Abstract
Purpose
This study was conducted to analyze the change in the obesity index in girls receiving a gonadotropin-releasing hormone agonist (GnRHa), based on treatment duration, and to aid in nutritional counseling by investigating dietary habits and lifestyle.
Methods
Anthropometric examinations were conducted on 62 girls treated with GnRHa from January 2010 through July 2014. Parents were asked to fill out questionnaires on patient dietary habits and lifestyle.
Results
The group taking GnRHa for over 1 year had a higher rate of obesity increase than the group taking GnRHa for less than 1 year, but they had common habits related to obesity, which should be corrected. In addition, 69.2% of the normal weight group taking GnRHa for over 1 year gained weight, and needed more intensive programs, which include physical exercise and nutritional education. Although girls with precocious puberty showed a decrease in the intake of high-calorie foods with nutritional intervention regardless of treatment duration, they still had problems that needed improvement, such as shorter meals and lack of exercise.
Conclusion
Girls with precocious puberty and their parents should emphasize maintenance of proper body weight, especially when treatment for over 1 year is anticipated. Consistent education in nutrition, ways to increase intensity and duration of physical activity, and the need to slow down mealtimes are important in managing obesity; doctors need to perform regular checkups and provide nutritional counseling.
According to a 5-year statistical report by the Health Insurance Review and Assessment Services for 2006 to 2010, precocious puberty in children and adolescents has rapidly increased in Korea, keeping pace with Western countries. The number of medical personnel increased 4.4 times, from approximately 6,400 to 28,000, and medical costs increased 7.8 times during this period. The reasons for the increase in the number of children with precocious puberty are not clear, but it is assumed that they are related to increases in childhood obesity resulting from Westernized dietary habits and lifestyle, exposure to sexual stimulation through TV and the Internet, endocrine disruptors from environmental pollution, and increase in disease reporting as a result of greater medical facility use, which is consistent with increased parental interest in their children's growth [1]. It is not clear how obesity induces the onset of puberty, but visceral fat accumulation has been noted as a metabolic control factor affecting the central nervous system, which controls the onset and progression of puberty, particularly through early activation of periodic gonadotropin-releasing hormone (GnRH) secretion [2]. Furthermore, most girls with precocious puberty have an above-average obesity index with respect to their chronological age, before GNRH agonist (GnRHa) treatment, which can interfere with treatment effects if weight control is ineffective [34].
This study analyzed obesity index changes in girls with precocious puberty who needed more than 2 years of GnRHa treatment, as well as the dietary habits of girls who need weight loss along with GnRHa treatment. Although there has been much research and interest in the dietary habits of children and adolescents, particularly those who are obese, few studies have investigated the dietary habits of girls with precocious puberty. This study aims to contribute to treatment and nutritional counseling of girls with precocious puberty.
From March 1 to October 30 in 2014, this study surveyed 70 girls diagnosed with true precocious puberty from January 2010 to July 2014 at the Department of Pediatrics, Presbyterian Medical Center (Jeonju, Korea) and who have since been treated. The subjects were included only when they or their mothers agreed to the survey; the final number of subjects was 62, excluding five who did not give consent and three who provided incorrect information on the questionnaire. True precocious puberty was diagnosed when secondary sexual characteristics appeared before age 8 years, bone age was in advance of chronological age, and the maximum luteinizing hormone level was above 5 IU/L in a GnRH stimulation test, excluding cases with a serious underlying condition such as brain tumor, thyroid abnormality, or other disease [5]. The number of medical personnel involved in treating girls was 12.3 times greater than that in treating boys, and the proportion of girls (92.5%) was greater than that of boys (7.5%) in hospital variance analysis, according to the 2010 statistics reported by the Health Insurance Review and Assessment Service. Furthermore, cases in boys were often caused by the presence of an underlying condition. Thus, this study included only girls. This study was approved from the institutional review board of Presbyterian Medical Center (IRB no. 2014-04-019).
Age, height, and weight were determined from the medical records at the time of diagnosis, and height and weight were determined every 3 months after GnRHa treatment began. Anthropometric height and weight were measured using an automatic height-weight meter (Fatness Measuring System, DS-102; Dongasn Jenix, Seoul, Korea). Obesity index were calculated using the formula: (actual weight−standard weight for height)/standard weight for height×100. The results were categorized into "normal" (−10 to +10), "overweight" (10 to 20), and "obese" (over 20) groups, and were compared with standard weights specified by the Korean Society of Pediatrics in the "2007 Korean children and adolescents physical growth standard measurements" [67].
In nutritional counseling at the hospital before and after anthropometry, overweight and obese patients were asked about issues such as meal times and food intake, based on which their intake calories were analyzed and food substitutions were proposed. The subjects visited the hospital for anthropometry every 3 months, when their food intake and dietary habits were checked and feedback was provided. The questionnaire on dietary habits used in this study were based on the 2008 revised obesity questionnaire by the Korean Society of Pediatrics Nutrition Committee, which includes 43 questions about family relationships, dietary habits, main types of food intake and late-night meals, lifestyle, and health management [8]. The mean treatment duration for girls with precocious puberty is 27.9±9.0 months; therefore, this study categorized median values into 2 groups, based on 1-year treatment periods, starting from before the beginning of treatment [9].
Data were processed using SAS software (version 9.1; Cary, NC, USA). Anthropometric measurements were shown as mean±standard deviation; treatment periods were indicated by median values and interquartile ranges (IQRs); categorical variables were indicated by frequency and percentile. For each item of the obesity index, the differences between the weight gain (WG) and weight loss (WL) groups were analyzed using the chi-square test, and values of p<0.05 were considered statistically significant.
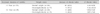
The age of the 62 subjects ranged from 5 to 9 years when diagnosed with precocious puberty, with a median value of 8 years (IQR 7-8), with 3 girls aged 5 years (4.8%), 7 girls aged 6 years (11.3%), 18 girls aged 7 years (29.0%), 28 girls aged 8 years (45.2%), and 6 girls aged 9 years (9.7%). The age of the subjects ranged from 6 to 11 years when dietary habits were surveyed, with a median value of 9 years (IQR 8-10). Their mean height and weight for age before starting GnRHa treatment were all higher than mean values in comparison with standards specified by the Korean Society of Pediatrics, with obesity index somewhat high (Table 1). The results revealed that the overweight subject ratio was higher during the dietary habits survey than before precocious puberty treatment. Before treatment, 9 overweight subjects (14.5%) had an obesity index of above 10% and 7 subjects (11.3%) showed an obesity index of above 20%; during the dietary habit survey, there were 13 overweight subjects (21.0%) and 7 obese subjects (11.3%), which was higher than the obesity ratio before treatment. However, in comparing overweight and obesity ratios with the body mass index (BMI), 14 subjects (22.6%) had a BMI above the 85th percentile and 2 (3.2%) had a BMI above the 95th percentile, both before treatment and during the survey.
Anthropometric measurement of subjects' fathers showed a mean height of 172.32±0.59 cm, mean weight of 73.03±0.95 kg, and median obesity index value of 9.95 (IQR 6.30-13.58); measurements of their mothers showed a mean height of 159.33±0.61 cm, mean weight of 57.10±1.00 kg, and median obesity index value of 1.15 (IQR −6.75-10.35).
In this study, the GnRHa treatment duration was 6-42 months (from initial diagnosis to the dietary habit survey), with a median value of 15 months (IQR 9-27). The 62 subjects were categorized as patients whose GnRHa treatment period was over 1 year (Group A) and those who had less than 1 year of treatment (Group B); their weight changes during treatment were compared for obesity index: Group A, 66.6% (22/33); Group B, 41.4% (12/29). The obesity index significantly increased in Group A (p=0.046) (Table 2). Among the 33 patients in Group A, 26 belonged to the normal weight group, but 18 (69.2%) showed an increase in obesity index during compared to before the survey (Table 3).
Of the 62 subjects, 62.9% (39/62) took less than 20 minutes for a meal. When these 39 subjects were categorized into WG and WL groups with the obesity index for comparison, 73.5% (25/34) of the WG group and 50.0% (14/28) of the WL group took less than 20 minutes for a meal, demonstrating a significantly shorter meal time in the WG group (p=0.032). The rates of skipping breakfast among subjects were 3.3% (2/60), when "skipping breakfast" was defined as 5 days out of 7. Furthermore, 85.5% (53/62) of the subject sate the largest amount during dinner, but the differences were statistically insignificant. Fast food was eaten at least once a week by 40.3% (25/62). Moreover, 71.0% (44/62) did not drink carbonated beverages; however, the ratios were 82.4% (28/34) in the WG group and 57.1% (16/28) in the WL group, showing significantly higher numbers in the WG group (p=0.030). Most subjects did not habitually have late-night meals (snacks)—often less than once a week—but statistical significance was not detected for obesity index. For late-night meals, fruits predominated, followed by snack foods, noodles, and fatty foods (Table 4).
Of 33 subjects in the two groups, 77.3% (17/22) of the WG group and 45.5% (5/11) of the WL group took less than 20 minutes for a meal, with significantly shorter meal time in the WG group (p=0.025). Regarding timing of late-night meals, 50.0% (11/22) of the WG group and 18.2% (2/11) of the WL group ate later than 8 pm, with significantly later times in the WG group (p=0.045).
Of 62 subjects in the survey of weekly exercise hours, 73.5% (25/34) of the WG group and 53.6% (15/28) of the WL group answered "either do not exercise or for less than 30 minutes," showing significantly fewer hours in the WG group (p=0.048). As for TV, 47.1% (16/34) of the WG group and 17.9% (5/28) of the WL group spent longer than 3 hours watching TV on weekends, with significantly longer hours in the WG group (p=0.049). The subjects spent less than 1 hour on the computer both during the week and on weekends in most cases; there were no significant differences between use during the week and on weekends (78.7% [48/61] vs. 69.5% [41/59]). In addition, no significant difference was found between the 2 groups in accordance with the obesity index (Table 4).
Of 33 subjects, 45.5% (10/22) of the WG group and 18.2% (2/11) of the WL group spent longer than 3 hours watching TV on weekends, with significantly longer hours in the WG group (p=0.042).
Among the mothers, 71.0% (44/62) stated that "precocious puberty is related to obesity." When asked if they tried measures other than hospital treatment and were allowed multiple responses, 38.7% (24/62) reported diet control, 38.7% (24/62) reported exercise, and 11.3% (7/62) reported reducing TV watching or computer use hours. When asked where they obtained relevant dietary information on precocious puberty and were allowed multiple responses, they reported the Internet at 62.9% (39/62), family and friends at 17.7% (11/62), pediatric doctors at 17.7% (11/62), and TV at 11.3% (7/62). Regarding nutrition counseling for precocious puberty provided at the hospital, the response was "helpless", "little helpful", or "very helpful" in 8.9% (5/56), 73.2% (41/56), and 17.9% (10/56), respectively (Table 5).
There is a worldwide trend toward puberty onset at a younger age, and the frequency of precocious puberty has increased in girls. GnRHa treatment in patients with precocious puberty slows the progression of puberty and bone maturation by suppressing the hypothalamic-pituitary-gonadal axis, and thus extends the period of puberty, eventually increasing the final height in adulthood [1011]. Many studies have investigated the effects of precocious puberty treatment on adult height and weight but anthropometric changes have not been clearly identified during treatment [12]. Aguiar et al. [13] studied the effects for 2 years after GnRHa treatment in 176 girls with precocious puberty, and reported that BMI was significantly greater after compared to before treatment. In addition, the amount of BMI increase was greater in girls with normal weight before treatment compared to girls with obesity. On the other hand, Arrigo et al. [14] investigated the obesity ratio and BMI changes in girls who underwent GnRHa treatment for over 2 years and reported a decrease in obesity ratio, leaving room for discussion.
This study compared obesity index in accordance with GnRHa treatment duration and found that the obesity index significantly increased in Group A (Table 2). It is not clear if the weight changes are related to precocious puberty treatment, or the increase was seen in the growth of girls with precocious puberty with above-average obesity index. However, medical personnel must monitor weight increase in patients during GnRHa treatment. Furthermore, among the patients in Group A, the obesity index increased during treatment in 69.2% of those in the normal weight group compared to the beginning of treatment (Table 2). This can be due to either lack of effort to control obesity with diet or correction of lifestyle at the beginning of treatment when children are at normal weight, or lack of parental involvement. Moreover, obesity prevention management and nutritional counseling in the normal weight group provided by the hospital can be insufficient. Thus, consistent follow-up and nutritional counseling for weight increase are also needed in the normal weight group until treatment is finished, along with periodic physical examinations and evaluation of dietary habits.
Approximately 80% of childhood obesity cases can progress to adult obesity. It has been reported that one-third of adult obesity cases that began in childhood and adolescence resulted from an increase in the size and number of lipocytes [15]. Dietary habits and lifestyle are controllable causes and nutritional education during childhood is very effective in development of dietary habits. Dietary attitudes and habits benefit from greater nutritional knowledge. Therefore, it is very important to identify and correct the effects of dietary habits on the obesity index [16]. This study categorized dietary habits into WG and WL groups in accordance with obesity index, and focused on means of improvement. The results showed that 73.5% of the WG group and 50.0% of the WL group took less than 20 minutes for a meal, with a significantly greater percentile in the WG group. It takes longer than 20 minutes for a human to feel satiety, and therefore one can eat more as well as more often when eating fast [1718]. Furthermore, 3% of girls with precocious puberty skipped breakfast, which was lower than the 13.6% reported for girls aged 6-11 years in the 2013 National Health and Nutrition Survey. Having a good breakfast can reduce the amount of snack and excessive calorie intake at lunch by girls undergoing treatment for precocious puberty, and help with weight management [19]. Out of 3 meals, the greatest amount of food intake occurred during dinner. Greater amounts of fat from the same amount of food can accumulate in the body if taken at night rather than during the day, because the sympathetic nervous system facilitates energy consumption during the day; at night, the parasympathetic nervous system tends to facilitate energy conservation [2021]. Thus, during nutritional counseling of girls with precocious puberty, it is necessary to recommend changes in dietary habits, such as eating breakfast, reducing the amount of food intake at dinner, and to eat slowly, to prevent obesity by maintaining good dietary habits during treatment (Table 4). Carbonated beverages were not consumed during the week by 71.0% of the subjects in this study. Considering the 26% reported by the 2009 children's dietary life survey by the Ministy of Food and Drug Safety in Korea for 2,772 fifth-grade students, this demonstrated that the subjects were careful to avoid foods contributing to weight gain compared to patients with precocious puberty in general. In comparing the 2 groups in this study regarding carbonated beverages, the ratios were 82.4% in the WG group and 57.1% in the WL group, with significantly higher numbers in the WG group (Table 4). This is presumably because parents intervened more actively regarding consumption of high-calorie food intake, including carbonated beverages, when children showed a weight increase during treatment.
According to a 2012 study on actual involvement in physical activities by lower-income children and adolescents and a report by the National Youth Policy Institute conducted in 1,745 elementary, middle, and high school students in Seoul, the mean daily exercise hours of elementary school students was 69.9 minutes. Among subjects in this study, 93.5% spent less time exercising than elementary school students whose exercise time was less than one hour. Furthermore, in looking at the weekly exercise hours of the subjects, 73.5% of the WG group and 53.6% of the WL group answered "either do not exercise or for less than 30 minutes," with significantly fewer hours in the WG group (Table 4). Thus, exercise counseling needs to educate subjects to slowly and steadily extend exercise hours rather than increasing hours all at once; when they cannot set aside time for exercise, advise them to exercise eat other times, such as climbing stairs, walking fast on the way to school, tread-walking, or stretching while watching TV [22]. As for TV watching, 47.1% of the WG group and 17.9% of the WL group spent longer than 3 hours watching TV on weekends, with significantly longer hours in the WG group (Table 4). According to the 2005 National Health and Nutrition Survey, obesity risk did not increase with less than 2 hours of TV watching or computer usage, but doubled with 2-3 hours, and increased by up to 4.7 times in proportion to the hours. Gordon-Larsen et al. [23] reported in their 2002 study on middle and high school students that obesity risk was proportional to TV-watching hours and inversely proportional to significant physical activity. Thus, girls with precocious puberty are advised not to spend their increased leisure time watching TV on weekends but to spend more time with family or exercising; parents need to set an example by reducing TV-watching hours.
Patients of the WG group had dietary habits in need of intervention, such as fast eating, latemeals, and lengthy TV-watching hours during the weekend. Despite education on anthropometry, correction of dietary habits, nutrition, and exercise by medical personnel when subjects visited the hospital once a month, the initial attention of parents and patients tended to decrease over time. The mean treatment duration for precocious puberty is 27.9±9.0 months and extends to over 2 years, depending on timing of menarche or final adult height. In general, treatment stops in girls when bone age 12-12.5 years [2425]. Thus, involvement by medical personnel is needed to provide education for more specific interests in accordance with GnRHa treatment duration.
Among mothers of girls with precocious puberty, 71.0% stated that "precocious puberty is related to obesity," and most obtained information on precocious puberty through the Internet, while 82% were not satisfied with hospital nutritional counseling (Table 5). This indicates that a hospital needs to provide not only relevant information about precocious puberty, obesity, dietary habits, and nutritional counseling, but also concrete interventions, e.g., a dining diary, menu-planning, and exercise programs using multiple approaches involving nutritionists and exercise therapists along with medical personnel. Moreover, nutrition and dietary education are needed both for patients with precocious puberty and their parents. The Ministy of Food and Drug Safety in Korea investigated dietary habits in 1,084 elementary and middle school students in Seoul from June to July 2011, and found that nutrition and dietary education were useful in forming healthy dietary and exercise habits. The skipped breakfast rate was 12.4% in students who received nutrition and dietary education, but 17.5% in students who did not. The ratio of students who drank carbonated beverages more than 3 times a week was 19.4% among those who received nutrition and dietary education and 22.2% among those who did not. Furthermore, the ratio of vigorous physical activity (exercising for longer than 20 minutes to the point of sweating or having difficulty breathing or shortness of breath) was found to be 58.1% in students who received nutrition and dietary education and 49.8% among those who did not. In comparing moderate physical activity (exercising for longer than 30 minutes or until slight difficulty breathing or shortness of breath), the ratio was 23.3% in students who received nutrition and dietary education and 17.6% among those who did not. Thus, education an affect exercise habits. Nutritional counseling and education provided at the hospital plays an important role in improving dietary habits. However, active support from the surrounding environment must be provided, and requires changes in family behavior, because family and parents can assist in obesity prevention, and play an important role in family-oriented behavioral intervention [2627]. Epstein et al. [28] conducted a weight loss program with 3 groups: parents and children, children, and family, and reported that the parents and children group showed the greatest weight loss over 5 years, indicating that parents and children can mutually effect behavioral changes related to food intake and weight loss. Moreover, preschool children eat foods in the way their parents do, and their nutritional intake pattern is also related to that of their parents [2930]. Thus, parents must monitor the dietary habits of their children and keep records, thereby identifying bad habits and making efforts to correct them, along with help from medical personnel and the community.
In conclusion, girls with precocious puberty had dietary habits and lifestyles related to obesity, such as fast eating and less physical activity, which require intervention. In particular, since precocious puberty treatment requires more than 2 years, medical personnel need to take a personal interest in patients and make more effort to investigate problematic dietary habits during GnRHa treatment. Furthermore, consistent nutritional education for both parents and patients along with promoting interest in weight-watching are also needed in the normal weight group, with periodic physical examinations and nutrition counseling.
This study has limitations due to a small number of subjects at a single hospital using questionnaires. In addition, a normal reference group was not used, making it difficult to generalize to other patients with precocious puberty. However, the study proposed a direction for nutritional counseling and thereby contributed to treatment by analyzing weight change and obesity-related dietary habits in accordance with the treatment of patients with precocious puberty. In the future, proper nutritional counseling and education guidelines will be obtained by conducting long-term and large-scale tracking and observation studies, and by analyzing data on obesity-related dietary habits of patients with precocious puberty.
Figures and Tables
Table 3
Difference of Obesity Index Change between Overweight/Obesity and Normal Weight according to Treatment Duration
References
1. Shim KS, Kim JT. Therapy for idiopathic precocious puberty in children. J Korean Med Assoc. 2011; 54:953–956.

2. Burt Solorzano CM, McCartney CR. Obesity and the pubertal transition in girls and boys. Reproduction. 2010; 140:399–410.

3. Styne D, Grumbach M. Puberty. In : Kronenberg HM, Melmed S, Polonsky KS, Larsen PR, editors. Williams textbook of endocrinology. 11th ed. Philadelphia: Saunders Co;2008. p. 969–1166.
4. Rosenfield RL, Lipton RB, Drum ML. Thelarche, pubarche, and menarche attainment in children with normal and elevated body mass index. Pediatrics. 2009; 123:84–88.

5. Rosenfield RL, Cooke DW, Radovick S. Puberty and its disorder in the female. In : Sperling MA, editor. Pediatric endocrinology. 4th ed. Philadelphia: WB Saunders Co;2014. p. 569–663.
6. Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, et al. 2007 Korean National Growth Charts: review of developmental process and an outlook. Korean J Pediatr. 2008; 51:1–25.

7. Knittle JL, Merritt RJ, Dixon-Shanies D, Ginsberg-Fellner F, Timmers KI, Katz DP. Childhood obesity. In : Robert MS, editor. Textbook of pediatric nutrition. 2nd ed. New York: Raven Press;1981. p. 415–434.
8. Seo JW, Jung JA, Park HS, Ko JS, Kim YJ, Kim JY, et al. Assessment of modifiable lifestyle factors for obese children and adolescents through questionnaires. Korean J Pediatr. 2008; 51:576–583.

9. Shalitin S, Phillip M. Role of obesity and leptin in the pubertal process and pubertal growth--a review. Int J Obes Relat Metab Disord. 2003; 27:869–874.

10. Lebrethon MC, Bourguignon JP. Management of central isosexual precocity: diagnosis, treatment, outcome. Curr Opin Pediatr. 2000; 12:394–399.

11. Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993; 22:167–177.

12. Yoon JY, Kang MJ, Kim SY, Seo JY, Yang SW, Lee YA, et al. The relationship between initial body mass index and body mass index after one year of gonadotropin-releasing hormone agonist therapy in idiopathic true precocious puberty girls. J Korean Soc Pediatr Endocrinol. 2011; 16:165–171.

13. Aguiar AL, Couto-Silva AC, Vicente EJ, Freitas IC, Cruz T, Adan L. Weight evolution in girls treated for idiopathic central precocious puberty with GnRH analogues. J Pediatr Endocrinol Metab. 2006; 19:1327–1334.

14. Arrigo T, De Luca F, Antoniazzi F, Galluzzi F, Segni M, Rosano M, et al. Reduction of baseline body mass index under gonadotropin-suppressive therapy in girls with idiopathic precocious puberty. Eur J Endocrinol. 2004; 150:533–537.

15. Kim MS, Choi MS, Kim KN. Effect of nutrition education and exercise intervention on physical and dietary patterns of some obese. Korean J Community Nutr. 2011; 16:426–438.

16. Kim JH, Choi YJ, Lim HS, Chyun JH. Improvement of food habits and eating behavior of children with obesity and precocious puberty by nutrition education monitoring. J Korean Soc Food Cult. 2015; 30:129–136.

17. Cho KY, Park H, Seo JW. The relationship between lifestyle and metabolic syndrome in obese children and adolescents. Korean J Pediatr Gastroenterol Nutr. 2008; 11:150–159.

18. Hassink SG. Pediatric Expert Panel. Weighing risk: the expert committee's recommendations in practice. Semin Pediatr Surg. 2009; 18:159–167.

19. Ashwell M. An examination of the relationship between breakfast, weight and shape. Br J Nurs. 2010; 19:1155–1159.

20. Akselrod S, Gordon D, Madwed JB, SnidmanNc , Shannon DC, Cohen RJ. Hemodynamic regulation: investigation by spectral analysis. Am J Physiol. 1975; 228:775–780.

21. Guyton AC, Hall JE. The autonomic nervous system and the adrenal medulla. In : Rebecca G, editor. Guyton and Hall textbook of medical physiology. 12th ed. Philadelphia: WB Saunders Co;2011. p. 729–739.
23. Gordon-Larsen P, Adair LS, Popkin BM. Ethnic differences in physical activity and inactivity patterns and overweight status. Obesity Research. 2002; 10:141–149.

24. Carel JC, Eugster EA, Rogol A, Ghizzoni L, Palmert MR, Antoniazzi F, et al. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics. 2009; 123:e752–e762.

25. Baek JW, Nam HK, Jin D, Oh YJ, Rhie YJ, Lee KH. Age of menarche and near adult height after long-term gonadotropin-releasing hormone agonist treatment in girls with central precocious puberty. Ann Pediatr Endocrinol Metab. 2014; 19:27–31.

26. Gruber KJ, Haldeman LA. Using the family to combat childhood and adult obesity. Prev Chronic Dis. 2009; 6:106–107.
27. Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med. 2004; 158:342–347.

28. Epstein LH, McCurley J, Wing RR, Valoski A. Five-year follow-up of family-based behavioral treatments for childhood obesity. J Consult Clin Psychol. 1990; 58:661–664.

29. Barlow SE. Expert Committee. Expert Committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007; 120:Suppl 4. S164–S192.

30. Seo JW. Management of nutrition and eating behavior in obese children adolescents. Korean J Pediatr Gastroenterol Nutr. 2008; 11:Suppl 1. 93–101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download