Abstract
Purpose
Undernutrition during hospitalization increases the risk of nosocomial infection and lengthens the disease courses. The aim of this study was to evaluate the risk factors of weight loss during hospitalization in children.
Methods
All the patients who were admitted in general wards between April and May 2014 were enrolled. Patients aged >18 years and discharged within 2 days were excluded. Weight loss during hospitalization was defined as a decrease in body weight of >2% in 8 hospital days or on the day of discharge. Patients who lost body weight during hospitalization were compared with patients who maintained their body weights. Significant parameters were evaluated by using the multivariate logistic regression analysis.
Results
We enrolled 602 patients, of whom 149 (24.8%) lost >2% of their body weight. Complaint of pain (p=0.004), admission to the surgical department (p=0.001), undergoing surgery (p=0.044), undergoing abdominal surgery (p=0.034), and nil per os (NPO) durations (p=0.003) were related to weight loss during hospitalization. The patients who had high weight-for-age tended to lose more body weight (p=0.001). Admission to the surgical department (odds ratio [OR], 1.668; 95% confidence interval [CI], 1.054-2.637; p=0.029) and long NPO durations (OR, 1.496; 95% CI, 1.102-2.031; p=0.010) were independent risk factors of weight loss during hospitalization. The patients with high weight-for-age tended to lose more weight during hospitalization (OR, 1.188; 95% CI, 1.029-1.371; p=0.019).
Hospitalized children can easily lose body weight, unless special consideration is given to this issue. Acute illness usually leads to increasing energy consumption while interfering with the child’s appetite and energy intake. Undernutrition during hospitalization interferes with recovery. Delayed recovery provokes comorbidities such as nosocomial infection [1], prolongs hospital stay [23], and increases social medical costs. Compared with that in adults, hospital undernutrition in children can further lead to poor growth and reduced educational and social achievements; additionally, it can possibly have implications on health and performance during adulthood [4]. Even if previously healthy, children admitted to the hospital for specific medical problems are still at risk of body weight loss during hospitalization to prevent undernutrition. Nevertheless, nutrition can be easily disregarded because of acute medical problems.
In recent studies, the prevalence of undernutrition in hospitalized children has varied according to socioeconomic status and medical environment, ranging from 6.1% to 37% [56789]. However, studies related to this issue are still lacking, and no study has been conducted about the nutritional changes in children during hospitalization in Korea.
We conducted this study to assess the prevalence and risk factors of body weight loss in pediatric patients during hospitalization in a Korean level III children’s hospital.
When we expected the prevalence of weight loss during hospitalization to be 30%, at least 138 and 227 patients were needed for an effective sample size of 80% and 90% power, respectively, with 5% significance level, using a two-sided test in the power analysis. We collected the data of all the pediatric patients aged 1 month to 18 years who were admitted in the general wards of the Pusan National University Children’s Hospital between April and May 2014, according to the estimated patient number. This study was performed after review by the institutional review board of Pusan National University Yangsan Hospital (IRB no. I-2014-447).
During the study period, all the patients were enrolled except those who were discharged within 48 hours and those admitted in the psychiatric closed ward and intensive care units. If the patient was readmitted within the study period, the readmission record was excluded. Patients whose weight data could not be used as a nutritional status, such as those with edema or hypoalbuminemia (e.g., nephrotic syndrome, protein losing enteropathy, and congestive heart disease), were excluded. Those with incomplete medical records were also excluded.
This study was performed by reviewing the medical records of the patients retrospectively. At admission, age, sex, body weight, height, presence of low appetite (<50% as usual), presence of pain (absence/presence), gastrointestinal symptoms, underlying chronic gastrointestinal disease, department of admission (medical and surgical department), and laboratory data (total lymphocyte count and albumin) were investigated. Body weight with light clothes as much as possible was checked early in the morning, before breakfast. Pain data were obtained from the admission medical record of age-appropriate pain scales as follows: Wong-Baker scale for older children, FLACC (face, legs, activity, cry, consolability) behavioral scale for toddlers, and infant scale for infants. We set the end point on the eighth hospital day (the first week of hospitalization); and if the patient was discharged within 7 days, the discharge day was regarded as the end point. Body weight, duration of nothing by mouth (nil per os, NPO), and operation records were investigated at the study end point. If the patient was initially dehydrated, body weight after recovering from dehydration was considered as the baseline body weight. The Z scores of weight-for-age, height-for-age, and weight-for-height were calculated by using the measured body weights and lengths/heights. The L-M-S methods of the 2007 Korean Children and Adolescents Growth Standards were used for calculating the Z score.
Weight loss during hospitalization was defined as a body weight loss of >2% at the study end point compared with the admission body weight. We investigated the prevalence of patients who lost body weight during hospitalization. We analyzed the risk factors of weight loss during hospitalization by using a univariate analysis for undernutrition (independent t-test, χ2 test or Fischer exact test). Further multivariate logistic regression analysis was performed by using the significant data in the univariate analysis. All statistical data were further analyzed according to 4 different age groups (<1, 1-6, 7-11, and 12-18 years).
IBM SPSS Statistics ver. 21.1 (IBM Co., Armonk, NY, USA) was used, and a p-value of <0.05 was considered significant.
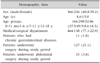
During a period of 2 months, 1,063 patients were admitted in general wards. According to the inclusion and exclusion criteria, 602 patients (366 boys and 236 girls) were included in this study (Fig. 1). The mean age at admission was 4.6±5.0 years (range, 0.1-17.8 years), and the age distribution is described in Table 1. Of the patients, 464 (77.1%) were admitted in the medical department, whereas 138 (22.9%) were admitted in the surgical department (Table 1).
The mean weight-for-age Z score was –0.23±1.63 in all the patients, and 12.5% of the patients were under 5 percentiles (Z score, <–1.645). The mean height-for-age and weight-for-height Z scores were 0.17±1.57 and –0.31±1.43, respectively.
Body weight loss of >2% was observed in 149 patients (24.8%) during the hospitalization; >5%, in 38 patients (6.3%) during the first week of hospitalization; and >10%, in 3 patients (0.5%) during the first week of hospitalization.
Pain complaint (p=0.004), admission in the surgical department (p=0.001), undergoing surgery (p=0.044), undergoing abdominal surgery (p=0.034), and NPO duration (p=0.003) were risk factors of weight loss during hospitalization in the univariate analysis. The patients who had lower weight-for-age and weight-for-height tended to lose less body weight (p=0.001; Table 2).
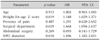
Multivariate logistic regression analysis was performed, including variables of age, weight-for-age, presence of pain, admission in the surgical department, abdominal surgery, and NPO duration. Admission in the surgical department (odds ratio [OR], 1.668; 95% confidence interval [CI], 1.054-2.637; p=0.029), weight-for-age (OR, 1.188; 95% CI, 1.029-1.371; p=0.019), and NPO durations (OR, 1.496; 95% CI, 1.102-2.031; p=0.010) were independent risk factors of weight loss during hospitalization (Table 3).
In the infant group (age <1 year, n=166), high weight-for-age (OR, 1.446, 95% CI, 1.005-2.079, p=0.047) and long NPO duration (OR, 7.327; 95% CI, 1.505-35.677; p=0.014) were risk factors of weight loss during hospitalization. Infants who underwent abdominal surgery (OR, 8.432×10–5; 95% CI, 0.000-0.941; p=0.049) had less risk of weight loss statistically. Only 2 infants underwent abdominal surgery. In the toddler group (age between 1 and 6 years, n=298) and school-aged group (age between 7 and 11 years, n=52), no specific factors were related to weight loss during hospitalization However, in the adolescent group (age between 12 and 18 years, n=86), age (OR, 1.622; 95% CI, 1.064-2.472; p=0.024) was a risk factor of weight loss during hospitalization in the multivariate logistic regression analysis.
All Korean hospitalized patients should be screened for their nutritional status and risk of undernutrition according to the recommendation of the Korean Ministry of Health and Welfare in order to prevent hospital undernutrition. If the patient is currently undernourished or at risk of undernutrition, the hospital should pay more attention to the nutrition of the indexed patient. Anthropometric parameters such as weight and height are effective to detect current undernutrition in children. Several nutritional screening tools have been published [101112131415]. However, currently, in Korea, most of the medical centers use nutritional screening tools for adults equally for children.
Several pediatric nutrition screening tools are available for hospitalized children. Sermet-Gaudelus et al. [10] introduced the Pediatric nutritional risk score, which regarded undernutrition as a body weight loss of >2%. They suggested contents of food intake (score 1), difficulty retaining food (score of 1), pain (score of 1), ability to eat (score of 1), medication condition (score of 1-3), and score of >3 as high-risk factors of undernutrition. Secker and Jeejeebhoy [11] suggested a subjective global nutritional assessment for surgical children, which included weight history, parental height, dietary intake, gastrointestinal symptoms, functional capacity, physical examination, and underlying condition. Gerasimidis et al. [12] recommended the Paediatric Yorkhill Undernutrition Score, which covered body mass index, recent weight loss, nutritional intake, and medical condition. Hulst et al. [13] suggested STRONGkids by using four items of subjective assessment, high-risk disease, nutritional intake and weight loss. McCarthy et al. [14] suggested the Screening Tool for the Assessment of Undernutrition in Pediatrics (STAMP), which used clinical diagnosis, nutritional intake, and anthropometry. White et al. [15] recently suggested a simple pediatric nutrition screening tool (PNST) that uses current changes in appetite and body weight as assessments parameters. All the tools were built in different medical, surgical conditions, and social and health-care systems in variable countries. Several validation studies, meta-analysis, and application studies have been conducted [7916171819]. All these screening tools used similar and somewhat different parameters for screening undernutrition risk, and the study population for each study was also variable. To screen nutritional risk in each medical institute, each should have to recognize their own risk factors of developing undernutrition.
In the present study, admission in the surgical department and prolonged NPO durations were major independent risk factors of weight loss during hospitalization in our children’s hospital. Long NPO duration was a dominant risk factor especially in the infant group, with an OR of 7.327. As infants have insufficient reserve to withstand starvation and are susceptible to the effect of starvation [20], parenteral nutrition should be given at least a few days of fasting. However, this result indicates that our current practice might be insufficient to prevent from weight loss during hospitalization in infants. Older children and adolescents tend to be more tolerant of prolonged inadequate nutrition up to 7 days [20]. Seven days is a short period for estimating actual nutritional deficit. However, clinicians should be aware of prolonged NPO and should apply adequate enteral or parenteral nutrition in appropriate timing. In the adolescent group, age was a risk factor of weight loss during hospitalization. It could be influenced by many factors such as differences in diseases or treatments, types of meals and emotional stresses. The number of patients in each subgroup was not enough to attain a strong statistical power in the subgroup study. For gathering age-specific information, further study is needed.
Several classic nutritional biomarkers of undernutrition have been used, such as albumin, prealbumin, retinoic binding protein, and ferritin levels, and total lymphocyte count [21]. Patients with poor nutritional biomarkers can be considered as having undernutrition. However, these markers were not indicative of ongoing undernutrition during hospitalization. Total lymphocyte count and albumin level were not related to weight loss during hospitalization in the present study. Like in our study, the current consensus is that laboratory parameters are not suitable as screening modalities [22].
Several limitations should be considered in the present study. First, we considered losing 2% of the previous body weight as a marker of undernutrition. We excluded edema and dehydration. For patients who are very light, 2% can be narrow in range. Parents who have patients with low body weights are usually more interested in the body weight changes of their children. Therefore, misperception in determining body weight as an index of undernutrition is possible. However, body weight is a useful marker of acute malnutrition, and a study similar to ours was conducted [10]. Second, we identified the risk factors of weight loss during hospitalization to further establish a screening tool that can be easily used at the point of admission. However, NPO duration is difficult to predict at the time of admission. Third, at the time of the present study, in our institute, the nutritional support team acted passively. Some interventions were given to patients who lost 5% of their body weights.
Despite these several limitations, the present data might represent our current situations. Nutritional status is changing continuously. Studies such as this should be performed regularly, and a further validation study should be conducted as a follow-up study.
In conclusion, 24.8% of children lose >2% of their body weights during the first week of hospitalization. Admission in a surgical department and prolonged NPO duration were identified as independent risk factors of weight loss during hospitalization. Patients with such risk factors should receive more attention regarding their nutritional status during hospitalization in order to prevent hospital undernutrition.
Figures and Tables
 | Fig. 1Schematic diagram of the patient enrollment according to the inclusion and exclusion criteria. DKA: diabetes ketoacidosis, NS: nephrotic syndrome. |
ACKNOWLEDGEMENTS
This study was supported the Research institute for Convergence of biomedical science and technology (30-2014-007), Pusan National University Yangsan Hospital. The statistical analysis was supported by Research and Statistical Support, Research Institute of Convergence for Biomedical Science and Technology, Pusan National University Yangsan Hospital.
References
1. Schneider SM, Veyres P, Pivot X, Soummer AM, Jambou P, Filippi J, et al. Malnutrition is an independent factor associated with nosocomial infections. Br J Nutr. 2004; 92:105–111.

2. Kac G, Camacho-Dias P, Silva-Coutinho D, Silveira-Lopes R, Marins VV, Pinheiro AB. Length of stay is associated with incidence of in-hospital malnutrition in a group of low-income Brazilian children. Salud Publica Mex. 2000; 42:407–412.

3. de Amorim AC, Costa MD, Nunes FL, da Silva Mda G, de Souza Leão C, Gadelha PC. Nutritional status and perioperative fasting time versus complications and hospital stay of surgical patients. Nutr Hosp. 2015; 32:878–887.
4. Hoddinott J, Behrman JR, Maluccio JA, Melgar P, Quisumbing AR, Ramirez-Zea M, et al. Adult consequences of growth failure in early childhood. Am J Clin Nutr. 2013; 98:1170–1178.

5. Lee DG, Rho YI, Moon KR. Assessment of nutritional status in hospitalized pediatric patients. Korean J Pediatr Gastroenterol Nutr. 2001; 4:83–91.

6. Joosten KF, Hulst JM. Prevalence of malnutrition in pediatric hospital patients. Curr Opin Pediatr. 2008; 20:590–596.

7. Mărginean O, Pitea AM, Voidăzan S, Mărginean C. Prevalence and assessment of malnutrition risk among hospitalized children in Romania. J Health Popul Nutr. 2014; 32:97–102.
8. Márquez Costa MV, Alberici Pastore C. Nutritional screening tool versus anthropometric assessment in hospitalized children: which method is better associated to clinical outcomes? Arch Latinoam Nutr. 2015; 65:12–20.
9. Chourdakis M, Hecht C, Gerasimidis K, Joosten KF, Karagiozoglou-Lampoudi T, Koetse HA, et al. Malnutrition risk in hospitalized children: use of 3 screening tools in a large European population. Am J Clin Nutr. 2016; 103:1301–1310.

10. Sermet-Gaudelus I, Poisson-Salomon AS, Colomb V, Brusset MC, Mosser F, Berrier F, et al. Simple pediatric nutritional risk score to identify children at risk of malnutrition. Am J Clin Nutr. 2000; 72:64–70.

11. Secker DJ, Jeejeebhoy KN. Subjective global nutritional assessment for children. Am J Clin Nutr. 2007; 85:1083–1089.

12. Gerasimidis K, Keane O, Macleod I, Flynn DM, Wright CM. A four-stage evaluation of the Paediatric Yorkhill Malnutrition Score in a tertiary paediatric hospital and a district general hospital. Br J Nutr. 2010; 104:751–756.

13. Hulst JM, Zwart H, Hop WC, Joosten KF. Dutch national survey to test the STRONGkids nutritional risk screening tool in hospitalized children. Clin Nutr. 2010; 29:106–111.

14. McCarthy H, Dixon M, Crabtree I, Eaton-Evans MJ, McNulty H. The development and evaluation of the Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP©) for use by healthcare staff. J Hum Nutr Diet. 2012; 25:311–318.

15. White M, Lawson K, Ramsey R, Dennis N, Hutchinson Z, Soh XY, et al. Simple nutrition screening tool for pediatric inpatients. JPEN J Parenter Enteral Nutr. 2016; 40:392–398.

16. Huysentruyt K, Alliet P, Muyshont L, Rossignol R, Devreker T, Bontems P, et al. The STRONG(kids) nutritional screening tool in hospitalized children: a validation study. Nutrition. 2013; 29:1356–1361.

17. Joosten KF, Hulst JM. Nutritional screening tools for hospitalized children: methodological considerations. Clin Nutr. 2014; 33:1–5.

18. Wonoputri N, Djais JT, Rosalina I. Validity of nutritional screening tools for hospitalized children. J Nutr Metab. 2014; 2014:143649.

19. Huysentruyt K, Devreker T, Dejonckheere J, De Schepper J, Vandenplas Y, Cools F. Accuracy of nutritional screening tools in assessing the risk of undernutrition in hospitalized children. J Pediatr Gastroenterol Nutr. 2015; 61:159–166.

20. Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R. 1. Guidelines on paediatric parenteral nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), Supported by the European Society of Paediatric Research (ESPR). J Pediatr Gastroenterol Nutr. 2005; 41:Suppl 2. S1–S87.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download