg. 1998. 13:317–323.
18. Baek SH, Lee JK, Lee JH, Kim MJ, Kim JR. Comparison of treatment outcome and stability between distraction osteogenesis and LeFort I osteotomy in cleft patients with maxillary hypoplasia. J Craniofac Surg. 2007. 18:1209–1215.

19. Posnick JC, Dagys AP. Skeletal stability and relapse patterns after Le Fort I maxillary osteotomy fixed with miniplates: the unilateral cleft lip and palate deformity. Plast Reconstr Surg. 1994. 94:924–932.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download