Abstract
Purpose
To evaluate the correlation between colon transit time (CTT) test value and initial maintenance dose of polyethylene glycol (PEG) 4000 or lactulose.
Methods
Of 415 children with chronic functional constipation, 190 were enrolled based on exclusion criteria using the CTT test, defecation diary, and clinical chart. The CTT test was performed with prior disimpaction. The laxative dose for maintenance was determined on the basis of the defecation diary and clinical chart. The Shapiro-Wilk test and Pearson's and Spearman's correlations were used for statistical analysis.
Results
The overall group median value and interquartile range of the CTT test was 43.8 (31.8) hours. The average PEG 4000 dose for maintenance in the overall group was 0.68±0.18 g/kg/d; according to age, the dose was 0.73±0.16 g/kg/d (<8 years), 0.53±0.12 g/kg/d (8 to <12 years), and 0.36±0.05 g/kg/d (12 to 15 years). The dose of lactulose was 1.99±0.43 mL/kg/d (<8 years) or 1.26±0.25 mL/kg/d (8 to <12 years). There was no significant correlation between CTT test value and initial dose of laxative, irrespective of the subgroup (encopresis, abnormal CTT test subtype) for either laxative. Even in the largest group (overall, n=109, younger than 8 years and on PEG 4000), the correlation was weak (Pearson's correlation coefficient [R]=0.268, p=0.005). Within the abnormal transit group, subgroup (n=73, younger than 8 years and on PEG 4000) correlation was weak (R=0.267, p=0.022).
Constipation is one of the most common symptoms in children and is responsible for 7% of pediatric clinic visit. Up to 25% of children who visit pediatric gastroenterology specialist have constipation [123]. Constipation in children can become chronic in up to one-third of patients and persist into the adult [4]. So, it is important to provide appropriate treatment in pediatric patients. Initiating appropriate treatment starts with evaluating the status of the patients correctly.
Several laxatives with different mechanisms are available in pediatrics, and osmotic laxatives are most frequently prescribed. Studies on the dose of laxative needed for disimpaction or maintenance were generally performed based on body weight or age [56789]. However, according to the authors' experience, weight- and age-matching do not describe equivalent clinical status of constipation. That is, same-aged children do not use the same drug or same amount. In clinical practice, we usually stratifies the patients according to the clinical status (How often the patient has bowel movement?; How long has the patient been constipated?; Dose the patient soil feces? etc.) and results of several diagnostic tests (the hardness or size of rectal mass on digital rectal examination, fecal amount on plain abdominal film, etc.). However, this process doesn't seem to be satisfactory.
A colon transit time (CTT) test using radiopaque markers is regarded as the gold standard for evaluating colon transit function in both adults and children [1011121314]. Functional constipation can be classified into normal colon transit type, outlet obstruction type, and slow transit type on the basis of CTT [111314]. This distinction may be helpful for establishing an accurate diagnosis and effective treatment in adults [1314]. Despite limited studies, CTT test has proved its value for evaluating chronic functional constipation in children. Prolonged CTT test value implies worse clinical status, and constipation accompanying encopresis shows a prolonged CTT test value compared to that without encopresis [111516].
Authors think that CTT test can reflect the clinical status of constipation and the results of CTT test can be applied to treatment. In the present study, we evaluated the correlation between CTT test value and initial maintenance dose of polyethylene glycol 4000 or lactulose, based on highly refined data from a defecation diary, medical records, CTT test results with prior disimpaction and proper statistical analysis.
A total of 415 children who met Rome III criteria for constipation [1718] were enrolled at Konkuk University Medical Center in Seoul between January 2005 and March 2015. Of these, 224 children were excluded, and 190 were finally enrolled in this study. Some of the children overlapped during screening. Exclusion criteria were as follows: (1) the sum of retained radiopaque markers on the 4th and 7th day was the same or less than 10 on the CTT test (n=85); (2) during the CTT test, there was acute illness, or in cases where the defecation pattern during CTT test was better than that of the on medication period on the basis of the defecation diary (n=155); (3) the child was on more than 2 medications for constipation (n=10); (4) underlying disease (n=9), including failure of the puborectalis muscle to relax (n=4), imperforate anus (n=1), intracranial hemorrhage (n=1), extreme obesity (n=1), or epilepsy (n=2); (5) older than 16 year (n=8); and (6) child on Mirax (PEG 3350; Keonil Pharmacy Co., Seoul, Korea) (n=4).
CTT test was performed after removing fecal impaction within 1-2 months after the initial diagnosis. Before or during the tests, participants maintained a normal diet. From the day before the tests, medications (antibiotics, antihistamines, antipyretics) and foods (persimmon, banana) known to affect gastrointestinal motility were avoided. If a child had acute illness (upper respiratory infection, acute gastroenteritis, etc.) during the test, the study was postponed. CTT test was performed according to a method by Metcalf et al. [19]. A Kolomark (MI Tech, Seoul, Korea) capsule containing 20 radiopaque markers was taken at the same time each day for 3 consecutive days. A plain abdominal radiograph was taken on days 4 and 7, and the number of remaining markers was counted. The CTT test value was calculated according to the following formula: CTT test value=sum of remaining markers on film on days 4 and 7×1.2. The CTT test vaslue was classified as normal transit type, ≤35 (42 hours), or abnormal transit type, ≥36 (43 hours) [11]. An abnormal type was subdivided into an outlet obstruction subtype and a slow transit subtype.
The initial maintenance dose was defined as the amount of laxative that resulted in relief of the chief complaint and a comfortable bowel movement (soft or loose stool) more than 5 days per week for more than 2 months without change in dose, on the basis of a defecation diary that described frequency of bowel movements and consistency of stool, as reported by the patient or guardian. To determine the dose of laxative by weight, subjects were divided in three groups according to age: less than 8 years old (before elementary school), 8 to less than 12 years old (elementary school, before growth spurting), and 12 to 15 years old (growth spurting).
For statistical analysis, IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA) was used.
For statistical correlation between CTT test value and initial maintenance dose of PEG 4000, Pearson's and Spearman's correlations were used according to the result of the Shapiro-Wilk test. A p-value less than 0.05 was considered statistically significant.
The CTT test results were as follows. Overall, the median value of CTT test was 43.8 hours, with interquartile range (IQR), 31.8 hours. The median value and IQR of CTT test was 54 (37.5) hours in the encopresis group, and 40.2 (27.9) hours (p<0.001) in the non-encopresis group. In the non-encopresis group, the values were 26.4 (9.6) hours with normal transit, 62.4 (15.6) hours with outlet obstruction, and 54.6 (21.0) hours with slow transit. In the encopresis group, the values were 32.4 (9.9) hours with normal transit, 67.8 (34.8) hours with outlet obstruction, and 59.4 (62.7) hours with slow transit.
Of 190 children, 86 were male. The median age and IQR was 5 (4) years (3-15 years); 137 (72.3%) children were on PEG 4000 (Forlax; Beaufour Ipsen Pharm., Paris, France) and 53 (27.7%) were on lactulose (Duphalac syrup; JW Pharmaceutical, Seoul, Korea). The mean lactulose dose in children younger than 8 years (n=42) was 1.99±0.43 mL/kg/d and the dose in children 8 to <12 years (n=11) was 1.26±0.25 mL/kg/d. The mean dose of PEG 4000 in children younger than 8 years (n=109) was 0.73±0.16 g/kg/d, that in children 8 to <12 years (n=23) was 0.53±0.12 g/kg/d, and that in children 12 to 15 years (n=5) was 0.36±0.05 g/kg/d (Table 1).
In the overall group, Pearson's correlation coefficient (R) between CTT test value and PEG 4000 was 0.268 (p=0.005) in children younger than 8 years. In other groups, the correlation was not statistically significant (Table 2).
In the non-encopresis group (n=154), 63 were male, and the median age and IQR was 5 (4) years; 102 (66.2%) were on PEG 4000 and 52 (33.8%) were on lactulose. In the encopresis group (n=36), 22 were male, and the median age and IQR was 5 (2) year; 35 (97.2%) were on PEG 4000 and 1 (2.8%) was on lactulose.
In the non-encopresis group, the mean dose of lactulose in children younger than 8 years (n=41) was 2.00±0.43 mL/kg/d and that in children 8 to <12 years (n=11) was 1.26±0.25 mL/kg/d. The mean dose of PEG 4000 in children younger than 8 years (n=81) was 0.71±0.15 g/kg/d, that in children 8 to <12 years (n=16) was 0.52±0.12 g/kg/d, and that in children 12 to 15 years (n=5) was 0.36±0.05 g/kg/d. In the encopresis group, the mean dose of PEG 4000 in children younger than 8 years (n=28) was 0.78±0.17 g/kg/d and that in children 8 to <12 years (n=7) was 0.55±0.13 g/kg/d (Table 3).
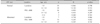
In every group, the correlation was not statistically significant (Table 4).
In the normal transit group (n=92), 39 were male, and the median age and IQR was 5 (2) years; 47 (51.1%) were on PEG 4000 and 45 (48.9%) were on lactulose. In the abnormal transit group (n=98), 46 were male, and the median age and IQR was 5 (3) years; 90 (91.8%) were on PEG 4000 and 8 (8.2%) were on lactulose.
In the normal transit group, the mean dose of lactulose in children younger than 8 years (n=35) was 2.01±0.42 mL/kg/d and that in children 8 to <12 years (n=10) was 1.27±0.25 mL/kg/d. The mean dose of PEG 4000 in children younger than 8 years (n=36) was 0.69±0.15 g/kg/d, that in children 8 to <12 years (n=8) was 0.52±0.08 g/kg/d, and that in children 12 to 15 years (n=3) was 0.34±0.04 g/kg/d.
In the abnormal transit group, the mean dose of lactulose in children younger than 8 years (n=7) was 1.89±0.48 mL/kg/d and that in children 8 to <12 years (n=1) was 1.21 mL/kg/d. The mean dose of PEG 4000 in children younger than 8 years (n=73) was 0.75±0.16 g/kg/d, that in children 8 to <12 years (n=15) was 0.54±0.14 g/kg/d, and that in children 12 to 15 years (n=2) was 0.40±0.04 g/kg/d (Table 5).
In the abnormal transit group, Pearson's correlation coefficient (R) for the correlation between the CTT test value and PEG 4000 was 0.267 (p=0.022) in children younger than 8 years. In other groups, the correlation was not statistically significant, even in subtype groups (outlet obstruction type, slow transit type) (Table 6).
Treatment of chronic functional constipation generally consists of 3 phases: disimpaction, maintenance, and weaning. In the maintenance phase, laxatives are the main modality of treatment, in addition to dietary instruction and toilet training. PEG 3350/4000, lactulose, sorbitol, magnesium hydroxide, mineral oil, and fiber are usually prescribed in pediatrics [5]. In the present study, we used lactulose and PEG 4000 as laxatives, and defined the initial dose for maintenance on the basis of a defecation diary that described the frequency of bowel movements and consistency of stool, as reported by the patient or guardian.
Studies on the dose of laxative were usually performed based on body weight or age. With respect to PEG 3350/4000, the usual dose for a child was 0.2 g/kg/d to 1 g/kg/d [56789]. For disimpaction, the average safe and effective dose of PEG 4000 was 0.93±0.28 g/kg/d (0.4-2.0 g/kg/d, maximum: 30 g/d) in children with chronic functional constipation. In this study, the dose was also based on age [8]. In one study that enrolled children with and without - encopresis, the average effective long-term dose of PEG 3350 was 0.7 g/kg/d. However, this study did not discuss disimpaction [6]. For maintenance, one European study stratified patients according to age, and a daily dose of PEG 4000 of around 0.50 g/d/kg in children aged 6 months to 15 y was effective in more than 90% of constipated children and 60% of those with fecal soiling [7]. In a Korean study, the average dose of PEG 4000 was 0.55±0.16 g/kg/d; according to age, the dose was 0.60±0.15 g/kg/d (3-5 years), 0.57±0.16 g/kg/d (6-8 years), and 0.44±0.14 g/kg/d (9-13 years) [9]. In the present study, the average dose of PEG 4000 for maintenance in the overall group was 0.68±0.18 g/kg/d; according to age, the dose was 0.73 g/kg/d (<8 years), 0.53 g/kg/d (8 to <12 years), and 0.36 g/kg/d (12 to 15 years). This result was similar to previous studies, with a tendency toward decreasing dose as age increased.
The CTT test with radiopaque markers is simple, and has been used widely for assessing colon transit function in both adults and children. It can measure total CTT and can determine segmental transit function. This can indicate the subtype of functional constipation [13]. In pediatrics, no study on subtype has been reported to date. However, in adults, diagnostic and therapeutic strategy can be directed by subtype. With a normal transit type, a stool softener or fiber can be tried; with an outlet obstruction type, biofeedback can be applied; with a slow transit type, prokinetics, stimulants, or electronic stimulation can be applied [14]. In pediatrics, studies on normal and abnormal transit value with adequate statistical analysis were recently published [1112]. In some studies, prolonged CTT test value implies poor clinical status, and children with encopresis have prolonged CTT test values compared to those without encopresis [11151620]. In the present study, the CTT test was performed with disimpaction. Appropriate data were selected based on a defecation diary and clinical chart with proper statistical analysis. This process helped refine the present study.
Based on adequate data for the dose of laxatives and the highly refined CTT test value, the authors in the present study evaluated the correlation between CTT test value and initial maintenance dose of laxatives. To our knowledge, this is the first such report. The results showed no significant correlation, irrespective of the subgroup (encopresis, abnormal CTT test subtype). Even in the largest group (overall, n=109, younger than 8 year and on PEG 4000), which showed normal distribution, the correlation was weak (Pearson's correlation coefficient [R]=0.268, p=0.005). Within the abnormal transit group, subgroup (n=73, younger than 8 years and on PEG 4000) correlation was weak (R=0.267, p=0.022). This implies that there is not a linear correlation between CTT test value and initial dose of laxatives for maintenance phase, and CTT test value cannot predict the initial maintenance dose of laxatives, PEG 4000 or lactulose. However, authors think that this disappointing result does not exclude the need to study with CTT test in children with constipation. Authors think that CTT test can reflect the clinical status of constipation, and similar CTT test values or the same CTT test subtype can be used for children with chronic constipation. This conception warrants further studies.
A limitation of this study is that even though 190 children were enrolled, the numbers in subgroups were small. This may have an effect on statistical analysis. Another limitation is that in practice, the usual maximum dose of PEG 4000 for maintenance is 20 g/d in most children, but some children were administered 30 g/d. This limitation may have an effect on the linear relationship between body weight and dose of laxative.
Figures and Tables
Table 2
Correlation between Colon Transit Time Test Value and Maintenance Dose of Laxatives in the Overall Group
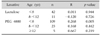
Table 4
Correlation between Colon Transit Time Test Value and Maintenance Dose of Laxatives in Groups according to Encopresis

References
2. Levine MD. Children with encopresis: a descriptive analysis. Pediatrics. 1975; 56:412–416.
3. Youssef NN, Di Lorenzo C. Childhood constipation: evaluation and treatment. J Clin Gastroenterol. 2001; 33:199–205.
4. van Ginkel R, Reitsma JB, Büller HA, van Wijk MP, Taminiau JA, Benninga MA. Childhood constipation: longitudinal follow-up beyond puberty. Gastroenterology. 2003; 125:357–363.

5. Tabbers MM, DiLorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014; 58:258–274.

6. Pashankar DS, Bishop WP, Loening-Baucke V. Long-term efficacy of polyethylene glycol 3350 for the treatment of chronic constipation in children with and without encopresis. Clin Pediatr (Phila). 2003; 42:815–819.

7. Dupont C, Leluyer B, Amar F, Kalach N, Benhamou PH, Mouterde O, et al. A dose determination study of polyethylene glycol 4000 in constipated children: factors influencing the maintenance dose. J Pediatr Gastroenterol Nutr. 2006; 42:178–185.

8. Lee JH, Lee R, Bae SH. Efficacy and safety of electrolytes-free polyethylene glycol (PEG) 4000 for disimpaction in children with chronic functional constipation. Korean J Pediatr. 2008; 51:391–395.

9. Lee SH, Bae SH. Maintenance dose of electrolyte free polyethylene glycol (PEG) 4000 in Korean children with chronic functional constipation. Korean J Pediatr. 2007; 50:1212–1216.

10. Southwell BR, Clarke MC, Sutcliffe J, Hutson JM. Colonic transit studies: normal values for adults and children with comparison of radiological and scintigraphic methods. Pediatr Surg Int. 2009; 25:559–572.

11. Yoo HY, Kim MR, Park HW, Son JS, Bae SH. Colon transit time test in Korean children with chronic functional constipation. Pediatr Gastroenterol Hepatol Nutr. 2016; 19:38–43.

12. Velde SV, Notebaert A, Meersschaut V, Herregods N, Van Winckel M, Van Biervliet S. Colon transit time in healthy children and adolescents. Int J Colorectal Dis. 2013; 28:1721–1724.

13. Kim ER, Rhee PL. How to interpret a functional or motility test - colon transit study. J Neurogastroenterol Motil. 2012; 18:94–99.

14. Lembo AJ, Ullman SP. Constipation. In : Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger and Fordtran's gastrointestinal and liver disease. 9th ed. Philadelphia: Saunders Elsevier Co.;2010. p. 259–284.
15. de Lorijn F, van Wijk MP, Reitsma JB, van Ginkel R, Taminiau JA, Benninga MA. Prognosis of constipation: clinical factors and colonic transit time. Arch Dis Child. 2004; 89:723–727.

16. Benninga MA, Büller HA, Tytgat GN, Akkermans LM, Bossuyt PM, Taminiau JA. Colonic transit time in constipated children: does pediatric slow-transit constipation exist? J Pediatr Gastroenterol Nutr. 1996; 23:241–251.

17. Hyman PE, Milla PJ, Benninga MA, Davidson GP, Fleisher DF, Taminiau J. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology. 2006; 130:1519–1526.

18. Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006; 130:1527–1537.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download