Abstract
Purpose
Acid neutralization during chemical clearance is significantly prolonged in children with cystic fibrosis, compared to symptomatic children without cystic fibrosis. The absence of available reference values impeded identification of abnormal findings within individual patients with and without cystic fibrosis. The present study aimed to test the hypothesis that significantly more children with cystic fibrosis have acid neutralization durations during chemical clearance that fall outside the physiological range.
Methods
Published reference value for acid neutralization duration during chemical clearance (determined using combined impedance/pH monitoring) was used to assess esophageal acid neutralization efficiency during chemical clearance in 16 children with cystic fibrosis (3 to <18 years) and 16 age-matched children without cystic fibrosis.
Results
Duration of acid neutralization during chemical clearance exceeded the upper end of the physiological range in 9 of 16 (56.3%) children with and in 3 of 16 (18.8%) children without cystic fibrosis (p=0.0412). The likelihood ratio for duration indicated that children with cystic fibrosis are 2.1-times more likely to have abnormal acid neutralization during chemical clearance, and children with abnormal acid neutralization during chemical clearance are 1.5-times more likely to have cystic fibrosis.
Conclusion
Significantly more (but not all) children with cystic fibrosis have abnormally prolonged esophageal clearance of acid. Children with cystic fibrosis are more likely to have abnormal acid neutralization during chemical clearance. Additional studies involving larger sample sizes are needed to address the importance of genotype, esophageal motility, composition and volume of saliva, and gastric acidity on acid neutralization efficiency in cystic fibrosis children.
Gastroesophageal reflux (GER) is a physiologic process that occurs in most individuals following a meal when the increased intra-abdominal pressure causes relaxation of the lower esophageal sphincter and subsequent release of gastric contents into the esophagus. Clearance of the refluxed bolus following a GER episode occurs in two phases. In the first phase, the rapid volume clearance removes the bulk of the refluxed bolus by peristalsis and gravity when positioned upright. In the second phase, chemical clearance restores the esophageal mucosa to pre-reflux conditions [1]. During chemical clearance of acid GER (AGER) episodes, the acidified esophageal mucosa is neutralized by swallowed bicarbonate-rich saliva [2] and/or by bicarbonate secreted into the esophageal lumen from esophageal submucosal glands within the esophageal body [345678]. In healthy individuals, these processes occur efficiently and in a timely manner. GER disease (GERD) occurs when physiological GER results in symptoms, such as heartburn, coughing and choking, laryngitis, difficulty swallowing, vomiting, and chronic pulmonary infections. Studies in infant humans [9], adult humans [1011] and in animals [11] suggest that impaired chemical clearance may be a primary pathophysiological mechanism for GERD. Acid neutralization is achieved when the acidified esophageal mucosa reaches pH 4 [12]. Fig. 1 depicts a classic AGER episode as measured using combined multichannel intraluminal impedance and pH (MII-pH) monitoring.
Children with cystic fibrosis (CF) are known to have increased GER, presumably due to the dynamics that predispose this patient population to GER; these include frequent coughing, hyperinflation of the chest causing an increased pressure gradient between the chest abdomen, delayed gastric emptying, high-fat diets, frequent feedings (grazing), and vest treatments used to break up the mucous in the airways [1314]. All of these can cause the lower esophageal sphincter to relax and release gastric contents into the esophagus.
In a study aimed at comparing GERD children with and without CF using combined MII-pH monitoring, we reported that while the impedance metrics appeared to be similar between the two cohorts, the duration of acid neutralization during chemical clearance was significantly prolonged in the CF cohort (123 seconds vs. 66 seconds, p=0.001) [15]. Unfortunately, the study was limited by the absence of available acid neutralization reference values that could be used to assess individual subjects for abnormal findings.
Using data derived from symptomatic children (ages 1 to <18 years) who were referred for symptoms suggestive of GER as an etiology, but had AGER in the normal physiologic range (<3%) and had no significant symptom-GER associations, we derived reference values for acid neutralization during chemical clearance [16].
Based on our previous study showing significantly prolonged acid neutralization during chemical clearance in children with CF compared to children without CF [17], we hypothesized that children with CF would be significantly more likely to have acid neutralization during chemical clearance that was outside of the physiological range. The present study aimed to use the published reference value for acid neutralization duration [15] to: 1) identify individual patients (within both groups) for whom the duration of acid neutralization during chemical clearance was outside the physiological range, 2) determine whether symptomatic children with CF were more likely to have “abnormal” acid neutralization during chemical clearance, and 3) assess the prospective predictive potential of the acid neutralization duration for identifying previously undiagnosed CF children.
This study included 16 children with CF (3 to<18 years) and 16 age-matched children without CF. Previously calculated mean durations for each patient [15] were compared to the recently published acid neutralization duration reference value [16]. Median duration for both cohorts was also compared to the published reference value. Acid neutralization durations were calculated using MII-pH monitoring [15].
For both CF and non-CF cohorts, mean values (for acid neutralization duration) that exceeded the physiologically normal range were considered abnormal. The published threshold value was 114.4 seconds for acid neutralization.
All analyses were conducted using SAS ver. 9.3 (SAS Institute, Cary, NC, USA) with two-sided p-values <0.05 considered to be significant. Since CF patients were matched by age to non-CF patients, McNemar's test for paired proportions was used to determine whether CF patients were more likely to have abnormal acid neutralization (duration) during chemical clearance. Area under the receiver operator characteristic curve (AUC), sensitivity, specificity, and likelihood ratio statistics were computed for using acid neutralization (duration) to potentially diagnose CF. Median (25th-75th quartile) values for CF and non-CF cohorts were compared using signed rank test.
The proportion of abnormal acid neutralization during chemical clearance was compared by CF status using chi-square and Fisher's exact tests. This part of the design was no longer a case-control study, since the matching was done by exposure and not outcome, and thus a paired analysis was not used.
This study was approved by the Institutional Review Board at Nationwide Children's Hospital prior to its execution (IRB no. 08-00195).
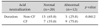
Brief demographics of the cohort are included in Table 1, and a full description of subject symptoms have been previously published [15]. When we compared the median durations of acid neutralization during chemical clearance to the reference value (114.4 seconds) (123 seconds [CF] vs. 66 seconds [non-CF]), acid neutralization during chemical clearance was abnormal for children with CF but normal for the children without CF.
When a 114.4 seconds threshold duration was used to assess CF and non-CF cohorts, 9 of 16 (56.3%) children with CF and 3 of 16 (18.8%) children without CF were determined to have abnormal durations (p=0.0412, Table 2).
We also found that a greater proportion of CF patients had abnormal acid neutralization during chemical clearance when we considered abnormal acid neutralization as a function of CF status (Table 3). CF status has fairly good ability to discriminate between patients who have normal vs. abnormal acid neutralization during chemical clearance (AUC=0.70). Based on likelihood ratio values (positive test), patients with CF are 2.1-times more likely to have abnormal acid neutralization during chemical clearance when duration is considered (Table 3).
The duration of acid neutralization during chemical clearance discriminate moderately well between CF and non-CF patients, as evidenced by the relatively high AUC value (0.69). If duration of acid neutralization during chemical clearance were used as a biomarker to identify CF, it would have sensitivity (true positive) of 75% and specificity (true negative) of 65%. The likelihood ratio (positive) for acid neutralization duration indicates that patients with abnormal acid neutralization during chemical clearance are 1.5-times more likely to have a CF diagnosis.
Hundreds of children are referred to our facility annually for symptoms suggestive of GER as an etiology. Among them are children with CF. Given that children with CF are known to have increased GER [18], we have sought to outline the differences between symptomatic children with and without CF so that we can differentiate and treat the children with CF appropriately and expeditiously. In a previous study, we compared two symptomatic pediatric cohorts (CF and non-CF) and found that while the majority of impedance parameters were not different between the two groups, the duration of acid neutralization during chemical clearance was significantly prolonged in the CF cohort [15]. Unfortunately, at the time of the study, there were no available reference values for acid neutralization during chemical clearance. Consequently, we had no way of knowing: 1) whether the prolonged acid neutralization was outside the physiologic range (i.e., abnormally prolonged), and 2) whether some or all children with CF had abnormal acid neutralization during chemical clearance. To fill this gap, we subsequently derived reference values for acid neutralization during chemical clearance [16].
The results of the present study show that not all children with CF have abnormally prolonged acid neutralization during chemical clearance. Children with CF, however, are more likely to have abnormal acid neutralization during chemical clearance. Given the fact that delays in acid neutralization during chemical clearance are likely to be the pathophysiological mechanism of GERD [910192021], our data indicating that children with CF are more likely to have prolonged acid neutralization during chemical clearance (2.1-times when considering acid neutralization duration) supports a clinical approach such that children with CF who present with GERD symptoms would likely benefit from acid neutralization assessment.
A review of the literature reveals that there is a population of CF patients who are not diagnosed in infancy using the CF newborn screening test for immunoreactive trypsinogen. These individuals, roughly 1.7-5.4% of the total, are identified at older ages and with varying severity of illness [22]. Given our initial observation that CF children (as a group) have prolonged acid neutralization during chemical clearance [15], we hypothesized that assessments of acid neutralization during chemical clearance could be used to identify previously undiagnosed CF children. While prolonged acid neutralization duration during chemical clearance may not be diagnostic of CF (sensitivity 75% and specificity 65%), the combined results of this study suggest that further CF evaluation should be considered in children with prolonged acid neutralization; particularly, in children who present with any of the common CF disease sequelae or history, such as nasal polyp removal, recurring pneumonias, etc. Other recent studies suggest that prolonged acid exposure may be related to the progression of mucosal damage during GERD [9101123], suggesting a mechanism for esophageal injury in CF patients with prolonged acid neutralization during chemical clearance.
In this and in previous studies [1524], we assessed chemical clearance by evaluating acid neutralization during chemical clearance of AGER. Acid neutralization is but one component of chemical clearance, i.e., the period during which the esophageal mucosa is being returned to pre-reflux conditions. While efficient acid neutralization is important for preventing esophageal mucosal damage, removal of injurious gastric and duodenal molecules, such as pepsin and bile acids, is equally important. Recently, a novel pH-impedance parameter has been used to assess chemical clearance in adults. This parameter, known as the post-reflux swallow-induced peristaltic wave (PSPW) index, describes the percentage of total impedance-detected GER episodes during which the first post-reflux peristaltic wave (a swallow) occurs within 30 seconds [1025]; the higher the PSPW index, the more efficient the chemical clearance. This new method shows promise for assessment of chemical clearance during acid, weakly acidic, and weakly alkaline GER episodes. Further work is needed to assess the efficacy of these impedance-pH parameters for assessing chemical clearance in children. Being able to identify children with abnormal chemical clearance, by either assessing acid neutralization or by calculations of PSPW Indices, will permit timely implementation of appropriate clinical management strategies for symptomatic children with and without CF.
This study has some limitations. First, the sample size is small. It is clear that the statistics would have benefited from a larger sample size. The narrow group of CF genotypes was also unfortunate. It is possible that our observations are unique to the present study and cannot be extrapolated to other patient populations. Second, the chemical clearance reference used to assess the patient values were generated using symptomatic patients who had a negative pH probe result on the day of testing. Because it is unethical to use healthy children (for whom impedance-pH is not clinically indicated) to generate true normal values, we are forced to consider reference values derived from symptomatic children with normal impedance-pH studies. Finally, analyses of impedance-pH tracings were not blinded to patient genotype. Other studies involving larger samples sizes are needed to confirm the validity and subsequent utility of acid neutralization reference values. Additional studies involving larger samples sizes and wider varieties of genotypes are needed to fully assess the potential impact of genotype on the efficiency of acid neutralization during chemical clearance.
In summary, the data indicate that while children with CF are more likely to have abnormal acid neutralization during chemical clearance compared to children without CF, not all children with CF have acid neutralization during chemical clearance that is outside the physiological range. It is possible that particular CF transmembrane conductance regulator (CFTR) genotypes, in combination with non-CFTRgenetic modifiers and environmental factors, influence acid neutralization efficiency in children with CF [2627]. It is possible that different CFTR genotypes may influence the efficiency of acid neutralization by reducing the efficiency of esophageal motility, by reducing the volume or changing the composition of the saliva, or possibly by increasing gastric acidity. Further investigation involving larger sample sizes are needed to address these questions.
References
1. Simrén M, Silny J, Holloway R, Tack J, Janssens J, Sifrim D. Relevance of ineffective oesophageal motility during oesophageal acid clearance. Gut. 2003; 52:784–790.

2. Helm JF, Dodds WJ, Pelc LR, Palmer DW, Hogan WJ, Teeter BC. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med. 1984; 310:284–288.

3. Boyd DD, Carney CN, Powell DW. Neurohumoral control of esophageal epithelial electrolyte transport. Am J Physiol. 1980; 239:G5–G11.

4. Hamilton BH, Orlando RC. In vivo alkaline secretion by mammalian esophagus. Gastroenterology. 1989; 97:640–648.

5. Meyers RL, Orlando RC. In vivo bicarbonate secretion by human esophagus. Gastroenterology. 1992; 103:1174–1178.

6. Orlando RC. Esophageal mucosal defense mechanisms. Part 1 Oral cavity, pharynx, and esophagus. GI Motil Online. 2006; DOI: 10.1038/gimo15.
7. Abdulnour-Nakhoul S, Nakhoul NL, Orlando RC. Lumen-to-surface pH gradients in opossum and rabbit esophagi: role of submucosal glands. Am J Physiol Gastrointest Liver Physiol. 2000; 278:G113–G120.

8. Abdulnour-Nakhoul S, Nakhoul HN, Kalliny MI, Gyftopoulos A, Rabon E, Doetjes R, et al. Ion transport mechanisms linked to bicarbonate secretion in the esophageal submucosal glands. Am J Physiol Regul Integr Comp Physiol. 2011; 301:R83–R96.

9. Sivalingam M, Sitaram S, Hasenstab KA, Wei L, Woodley FW, Jadcherla SR. Effects of esophageal acidification on troublesome symptoms: an approach to characterize true acid GERD in dysphagic neonates. Dysphagia. 2017; 32:509–519.

10. Frazzoni M, Manta R, Mirante VG, Conigliaro R, Frazzoni L, Melotti G. Esophageal chemical clearance is impaired in gastro-esophageal reflux disease--a 24-h impedance-pH monitoring assessment. Neurogastroenterol Motil. 2013; 25:399–406.
11. Vaezi MF, Singh S, Richter JE. Role of acid and duodenogastric reflux in esophageal injury: a review of animal and human studies. Gastroenterology. 1995; 108:1897–1907.

12. Tuttle SG, Rufin F, Bettarello A. The physiology of heartburn. Ann Intern Med. 1961; 55:292–300.

13. Pauwels A, Blondeau K, Mertens V, Farre R, Verbeke K, Dupont LJ, et al. Gastric emptying and different types of reflux in adult patients with cystic fibrosis. Aliment Pharmacol Ther. 2011; 34:799–807.

14. Pauwels A, Decraene A, Blondeau K, Mertens V, Farre R, Proesmans M, et al. Bile acids in sputum and increased airway inflammation in patients with cystic fibrosis. Chest. 2012; 141:1568–1574.

15. Woodley FW, Machado RS, Hayes D Jr, Di Lorenzo C, Kaul A, Skaggs B, et al. Children with cystic fibrosis have prolonged chemical clearance of acid reflux compared to symptomatic children without cystic fibrosis. Dig Dis Sci. 2014; 59:623–630.

16. Woodley FW, Machado R, Di Lorenzo C, Mousa H. Chemical clearance in infants and children with acid reflux in the physiologic range. J Pediatr Gastroenterol Nutr. 2015; 60:783–786.

17. Pauwels A, Blondeau K, Dupont LJ, Sifrim D. Mechanisms of increased gastroesophageal reflux in patients with cystic fibrosis. Am J Gastroenterol. 2012; 107:1346–1353.

18. Navarro J, Rainisio M, Harms HK, Hodson ME, Koch C, Mastella G, et al. Factors associated with poor pulmonary function: cross-sectional analysis of data from the ERCF. Eur Respir J. 2001; 18:298–305.

19. Dodds WJ, Dent J, Hogan WJ, Helm JF, Hauser R, Patel GK, et al. Mechanisms of gastroesophageal reflux in patients with reflux esophagitis. N Engl J Med. 1982; 307:1547–1552.

20. Richter J. Do we know the cause of reflux disease? Eur J Gastroenterol Hepatol. 1999; 11:Suppl 1. S3–S9.

21. Orlando RC. Overview of the mechanisms of gastroesophageal reflux. Am J Med. 2001; 111:Suppl 8A. 174S–177S.

22. Maclean JE, Solomon M, Corey M, Selvadurai H. Cystic fibrosis newborn screening does not delay the identification of cystic fibrosis in children with negative results. J Cyst Fibros. 2011; 10:333–337.

23. Martinucci I, de Bortoli N, Savarino E, Piaggi P, Bellini M, Antonelli A, et al. Esophageal baseline impedance levels in patients with pathophysiological characteristics of functional heartburn. Neurogastroenterol Motil. 2014; 26:546–555.

24. Woodley FW, Fernandez S, Mousa H. Diurnal variation in the chemical clearance of acid gastroesophageal reflux in infants. Clin Gastroenterol Hepatol. 2007; 5:37–43.

25. Frazzoni M, Savarino E, de Bortoli N, Martinucci I, Furnari M, Frazzoni L, et al. Analyses of the post-reflux swallow-induced peristaltic wave index and nocturnal baseline impedance parameters increase the diagnostic yield of impedance-pH monitoring of patients with reflux disease. Clin Gastroenterol Hepatol. 2016; 14:40–46.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download