Abstract
Purpose
Gastrostomy is commonly used procedures to provide enteral nutrition support for severely handicapped patients. This study aimed to identify and compare outcomes and complications associated with percutaneous endoscopic gastrostomy (PEG) and surgical gastrostomy (SG).
Methods
A retrospective chart review of 51 patients who received gastrostomy in a single tertiary hospital from January 2000 to May 2016 was performed. We analyzed the patients and the complications caused by the procedures.
Results
Among the 51 patients, 26 had PEG and 25 had SG. Four cases in the SG group had fundoplication for gastroesophageal reflux disease. PEG and SG groups were followed up for an average of 29 months and 44 months. Major complications occurred in 19.2% of patients in the PEG group and 20.0% in the SG group, but significant differences between the groups were not observed. Minor complications occurred in 15.4% of patients in the PEG group and 52.0% in the SG group. Minor complications were significantly lower in the PEG group than in the SG group (p=0.006). The average use of antibiotics in the PEG and SG groups was 6.2 days and 15.7 days (p=0.002). Thirteen patients died of underlying disease but not related to gastrostomy, and only one patient died due to complications associated with general anesthesia.
Severely handicapped patients who cannot meet their nutritional requirements by oral food intake alone require long-term enteral access with a gastrostomy tube. Surgical gastrostomy (SG) is an insertion method that has been commonly performed using the Stamm technique. SG is considered the safest method for enteric access. In 1980, The first percutaneous endoscopic gastrostomy (PEG) technique was introduced; PEG rapidly became one of the most preferred methods because of its minimally invasive nature, speed, low cost, and high patient tolerance [12]. Recently, other minimally invasive methods have been introduced including laparoscopic approach, radiographically guided percutaneous gastrostomy, and laparoscopic-assisted PEG [34].
Compared with elderly patients, gastrostomy feeding positively affects the growth of neurologically impaired children, as well as the quality of life of both children and their caregivers [56]. The parents of neurologically impaired children are frequently faced with the decision of having their child receive gastrostomy tube placement. Almost all caregivers have difficulties in choosing among the different tube placement techniques, and healthcare professionals must correctly inform the exact pros and cons of each gastrostomy technique. The primary objective of this study is to describe and compare the outcomes and complications associated with PEG and SG. The secondary objective is to suggest a proper gastrostomy method to patient's caregiver according to patient's individual clinical condition.
We performed a retrospective chart review of 51 patients who received gastrostomies at the Chonbuk National University Hospital from January 2000 to May 2016. These patients underwent either PEG or SG during the period. The medical records of these patients were reviewed. The differences in age, sex, underlying disease, complications, previous NG-tube usage, duration of antibiotics, death, fundoplication, post-procedural follow-up lengths, and anti-epileptic drug intakes of the patients were analyzed. This study was performed by the approval of the Institutional Review Board of Chonbuk National University Research Council (IRB no. CUH 2016-07-021).
The PEG procedure was performed at the endoscopy center in the pediatrics department. The patients who received gastrostomy fast at least 8 hours prior to the procedure and waited at least 24 hours after placement to begin feeding using a gastrostomy tube. Sedative endoscopic procedures were performed under moderate sedation using intravenous midazolam (0.05 to 0.1 mg/kg) or ketamine (0.5 to 1 mg/kg), except few cases performed under general anesthesia due to patient's unstable underlying conditions. In surgical procedures, all cases are operated under general anesthesia in the operating room. All endoscopic and SG procedures were administered intravenous prophylactic antibiotics before the procedure. Patient education on feeding via gastrostomy tube and stoma site management was conducted until discharge.
After an antiseptic skin preparation was applied to the abdomen, an endoscopic fiber with a snare was inserted into the stomach by passing through the patient's mouth. The stomach was inflated with air, which resulted in close apposition of the stomach to the abdominal wall, and the abdominal wall was transilluminated by the light of the scope. A small skin incision was performed, and a guidewire was passed into the stomach. This guidewire was snared by the gastroscope and removed back through the oral cavity, and a gastrostomy tube was then tied to this guidewire. The tube was pulled back down through the oral cavity to the stomach. The gastrostomy tube was pulled outside through the abdominal wall and fixed [78].
The general preparation is similar to the pull technique. After the endoscope was inserted and the appropriate site had been marked, three T-fastners were placed to secure the stomach to the anterior abdominal wall. A guidewire was then inserted through the incision, and dilators were passed over the guidewire. Finally, the gastrostomy tube was passed into the stomach through the abdominal wall from the outside. This method avoids passing the gastrostomy tube from the patient's oral cavity through the digestive tract into the stomach [9].
SG is difficult to perform properly in patients who have underlying gastrointestinal malformations, especially tracheo-esophageal fistula. A gastrostomy tube was placed using the standard Stamm gastrostomy technique through a midline incision. Sometimes this technique was combined with a standard open Nissen fundoplication when the esophageal refluxes of the patient were objectively proven by endoscopy or 24-hour esophageal pH test or clinical symptoms, such as frequent aspiration, to prevent the occurrence of esophagitis and aspiration pneumonia caused by the gastro-esophageal refluxes.
Pearson's chi-square test or Fisher's exact test was conducted to analyze statistically significant relationships of categorical data. Comparisons of continuous data were performed using the Mann-Whitney test. All statistical analyses were performed with PASW Statistics ver. 18.0 for Windows (IBM Co., Armonk, NY, USA). p<0.05 was considered statistically significant.
Fifty-one patients underwent gastrostomy between January 2000 and May 2016. A total of 26 patients underwent PEG (51.0%; male, 16; female, 10; mean age, 14.1 years) and 25 patients received SG (49.0%; male, 17; female, 8; mean age, 5.7 years). Six patients (11.8%; PEG, 1; SG, 5) were below 1 year old. In the PEG group, 22 patients (84.6%) used nasogastric tube feeding before gastrostomy and in the SG group, 20 patients (80.0%). Four of the twenty-five patients who underwent SG (16.0%) also had fundoplication. The PEG and SG groups were followed up for an average of 29 months and 44 months, respectively. Sixteen patients (61.5%) took anti-epileptic drugs at the time of gastrostomy placement in the PEG group and sixteen patients (64.0%) in the SG group (Table 1).
The indications for gastrostomy insertion are shown in Fig. 1. Clinical indications of patients who required gastrostomy insertion are trauma, hypoxic injury, congenital anomaly, degenerative disease, central nervous system infection, and others (drug intoxication, epilepsy). The most common indication in the PEG group is disability caused by trauma, such as brain hemorrhage (42.3%), and in the SG group is hypoxic injury (40.0%) (Fig. 1).
Twelve of the fifty-one patients had esophageal condition or esophagogastric junction state as revealed by endoscopy prior to gastrostomy procedure (PEG and SG). Meanwhile, all the remaining esophageal conditions of the PEG group were identified with PEG procedure. Five of the fifty-one patients (9.8%) in both PEG and SG groups confirmed acid reflux events by 24-hour pH and impedance monitoring. Two of them received fundoplication procedures at the time of SG placement, and two patients who were clinically suspected with gastric reflux underwent fundoplication (Table 1).
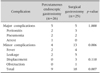
Major complications, such as peritonitis, pneumonia, and respiratory arrest, occurred in 19.2% of the patients in the PEG group (5/26) and 20.0% of the patients in the SG group (5/25). Minor complications occurred in 15.4% of the patients in the PEG group (4/26) and 52.0% of the patients in the SG group (13/25). Minor complications include tube displacement, fever without major complications associated with gastrostomy infection that was treated with systemic antibiotics, peristomal leakage, and tubal obstruction. No significant difference was observed in the incidence of major complications (p=1.000). However, the major complication of a “Cardiopulmonary arrest” occurred only in the PEG group after general anesthesia and sustained intubated state due to unstable respiration. Finally, the patient had respiratory arrest and died.
Significant differences were observed in minor (p=0.006) and overall complication (p=0.007) incidences. The minor complication of “tube displacement” and “tube obstruction” occurred only in the SG group before the first discharge after gastrostomy tube placement. Early complications (occurred within 7 days after the procedure was performed) occurred in 26.9% of the patients in the PEG group (7/26) and 20.0% of the patients in the SG group (5/25), and late complications (occurred after 7 days) occurred in 7.7% of the patients in the PEG group (2/26) and 52.0% of the patients in the SG group (13/25). Significant differences were observed in complications associated with their onset time in late period (p=0.001; Table 2 and 3).
The PEG group used antibiotics for an average of 6.2 days and the SG group for 15.7 days. Thus, the use of antibiotics after gastrostomy procedure was significantly lower in the PEG group compared with the SG group (p=0.002; Table 1). The patients were administered intravenous injection of cefazolin (first generation cephalosporin).
PEG is less invasive than SG for providing semi-permanent enteral access. In this study, complication rates of 34.6% after PEG and 72% after SG were observed. These results compare favorably to other published rates of pediatric PEG complications that range from 12.4% to 54.7% and to SG rates that range from 56% to 79% in literature [101112]. In 1988, Grant [2] reviewed 125 PEG and 88 SG performed in adults at a single center and showed lower complication rates (PEG, 8.8%; SG, 23.9%) than those previously mentioned in pediatric literature. The difference may be due to varied patient demographics and the relative difficulty of the procedural skill, as well as risk in maneuver gastrostomy placement in small patients than in adults [13].
Since the introduction of PEG in 1980, it became the modality of choice for long-term enteral access in adults [1]. Despite its generally safe results, PEG is still associated with many potential complications. Neurologically handicapped children are particularly high risk for both endoscopic and surgical post-procedural complications. This retrospective study found that PEG technique showed significantly lower incidences in minor (p=0.006) and overall (p=0.007) complication rates than the surgical group. Although the incidences of major complication between the two groups (PEG vs. SG) showed no significant difference, one patient in the PEG group died due to patient's aggravated respiratory condition at post-operative day 5. This patient took general anesthesia for PEG placement and eventually died due to respiratory failure. In this study, unlike all patients in SG group underwent general anesthesia, only 3 cases in the PEG group underwent general anesthesia due to patient's unstable basal condition and one patient expired and others who underwent general anesthesia in PEG group show no complication. This result shows the high risk potential of general anesthesia to the neurologically handicapped patients. Except for the above case, 12 patients died during the observation period as a consequence of the underlying disease but not as a result of gastrostomy placement.
Most endoscopic procedures including PEG placement in children are performed with deep sedation or general anesthesia to ensure patient's safety and comfort [1415]. PEG has a number of advantages compared with SG, other than reduced complications and duration of antibiotic use. Since PEG is a simple and less invasive method, it can be performed at an endoscopy unit, and an operating room is not necessary. General anesthesia is often not required for PEG, but it is necessary for most cases of SG [1617]. Almost all PEG procedures in children are commonly performed jointly by a gastroenterologist and a general surgeon in the operating room under general anesthesia in the United States [1819]. In our pediatric center, most pediatric gastrointestinal procedures including PEG placement are commonly carried out using deep sedation without general anesthesia at an endoscopy unit.
This study population was restricted to severely handicapped patients, and most of them are sufficient to be diagnosed as cerebral palsy. Cerebral palsy patients require careful consideration for their disabilities including gastrointestinal and respiratory systems. Decreased airway tone and increased risk of aspiration are frequent in neurologically handicapped patients, and a medical practitioner must focus on patients identified as high risk for aspiration during induction and endotracheal extubation [20]. Generally, epilepsy is present in approximately 30% of cerebral palsy patients [21]. In this study, 32 of 51 patients (62.7%) took anti-epileptic drugs, and the general anesthesia in these patients may aggravate the frequency and duration of seizure activity. Cerebral palsy patients with comorbid epilepsy have higher risk to experience a perioperative seizure activity than noncerebral palsy epileptic patients who underwent surgery. In 2012, Wass et al. [22] examined 800 pediatric and adult cerebral palsy patients who underwent surgery with general anesthesia. The risk of complications was 63%, and pediatric patients had a greater number of complications compared with adults. We suggest that the difference in sedation method could be strongly related to the complications after procedure according to the condition of patient.
The push type PEG technique has recently became well known in PEG tube placement and possesses advantages in infections. Several retrospective series have compared the pull and push methods [23]. In general, the pull-through PEG is technically easier, and the push PEG exhibits an overall significantly higher rate of complications, dislocations, and occlusions. However, a recent study showed that the overall incidence of complications in the push technique is lower than that in the pull technique in the study by Tucker et al. [23]. In the present day, we have performed all pediatric PEG cases by using the push method (5 cases) in our pediatric department since 2014. Only one case showed minor complications, and the overall outcome is excellent. However, more large number of cases is needed for statistical analysis.
An increasing number of gastrostomies are placed when children are dependent on a nasogastric tube for enteral nutrition for long periods [24]. The method of insertion was based on the recommendation by a pediatrician, a gastroenterologist, and a treating surgeon. Thus, medical practitioners who have responsibilities to treat their patients must explain to children's caregiver which methods are the most suitable and safest for each patient. Although the SG group showed more complications in this study, some patients who have congenital malformations of the gastrointestinal tract and need fundoplication to avoid frequent aspiration due to gastroesophageal refluxes, as well as those who have failed endoscopy, have no choice. The gastrostomy formation of these patients must be performed through SG formation with fundoplication procedure. Due to the retrospective nature of this study, there are limitations of gathering clinical data from reviewing previous chart. Many enteral access methods, such as laparoscopic and radiological methods, are recently introduced and increasingly used to substitute for the classic PEG and SG. In our institution, only one case of laparoscopic gastrostomy placement was recently performed in a pediatric patient. Further studies need to compare various gastrostomy placements in a large group to help patients and their caregivers to select more appropriate options and improve their satisfaction.
In conclusion, both PEG and SG methods can cause some complications, but the endoscopic method is safer and has shorter antibiotic use than the surgical method because of it can avoid the complications of general anesthesia. However, enteral route must be placed in some of the patients through surgical method because of basic clinical conditions, such as tracheo-esophageal fistula and gastrostomy formation with fundoplication, which are due to frequent gastric reflux events. If possible, we suggest early PEG procedure without general anesthesia for handicapped children. Medical professionals must convince the parents that gastrostomy feeding is a safe method that must be placed early to prevent malnutrition and improve the global health status of the patient.
Figures and Tables
ACKNOWLEDGEMENTS
This work was supported by the Research Institute of Clinical Medicine, Chonbuk National University Hospital.
References
1. Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980; 15:872–875.

2. Grant JP. Comparison of percutaneous endoscopic gastrostomy with Stamm gastrostomy. Ann Surg. 1988; 207:598–603.

3. Stringel G, Geller ER, Lowenheim MS. Laparoscopic-assisted percutaneous endoscopic gastrostomy. J Pediatr Surg. 1995; 30:1209–1210.

4. Reiner DS, Leitman IM, Ward RJ. Laparoscopic stamm gastrostomy with gastropexy. Surg Laparosc Endosc. 1991; 1:189–192.
5. Cook S, Hooper V, Nasser R, Larsen D. Effect of gastrostomy on growth in children with neurodevelopmental disabilities. Can J Diet Pract Res. 2005; 66:19–24.

6. Smith SW, Camfield C, Camfield P. Living with cerebral palsy and tube feeding: a population-based follow-up study. J Pediatr. 1999; 135:307–310.

7. Gang MH, Kim JY. Short-term complications of percutaneous endoscopic gastrostomy according to the type of technique. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:214–222.

8. McSweeney ME, Smithers CJ. Advances in pediatric gastrostomy placement. Gastrointest Endosc Clin N Am. 2016; 26:169–185.

9. Lucendo AJ, Friginal-Ruiz AB. Percutaneous endoscopic gastrostomy: an update on its indications, management, complications, and care. Rev Esp Enferm Dig. 2014; 106:529–539.
10. Chang SH, Kim DY, Kim SC, Kim IK, Kim KM. Complications of percutaneous endoscopic gastrostomy (PEG) in children. Korean J Pediatr Gastroenterol Nutr. 2004; 7:8–15.

11. Liu R, Jiwane A, Varjavandi A, Kennedy A, Henry G, Dilley A, et al. Comparison of percutaneous endoscopic, laparoscopic and open gastrostomy insertion in children. Pediatr Surg Int. 2013; 29:613–621.

12. Fox VL, Abel SD, Malas S, Duggan C, Leichtner AM. Complications following percutaneous endoscopic gastrostomy and subsequent catheter replacement in children and young adults. Gastrointest Endosc. 1997; 45:64–71.

13. ASGE Standards of Practice Committee. Lightdale JR, Acosta R, Shergill AK, Chandrasekhara V, Chathadi K, et al. Modifications in endoscopic practice for pediatric patients. Gastrointest Endosc. 2014; 79:699–710.

14. Fredette ME, Lightdale JR. Endoscopic sedation in pediatric practice. Gastrointest Endosc Clin N Am. 2008; 18:739–751,ix.

15. van Beek EJ, Leroy PL. Safe and effective procedural sedation for gastrointestinal endoscopy in children. J Pediatr Gastroenterol Nutr. 2012; 54:171–185.

16. Miller RE, Kummer BA, Tiszenkel HI, Kotler DP. Percutaneous endoscopic gastrostomy: procedure of choice. Ann Surg. 1986; 204:543–545.
17. Wasiljew BK, Ujiki GT, Beal JM. Feeding gastrostomy: complications and mortality. Am J Surg. 1982; 143:194–195.

18. El-Matary W. Percutaneous endoscopic gastrostomy in children. Can J Gastroenterol. 2008; 22:993–998.

19. McSweeney ME, Jiang H, Deutsch AJ, Atmadja M, Lightdale JR. Long-term outcomes of infants and children undergoing percutaneous endoscopy gastrostomy tube placement. J Pediatr Gastroenterol Nutr. 2013; 57:663–667.

20. Rudra A, Chatterjee S, Sengupta S, Iqbal A, Pal S, Wankhede R. The child with cerebral palsy and anaesthesia. Indian J Anaesth. 2008; 52:397–403.
21. Maranhão MV. Anesthesia and cerebral palsy. Rev Bras Anestesiol. 2005; 55:680–702.
22. Wass CT, Warner ME, Worrell GA, Castagno JA, Howe M, Kerber KA, et al. Effect of general anesthesia in patients with cerebral palsy at the turn of the new millennium: a population-based study evaluating perioperative outcome and brief overview of anesthetic implications of this coexisting disease. J Child Neurol. 2012; 27:859–866.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download