Abstract
Purpose
The management and clinical course in pediatric patients who had ingested foreign body were investigated retrospectively to evaluate the frequency and factor associated with successful removal of fishbone foreign body.
Methods
Based on the medical records of patients younger than 15 years old who visited emergency room because of foreign body ingestion from January 1999 to December 2012, the authors reviewed clinical characteristics including type of ingested foreign bodies, time to visits, managements and complications.
Results
Fishbone (50.1%) was the most common ingested foreign body in children. Among 416 patients with ingested fishbone, 245 (58.9%) were identified and removed using laryngoscope, rigid or flexible endoscope from pharynx or upper esophagus by otolaryngologists and pediatric gastroenterologists. The kind of ingested fish bone in children was diverse. The mean age of identified and removed fishbone group was 7.39 years old, and higher than that of unidentified fishbone group (5.81 years old, p<0.001). Identified and removed fishbone group had shorter time until hospital visit than the unidentified fishbone group (2.03 vs. 6.47 hours, p<0.001). No complication due to ingested fishbone or procedure occurred.
Foreign body ingestion is one of the main problems that causes young children to visit the emergent care unit or hospital frequently. Infants and children tend to understand surrounding objects by tasting and swallowing them [1]. Because infants and young children have limited languages and expressions, and most foreign bodies are naturally excreted through the gastrointestinal (GI) tract, the exact frequency remains unclear [23]. However, the American Poison Control Center reported that population under the age of 19 years who swallowed foreign bodies reportedly reached 125,000 in 2007 alone [4]. The frequency of foreign body ingestion was highest for young children from 6 months after birth up to less than 4 years old; in addition, while most of the foreign bodies were normally excreted through the GI tract and the anus without any complications, less than 10% experienced their retention in the gut [56]. Unlike adults, foreign body ingestion occurs accidently in young children. Hence, in case of sore throat of unknown cause or difficulty in swallowing food or saliva, suspicion of foreign substance in the throat or esophagus should be raised [7].
Hospital visits of pediatric patients due to foreign body intake are common worldwide. Most previous studies on GI foreign materials in children reported that coins represent the largest percentage and food related foreign bodies account for the second highest percentage [8]. With respect to food related foreign materials, major fish consuming countries such as China and Korea show a higher rate of ingested fish bones, as compared to other countries [9]. Fish bones are usually found at the palatine tonsils, tongue base, vallecula and pyriform sinus. They often require an otolaryngological treatment. Endoscopic treatment is recommended for fish bones that get lodged in lower than pharynx and the esophagus, but the frequency of discovery and removal is somewhat low [10]. However, if the fish bone remains lodged in the esophagus, mucosal ulceration or topical inflammatory reactions may cause esophageal stenosis or perforation, and may further develop into deep neck abscess, mediastinitis, lung abscess or aortic fistulae. Therefore, fast and accurate diagnosis and treatment are needed [4]. According to previous Korean studies on foreign bodies in children, the frequency of complications and surgery caused by foreign bodies in the gut have decreased due to shortened time from swallow of foreign bodies up to proper treatment [78]. The development and availability of flexible or rigid upper GI endoscope have led to active medical treatment in pediatric patients, as opposed to waiting for natural emissions.
Recent studies on pediatric foreign body still display a discernible trend of coins [78]. However, we experienced pediatric patients with fish bone foreign body more frequently than coin in this area, surrounded by river and coast. Therefore, we investigated clinical characteristics, kinds of foreign body, and outcomes in pediatric patients with foreign body ingestion, especially fish bone.
Retrospective reviews were conducted on previously healthy pediatric patients aged 15 years and younger, who visited emergency care unit in our hospital for suspected ingestion of foreign body between January 1999 and December 2012. Suspicious foreign body ingestion in the present study was defined as follows: first, patients who were witnessed the sight of ingestion of foreign body by caregiver or parents were included. Second, in absence of witness, ingested foreign body was found incidentally during hospitalization, or foreign body ingestion could be suspected based on the previous history (handling with foreign body, such as toy, coin, paper, and so on) or recent food history (such as, fish or chicken). The patients' sex, age, symptoms, type of ingested foreign body, time spent from accident to hospital visit, and removal were analyzed based on medical records. The methods used to remove foreign body on the medical records were laryngoscope, rigid and flexible GI endoscope. Rigid and flexible endoscopy were conducted by experienced otolaryngologists and pediatric gastroenterologists.
Statistical analyses were conducted using a frequency test and paired t-test with IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). The results of the t-test were considered as statistically significant only when the p-values were below 0.05.
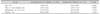
In total, previously healthy 831 patients aged younger and 15 years visited the Gyeongsang National University Hospital for suspected ingestion of foreign body between January 1999 and December 2012. Five hundred and eight patients (61.1%) were males. The mean age of all the patients with foreign body ingestion was 4.99 (±0.49) years old. Two hundred and seven patients (24.9%) were younger than 1 year old, 194 (23.3%) were between 1 and 3 years of age, 125 (15.0%) were between 4 and 5 years of age, 253 (30.4%) were between 6 and 12 years of age, and 52 (6.3%) were between 13 and 15 years of age. The most common ingested foreign body in children was fish bone (416 patients, 50.1%). The second most common foreign body was toy including magnet (135, 16.2%) and the third was coin (112, 13.5%). The others were sharp object including pin, pushpin or staple (39, 4.7%), and button battery (14, 1.7%) (Table 1).
Among 416 patients who visited the hospital due to the ingestion of fish bones, 249 (59.9%) were male. The mean age of the patients was 6.0 (±2.3) years old. Forty-eight patients (11.5%) were younger than 1 year old, 99 (23.8%) were between 1 and 3 years old, 65 (15.6%) were between 4 and 5 years old, and 204 (49.0%) were 6 years old and over. The kind of fish bone was diverse and was not associated with symptoms and outcomes. Croaker bones were 74 (17.8%), mackerel bones were 33 (7.9%), hairtail bones were 22 (5.3%), and others were gizzard shad bone, alaska pollock bone, sea bream bone, and so on. The time from ingestion of fish bone until the hospital visit was less than 2 hours in 287 patients (69.0%), between 2 and 6 hours in 62 patients (15.0%), between 6 and 24 hours in 52 patients (12.5%), and longer than 24 hours in 12 patients (2.9%). All the pediatric patients suspected of fish bone ingestion complained of one or more symptoms, which were foreign body sensation (287 patients, 69.0%), sore throat (58 patients, 13.9%), nausea or vomiting (64 patients, 15.4%), drooling or dysphagia (42 patients, 10.1%), and cough (31 patients, 7.5%) (Table 2). In 239 patients (57.5%), the guardians did not notice the ingestion, and the patients visited the hospital due to the symptoms after eating fish. Fish bone was identified most frequently at pharynx (240, 57.7%), esophagus (6, 1.4%) and stomach (1, 0.2%) in order. Fish bone was identified and removed using oropharyngeal examination, simple x-ray, rigid or flexible endoscopy. Fish-bone was removed successfully in 245 patients (58.9%). Flexible esophagogastroduodenal endoscopic examination was done in 38 patients because of sustained symptoms after failure to remove from oropharynx, and fish bone was removed from lower pharynx or esophagus in 8 patients. In 169 patients (40.6%), fishbone was unidentified after oropharyngeal, radiological, or endoscopic examination. Ingested fish bone in 171 patients was not identified or identified but failed to be removed and the patients were followed up at outpatient clinic (Table 2). No complication due to ingested fish-bone or procedure occurred.
The mean age of the patients with identified and removed fish bone was significantly higher than that of patients with unidentified fish bone (7.39±4.24 vs. 5.81±4.08 years old, t=3.411, p<0.001). The time spent until hospital visit was significantly shorter in identified fish bone group than in unidentified group (2.03±12.61 vs. 6.47±13.12 hours, t=4.223, p<0.001). The kinds of ingested fish and symptoms, ratio of radiopaque on x-ray and witness were not significantly different between the two groups (p=0.20, 0.38, 0.16, and 0.39, respectively) (Table 3).
In the present study, the authors analyzed 831 medical records of previously healthy pediatric patients with ingestion of foreign body including fish bone between January 1999 and December 2012. At the time of visit, otolaryngologist and pediatric gastroenterologist determined the treatment modality based on the findings of medical history such as the type of foreign body, symptom, physical examination or x-ray. When the ingested foreign body was detected in esophagus and stomach on x-ray, or when the kind of ingested foreign body was suspected to be a disc battery or sharp object, endoscopic examination was conducted preferentially. In 44.9% of the patients, foreign bodies were identified and removed with oropharyngeal examination, x-ray, rigid or flexible endoscope in the present study (Table 1). If the ingested foreign body was not identified, the patient was followed up at the outpatient clinic of the hospital. There was no surgical approach to remove foreign body in the present study. Surgical approach for removal of foreign body has decreased substantially from the past [8]. The decrease of surgery was caused by the advances made in endoscopic technologies and the convenience of the endoscopic approaches. Quick approaches at emergent unit and follow-up actions might facilitate a further decrease in the occurrence of complication or sequelae that would require surgical treatment. In 55.1% of patients, foreign body was removed unsuccessfully in the hospital since it had already passed to distal gut (58 cases, 7.1%) or it was hard to be detected because of too small, radiolucent, or parental refusal for further evaluation (Table 1).
In 237 of 831 patients, no symptom presented after foreign body ingestion. Moreover, ingestion of foreign bodies occurred more frequently in the absence of witnesses than in the presence of witnesses (Table 1). In the absence of witness, foreign bodies were identified and removed from 314 of 454 patients. Such results also indicate that the diagnosis can be delayed. Foreign body ingestion can be easily overlooked as there is no typical clinical symptom [7]. Therefore, the possibility of foreign body ingestion should always be considered in all pediatric patients with atypical symptoms and suspicious histories who visit emergency clinics or hospitals.
Food-related foreign body was the most common (461 patients, 55.5%), followed by toy and magnets (150, 18.1%) and coin (112 patients, 13.5%). The result was different from previous studies, which reported that coins were the most frequently ingested foreign bodies [81112]. The previous studies were conducted on cases in which the foreign bodies were endoscopic removed. Whereas, our study was conducted on the patients who were suspected of ingested foreign bodies or had actually ingested foreign bodies. However, when only the identified and removed foreign bodies in the present study were investigated, fish bones were still more frequently ingested than coins (identified fish bone in 245 patients vs. coin in 112 patients). Fish bone ingestion can occur at a high frequency in countries that consume large amounts of fish, such as South Korea and China [9]. In the present study, the study area is near a river and the coasts of the southern part of Gyeongsangnam-do in South Korea. In contrast to western countries that usually remove fish bones before cooking, most Korean fish dishes (fried, boiled or steamed) are cooked without prior removal of bones. Ingested fish bone was most often found in the pharynx in the present study (Table 2). In adults, fish bone gets stuck in the esophagus in most cases; in contrast, since the laryngopharynx in children is narrower while the tonsil is larger than in adults, fish bones were usually stuck in tonsil within pharynx [131415]. Therefore, endoscopic examination was not always necessary in our subjects with ingestion of fishbone foreign body.
Although foreign body ingestion was frequently occurred in infants younger than 1 year of age [4], fish bone ingestions were occurred more frequently in children older than 1 year of age in the present study. Such difference might be explained by the fact that children younger than 1 year of age usually eat pureed or mid-stage baby food where fish bones have been carefully removed and are usually assisted by guardians. Therefore, most children ingested fish bone accidentally was older than 1 year old. The mean age of identified and removed fish bone group was significantly higher than that of the unidentified group (Table 3). Older children who have higher linguistic capabilities, can accurately describe their clinical symptoms and the ingestion of fish bone in greater detail. Thus, the older children would have been able to notify the doctors of their symptoms and its locations resulting in easier removal of foreign bodies. Moreover, careful removal of fish bones by parents before giving fish to younger children, could also have contributed to the higher mean age of the identified fish bone ingestion group. The parents or guardians might need to pay attention when serving and feeding fish to their children aged older than 1 year. The kinds of fish were very diverse. The kind of fishbone did not related with lodged site in patients and did not different between identified and removed fish bone, and unidentified group.
The significantly shorter interval between accident and hospital visit in the identified and removed fish bone group than that in the unidentified fish bone group could be explained as follows (Table 3). First, since older children in identified and removed fish bone group could explain their symptoms more quickly and location more in detail, they would have needed to visit the hospital more quickly and the fish bone would have been confirmed more easily. Second, when the patients visited the hospital more quickly, intervention for removal of fish bone would have been conducted immediately, and such quick therapeutic approach would have resulted in more efficient removal of the fish bone.
There were several limitations in the present study. First, although this study was conducted on all pediatric patients who had ingested foreign bodies and visited our hospital between 1999 and 2012, many other patients who had ingested foreign bodies might not have visited our hospital because of no or mild symptom. Therefore, this study has a limitation in representing the exact statistical frequency. Second, the research was conducted retrospectively based on the medical records of pediatric patients with impacted fish bone in a single tertiary hospital. However, the accident of fish bone ingestion in pediatric population occurred more commonly than that of coin in this area. Therefore, we tentatively suggest that more attention to children would be necessary during meal with fish. Third, because foreign body or fishbone ingestion was suspected by parents or caregiver's history in the absence of witness, the number of inclusions might be overestimated. However, because most children might have language limitations to describe their own experiences, clinical approaches usually have been performed depending on parent's reports.
In spite of the limitations, the present study showed several meaningful results. First, fishbone was the most common ingested foreign body in children living in this area. Regional characteristics can be affect the frequency of kind of ingested foreign body. Second, pediatric patients with ingested fish bone had excellent clinical outcomes whether removal was successful or not. Third, older child and earlier hospital visit within 2 hours were associated with detection and removal of ingested fishbone. Considering the sharpness of fish bone, extensive examinations to find and remove the ingested fish bone are often warranted. Although endoscopic examination was not always performed in the present study, endoscopic removal could be considered preferentially in case of older child and urgent hospital visit among children suspected fishbone ingestion.
Figures and Tables
Table 1
The Characteristics of Study Population with Ingested Foreign Body Younger Than 15 Years Old (n=831)

*The etc. includes fruit seeds and tablets. †Other objects include a part of a pen, mercury thermometer, artificial teeth and buttons. ‡Symptoms of patients suspected foreign body ingestion were foreign body sensation/pain on neck, nausea/vomiting, and drooling/dysphagia, etc. §In the patients without symptoms, histories of foreign body ingestion or diverse kinds of foreign bodies were noted during the hospitalization.
References
1. Uyemura MC. Foreign body ingestion in children. Am Fam Physician. 2005; 72:287–291.
2. Seo JK. Endoscopic management of gastrointestinal foreign bodies in children. Indian J Pediatr. 1999; 66:1 Suppl. S75–S80.
3. Ayantunde AA, Oke T. A review of gastrointestinal foreign bodies. Int J Clin Pract. 2006; 60:735–739.

4. Hesham A-Kader H. Foreign body ingestion: children like to put objects in their mouth. World J Pediatr. 2010; 6:301–310.

5. Alexander W, Kadish JA, Dunbar JS. Ingested foreign bodies in children. In : Kaufmann HJ, editor. Progress in pediatric radiology. 2nd ed. Chicago: Yearbook Medical Publishers;1969. p. 256–285.
6. Panieri E, Bass DH. The management of ingested foreign bodies in children--a review of 663 cases. Eur J Emerg Med. 1995; 2:83–87.

7. Cha K, Kim SW, Kim JH, Oh SH, Choi SM, Choi KH, et al. The characteristics and outcomes of foreign body aspiration and ingestion in pediatric patients who visit an emergency department. J Korean Soc Emerg Med. 2014; 25:79–83.
8. Choi E, Lee HG, Choi SJ, Chung SY. Clinical analysis of foreign bodies in gastrointestinal tract in children. J Korean Assoc Pediatr Surg. 2014; 20:12–16.

9. Zhang S, Cui Y, Gong X, Gu F, Chen M, Zhong B. Endoscopic management of foreign bodies in the upper gastrointestinal tract in South China: a retrospective study of 561 cases. Dig Dis Sci. 2010; 55:1305–1312.

10. Pfau P. Ingested foreign objects and food bolus impactions. In : Ginsberg GG, Kochman ML, Norton I, Gostout CJ, editors. Clinical gastrointestinal endoscopy. Philadelphia: Elsevier Saunders;2005. p. 291–304.
11. Lee MH, Kang KS, Jung HS, Seo JH, Lim JY, Park CH, et al. Gastrointestinal Foreign Bodies: Review of 96 Cases. Korean J Pediatr Gastroenterol Nutr. 2002; 5:136–142.

12. Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr. 2001; 160:468–472.

13. Chawla A, Eng SP, Peh WC. Clinics in diagnostic imaging (100). Migrated pharyngeal fish bone. Singapore Med J. 2004; 45:397–402.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download