Abstract
Mesenteric cysts are rare intra-abdominal lesions occurring during childhood, which were first described in 1507. Cases of mesenteric cysts have been continuously reported, but these cases were very small in number. They are often asymptomatic and incidentally found while patients are undergoing work-up or receiving treatment for other conditions such as appendicitis, small-bowel obstruction, or diverticulitis; however, patients may still have lower abdominal pain and symptoms that are frequently associated with other abdominal conditions. The symptoms are variable and non-specific, including pain (82%), nausea and vomiting (45%), constipation (27%), and diarrhea (6%). An abdominal mass may be palpable in up to 61% of patients. We are to report the clinical course and literature of a child with mesenteric cysts who complained of acute abdominal pain, distension, and vomiting and were surgically treated after being diagnosed with mesenteric cysts based on radiological examination.
Mesenteric cysts are rare intra-abdominal lesions that occur during childhood, which may vary in presentation from an asymptomatic mass to an acute abdomen. They can occur anywhere in the mesentery of the gastrointestinal tract from the duodenum to the rectum and may extend from the base of the mesentery to the retroperitoneum [1]. Incidences of pediatric mesenteric cyst are very low (lower than adult cases) [2]. Moreover, the rarity of this condition is one of the causes of incorrect preoperative diagnosis. In this report, we present a case of mesenteric cyst on the proximal ileum of a patient with abdominal pain.
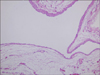
A previously healthy 4-year-old boy was transferred to our hospital from a primary clinic complaining persistent vomiting, abdominal pain, and an abdominal mass. He didn't have any other symptoms such as fever, jaundice, melena, or hematemesis. There was no familial record of any similar symptoms or history. Vital signs such as blood pressure, heart rate, respiratory rate, body temperature were all in normal ranges. However, on physical examination, bowel sounds were decreased, and a 10-cm-sized mass was palpable in the lower abdomen. It was freely movable and apparently fluctuant. There was no tenderness. Blood test results found that hemoglobin level was 12.5 g/dL; white blood cell was 8,930 /µL with 84.2% neutrophil and 12.0% lymphocyte; platelet count was 301,000 /µL; erythrocyte sedimentation rate was 10 mm/h; C-reactive protein level was 6.73 mg/L. Liver function tests, basic metabolic panel, amylase and lipase levels, and urinalysis were within normal limits. In an abdominal ultrasonography to rule out intussusception, a large cystic lesion was found surrounded by a thin wall superior to the bladder, composed of homogenous fluid material inferior to the umbilicus; no solid lesion was observed (Fig. 1). Abdominal computed tomography (CT) revealed a low attenuated intra-abdominal cystic mass measured as 12 cm in diameter with thin intracystic septations (Fig. 2). He was transferred to the general surgery department for operation. Intraoperatively, the cyst was resected with the attached small bowel. A grossly unicystic mass was found, and the intestinal serosa was intact with a thin cystic wall measuring 9×8.5×4.2 cm, 152 g (Fig. 3). Immunohistochemical markers were negative. Histopathology of the mesenteric cystic wall shows a single layer of epithelial lining surrounded by fibrous structure. And the final pathophysiologic result was a lymphatic mesenteric cyst (Fig. 4). He made a good clinical recovery without complications after the operation. He was discharged home on the fifth post-operative day. There was no recurrence or complications during the follow-up period for one year.
A mesenteric cyst is defined as any cyst in the mesenterium. It was initially described by the Italian pathologist Antonio Benivieni during the autopsy of an 8-year-old child in 1507 [13]. Cases of mesenteric cysts have been reported continuously, but these cases were very small in number; thus, the etiology of mesenteric cysts has not been ascertained exactly. Mesenteric cyst may vary in size from a few centimeters to over 10 cm [4]. Its location is within the mesentery of the small intestine, most frequently followed by the mesentery of the colon and retroperitoneum [5]. In a review series of 162 patients, 60% of mesenteric cysts occurred in the small-bowel mesentery, 24% in the large-bowel mesentery, and 14.5% in the retroperitoneum [267].
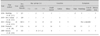
Mesenteric cyst is usually asymptomatic, but it can be accompanied by gastrointestinal symptoms which make it misunderstood as appendicitis, small bowel obstruction, or diverticulitis, before operation. Complications such as rupture, torsion, or intestinal obstruction rarely occur, which cause more severe symptoms [89]. According to a large review of the literature by de Perrot et al. [10], pain (82%), nausea and vomiting (45%), constipation (27%), or diarrhoea (6%) were the presenting symptoms while an abdominal mass was the clinical finding in up to 61% of the patients. There were also non-specific symptoms in this case, such as abdominal pain, distension, and vomiting. It is likely that young patients under the age of 10 take less time to show some symptoms compared with patients aged over 10 [6]. Various clinical characteristics were shown at the recent case series reports of mesenteric cysts in pediatric patients (Table 1) [911121314]. Nearly no case in childhood has been reported in Korea.
Because mesenteric cyst in childhood is occasionally accompanied by symptoms like pain, history taking and physical examination should be performed precisely, and radiologic findings such as abdominal ultrasound (USG) and CT scan are important. According to study of Senocak et al. [15], abdominal USG by experienced hands is the most reliable diagnostic tool, and CT scan should be performed additionally in a suspected case. USG and CT of the abdomen can distinguish between solid and cystic characteristics of abdominal mass.
Mesenteric cyst has a possibility of secondary complications such as hemorrhage, torsion, obstruction, or infection, hence complete excision of cyst with or without bowel resection is the procedure of choice to prevent recurrence or malignant transformation [616]. Once the cyst is removed, it recurs rarely, and the prognosis of the patient is usually excellent. Recurrence is reported to be higher after partial wall excision and drainage than after total excision. There are little reports of malignant cysts at childhood yet. According to Kurtz et al. [6], only 3% of mesenteric cysts were malignant, all of which were found in adults.
In conclusion, we reviewed the clinical course and literature of a child with mesenteric cysts who complained of acute abdominal pain, distension, and vomiting and were surgically treated after being diagnosed with mesenteric cysts based on radiological examination.
Figures and Tables
Fig. 1
Ultrasonography scans showing a large unicystic mass that has a well-defined wall with anechoic lesion. On an abdominal ultrasonography, a large cystic lesion was found with a thin wall superior to the bladder, composed of homogenous fluid material inferior to the umbilicus.
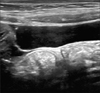
Fig. 2
Abdominal computed tomography (CT) scan showing a large unicystic mass with fine septations (about 12 cm×11 cm). A low attenuated intra-abdominal unicystic mass was found in an abdominal CT, measured as 12 cm in diameter with thin intracystic septations.
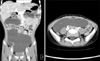
Fig. 3
Operative photograph showing a giant mesenteric cyst. An unicystic mass was found grossly, and the intact intestinal serosa was found with a thin cystic wall measuring 9×8.5×4.2 cm.

Fig. 4
Histopathology of the mesenteric cystic wall; a single layer of epithelial lining surrounded by fibrous structure (H&E, ×100). A single layer of epithelial lining surrounded by fibrous structure was found at the histopathology of the mesenteric cyst which was a lymphatic mesenteric cyst at the final result.
References
1. Dequanter D, Lefebvre JC, Belva P, Takieddine M, Vaneukem P. Mesenteric cysts. A case treated by laparoscopy and a review of the literature. Surg Endosc. 2002; 16:1493.
2. Chung MA, Brandt ML, St-Vil D, Yazbeck S. Mesenteric cysts in children. J Pediatr Surg. 1991; 26:1306–1308.

3. Mohanty SK, Bal RK, Maudar KK. Mesenteric cyst--an unusual presentation. J Pediatr Surg. 1998; 33:792–793.

4. Richard RR. Mesenteric and omental cysts. In : Grosfeld JL, O'Neill JA, Coran AG, Fonkalsrud EW, editors. Pediatric surgery. 6th ed. Philadelphia: Mosby Elsevier;2006. p. 1399–1406.
5. Vanek VW, Phillips AK. Retroperitoneal, mesenteric, and omental cysts. Arch Surg. 1984; 119:838–842.

6. Kurtz RJ, Heimann TM, Holt J, Beck AR. Mesenteric and retroperitoneal cysts. Ann Surg. 1986; 203:109–112.

7. Saviano MS, Fundarò S, Gelmini R, Begossi G, Perrone S, Farinetti A, et al. Mesenteric cystic neoformations: report of two cases. Surg Today. 1999; 29:174–177.

8. Marte A, Papparella A, Prezioso M, Cavaiuolo S, Pintozzi L. Mesenteric cyst in 11-year old girl: a technical note. Case report. J Pediatr Surg. 2013; 1:84–86.

9. Prakash A, Agrawal A, Gupta RK, Sanghvi B, Parelkar S. Early management of mesenteric cyst prevents catastrophes: a single centre analysis of 17 cases. Afr J Paediatr Surg. 2010; 7:140–143.

10. de Perrot M, Bründler M, Tötsch M, Mentha G, Morel P. Mesenteric cysts. Toward less confusion? Dig Surg. 2000; 17:323–328.
11. Makhija D, Shah H, Tiwari C, Jayaswal S, Khedkar K, Waghmare M. Mesenteric cyst(s) presenting as acute intestinal obstruction in children: three cases and literature review. Int J Pediatr Adolesc Med. 2016; DOI: 10.1016/j.ijpam.2016.04.003.

12. Siva kumar S, Kireeti AS, Mohan TV. Giant mesenteric cysts of large intestine in children: two case reports and review of the literature. J Dent Med Sci. 2015; 14:93–95.
13. Chang TS, Ricketts R, Abramowsky CR, Cotter BD, Steelman CK, Husain A, et al. Mesenteric cystic masses: a series of 21 pediatric cases and review of the literature. Fetal Pediatr Pathol. 2011; 30:40–44.

14. Rattan KN, Nair VJ, Pathak M, Kumar S. Pediatric chylolymphatic mesenteric cyst-a separate entity from cystic lymphangioma: a case series. J Med Case Rep. 2009; 3:111.

15. Senocak ME, Gündoğdu H, Büyükpamukçu N, Hiçsönmez A. Mesenteric and omental cysts in children. Analysis of nineteen cases. Turk J Pediatr. 1994; 36:295–302.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download