Abstract
Ingestion of foreign body in children is a relatively common problem among paediatric population. The foreign bodies mostly pass spontaneously through the gastrointestinal tract. However, complications can occur according to its anatomical location, the characteristics of the foreign body, and delays in management. Although the cases of ingested button batteries or sharp objects impacted at the gastrointestinal tract can be very serious, there have been very only a few cases have reported colonoscopic removal of these dangerous foreign bodies in adults, and there have been no case reports in children. We report one case of a button battery and one case of an open safety pin, both impacted in the terminal ileum that had moved from the stomach within a few hours of ingestion and were eventually managed by colonoscopy without any complications.
Accidental ingestion of a foreign body in children is a relatively common problem, and objects such as ingested batteries mostly pass spontaneously through the gastrointestinal system. But, in about 20% of cases, foreign body ingestion causes complications according to their shape, size or the children's medical status, and thus requiring endoscopic or surgical removal [1]. In particular, button batteries and sharp foreign bodies can be life threatening and difficult to manage by endoscopy. If button cell is retained in the gastrointestinal tract or sharp foreign body is ingested, they can be fatal and most cases require endoscopic retrieval before they move from the stomach to the intestine [2].
To date, there have been no reports on the management of a button battery impacted in the terminal ileum or the colon, having already passed the stomach, and only a few cases have been reported on the endoscopic retrieval of a foreign body in the small intestine or the colon in adults [345].
We report on a case of an ingested disc battery and another case of a sharp foreign body impacted around the ileocecal (IC) valve, separating the small intestine from the colon. Colonoscopic retrieval was successfully performed for both cases.
A 4-year-old girl was admitted 1hr after unintentional swallowing of a 15-mm-sized disc battery. She was previously healthy and had no other medical history. Her vital signs were stable. Her height was 103 cm (50-75th percentile); weight was 20 kg (90-95th percentile). She did not show signs of nausea, vomiting and abdominal pain. The abdomen was soft and flat with normoactive bowel sounds. There was neither tenderness nor rebound tenderness on the abdomen.
On laboratory examination, only a mild leukocytosis of 11,800/mm3 was revealed. Simple abdominal radiograph showed the radiopaque disc battery in the stomach (Fig. 1A). We anticipated spontaneous passage and decided to follow up with additional serial abdominal radiographs. Those revealed that the battery had migrated from the stomach to the IC valve (Fig. 1B). But, 3 days later, the battery still remained at the IC valve with the follow-up abdominal X-ray picture (Fig. 1C).
Colonoscopic examination on the 3rd admission day revealed that the disc battery still remained stagnant at the same site at the terminal ileum near the IC valve. However, the disc was not accessible due to a large amount of feces in the cecum. After proper bowel preparation using a lavage, colonoscopy was performed again on the 4th admission day. By using a magnet probe attached to the scope, the disc battery was retrieved successfully with minimal mucosal bleeding (Fig. 2). The child was discharged on the following day without any complications (Fig. 1D).
A 10-month-old girl had ingested an open safety pin and visited an outside hospital. Abdominal X-ray revealed an open safety pin in the esophagus, and the child was transferred to our medical center for endoscopic removal of the foreign body 6 hours after having swallowed the object. She was previously healthy and had no other medical history. Her vital signs were stable. Her height was 73.4 cm (25-50th percentile); weight was 9 kg (25-50th percentile). She did not show any signs of nausea, vomiting, or abdominal pain. Her abdomen was soft and flat. There was no tenderness or rebound tenderness. Her bowel sounds were normal.
On laboratory examination, only a mild leukocytosis of 20,400/mm3 and mild liver enzyme elevation (46 U/L) was revealed. Simple abdominal radiograph showed a radiopaque 2-cm-sized open safety pin in the stomach (Fig. 3A). We immediately performed an endoscopy but could not find any foreign body in the stomach or the duodenum. We decided to follow up with abdominal radiographs every 6 hour. In the follow up abdominal X-ray, the open safety pin was visible in the lower abdomen (Fig. 3B). The next morning, the open safety pin was located at the right lower abdomen, but serial abdominal radiographs revealed the safety pin had migrated to the IC valve (Fig. 3C). Three days later, the pin still remained in the right lower abdomen near IC valve on serial abdominal X-ray (Fig. 3D).
Colonoscopy was performed on the 4th admission day and revealed the open safety pin stuck in the IC valve (Fig. 4). The pin was then successfully removed by using a tripod forceps and abdominal X-ray after colonoscopy revealed no free air (Fig. 3E). The child remained asymptomatic after colonoscopic retrieval and was discharged without any complications three days later.
In pediatric populations, ingestion of foreign bodies frequently occurs. Most ingested foreign bodies naturally pass through the gastrointestinal tract without any clinical sequelae or damage [6]. However, in about 20% of cases, the objects require endoscopic retrieval and 1% of cases may finally require surgical removal. This rate depends on the type of the foreign body, its location, the patient's age, and duration of impaction [78].
Ingestion of button batteries accounts for up to 13% of all foreign body ingestions [9], and it is a special condition, requiring urgent intervention [10]. If the button batteries remain in the gastrointestinal tract, it can cause ulceration, perforation, eventually leading to fistula formation or even death [11]. To date, four mechanisms have been suggested about injury caused by button batteries: leakage of battery contents causing corrosive damage, low voltage burns, pressure necrosis on tissues, and metal toxicity [12].
A button battery impacted in the esophagus needs to be urgently removed, because esophageal injuries can occur within two hours of ingestion, whereas those in the stomach and bowel can be managed conservatively for cases where the patient is presented asymptomatically [13]. However, battery impaction within the intestine or the occurrence of symptoms also requires urgent endoscopic retrieval [7]. Moreover, button batteries with a large diameter (≥20 mm) in children younger than 4 years is more likely to have higher morbidity and mortality [13], whereas most of the small-sized button batteries pass the gastrointestinal tract within 2-6 days [14]. The recent report suggested indication for the observation of ingested foreign body as follows; absence of symptom, children older than 5 years, smaller battery (<20 mm), and short duration of ingestion (<2 hours) [15].
In our case, a button battery with a diameter of 15mm was found in stomach at first presentation and moved to terminal ileum and remained stationary for about 24 hours, but it stayed at the same site for an additional three days without any progress. Even though our patient was 4 years old, an initial observation was decided as she was asymptomatic. However, after confirming the impacted position of the button battery at the IC valve location, colonoscopic retrieval was tried and performed successfully. On colonoscopy, only mild erosion was observed possibly because the disc battery was not so old enough to leak.
Sharp objects are also known as one of the most commonly ingested foreign bodies in children. In a prospective study, 10% of all 244 ingested foreign bodies were identified as sharp objects including straight pins, open safety pins and hairbrush bristles [16]. Ingested sharp objects can cause a variety of complications such as perforation, abscess, peritonitis, fistula formation, appendicitis, aorto-esophageal fistula, and death [17]. If a sharp object is located in the esophagus, it should be removed as soon as possible. Once identified, optimal management depends on the location and type of the foreign body, and the rate of success depends on the skill of the endoscopist and the endoscopic devices such as retrieval forceps, retrieval net, and polypectomy snare [7]. However if the patient is small and weighs less than 5 kg, there would be a limit in using some of the devices [18].
In our case, button battery and open safety pin was both found in the stomach at first presentation and moved to the terminal ileum near IC valve within a day, but they stayed at the same site for an additional three days without any progress. After confirming the impacted button battery and the open safety pin at the IC valve area, colonoscopic retrieval was tried to remove the intestinal foreign body. We could remove the disc battery and the open safety pin successfully using a magnetic probe and a tripod forceps,
respectively, without any complications.
About 1% of ingested foreign body may eventually need surgical removal; however, there have been only a few cases reported on sigmoidoscopic or colonoscopic retrieval of an impacted object at the gastrointestinal tract in adults and children. In case of disc battery, there have been no reports in children to date [345]. If impacted foreign bodies at the gastrointestinal tract be within the scope of endoscopic approaches, colonoscopic removal may be helpful in young children to avoid invasive surgical treatment.
Figures and Tables
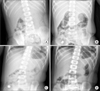 | Fig. 1(A) Abdominal radiograph on day 1 showing the disc battery in the stomach. (B) Day 3 X-ray showing that the disc battery had moved to the ileocecal valve. (C) Abdominal radiograph just before the colonoscopic retrieval, revealing long stagnation of the disc battery at the same site. (D) Skiagram after the colonoscopic retrieval, indicating a successful removal without any complications. |
 | Fig. 2(A) An ingested button battery observed in the terminal ileum and then moved to the cecum during colonoscopy. (B) A button battery successfully removed by using a magnetic probe during colonoscopy. (C) Magnetic probe used to remove a button battery. |
 | Fig. 3(A) Abdominal radiograph on day 1 showing a 2-cm-sized open safety pin in the stomach. (B) At 6 hours post-admission, the open safety pin had moved to the lower abdomen. (C) Abdominal X-ray on day 2 shows the open safety pin at the right lower abdomen. (D) Serial X-ray just before the colonoscopic retrieval on day 3, revealed an impacted open safety pin at the same site near the ileocecal valve. (E) Abdominal X-ray after colonoscopic retrieval showed only paralytic ileus without any complications. |
 | Fig. 4(A) An open safety pin found in the cecum during colonoscopy. (B) Foreign body removal was tried initially by using an alligator forceps but failed. (C) A tripod forceps used to remove an open safety pin. (D) An open safety pin was successfully removed by using a tripod forceps during colonoscopy. (E) After removing an open safety pin from the cecum, minor mucosal injury was observed at the site of foreign body impaction. (F) An open safety pin successfully removed by using a tripod forceps during colonoscopy. |
References
1. Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002; 55:802–806.

2. Chang JJ, Yen CL. Endoscopic retrieval of multiple fragmented gastric bamboo chopsticks by using a flexible overtube. World J Gastroenterol. 2004; 10:769–770.

3. Tarnasky PR, Newcomer MK, Branch MS. Colonoscopic diagnosis and treatment of chronic chicken bone perforation of the sigmoid colon. Gastrointest Endosc. 1994; 40:373–375.

4. Vemula NR, Madariaga J, Brand DL, Hershey H. Colonoscopic removal of a foreign body causing colocutaneous fistulas. Gastrointest Endosc. 1982; 28:195–196.

5. Viceconte G, Viceconte GW, Bogliolo G, Pietropaolo V, Dell'Anna A, Montori A. Endoscopic removal of foreign bodies in the large bowel. Endoscopy. 1982; 14:176–177.

6. Lyons MF 2nd, Tsuchida AM. Foreign bodies of the gastrointestinal tract. Med Clin North Am. 1993; 77:1101–1114.

7. Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995; 41:39–51.

8. Ginsberg GG, Pfau PR. Foreign bodies and bezoars. In : Feldman M, Friedman LS, Sleisenger MH, editors. Sleisenger and fordtran's gastrointestinal and liver disease: pathophysiology/diagnosis/management. London: Saunders;2002. p. 395–397.
9. Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr. 2001; 160:468–472.

10. Hachimi-Idrissi S, Corne L, Vandenplas Y. Management of ingested foreign bodies in childhood: our experience and review of the literature. Eur J Emerg Med. 1998; 5:319–323.
11. Chang YJ, Chao HC, Kong MS, Lai MW. Clinical analysis of disc battery ingestion in children. Chang Gung Med J. 2004; 27:673–677.
12. Litovitz T, Whitaker N, Clark L, White NC, Marsolek M. Emerging battery-ingestion hazard: clinical implications. Pediatrics. 2010; 125:1168–1177.

15. Kramer RE, Lerner DG, Lin T, Manfredi M, Shah M, Stephen TC, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr. 2015; 60:562–574.
16. Paul RI, Christoffel KK, Binns HJ, Jaffe DM. Foreign body ingestions in children: risk of complication varies with site of initial health care contact. Pediatric Practice Research Group. Pediatrics. 1993; 91:121–127.

17. Paul RI, Jaffe DM. Sharp object ingestions in children: illustrative cases and literature review. Pediatr Emerg Care. 1988; 4:245–248.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download