Abstract
Purpose
Regurgitation is a common physiological phenomenon in infants. The aim of the present study was to evaluate the efficacy of a new anti-regurgitation (AR) formula (Novalac), thickened with an innovative complex including fibres, on the daily number of regurgitations and to assess its impact on stool consistency and frequency.
Methods
Infants younger than five months, presenting at least 5 regurgitations per day were recruited in this trial. The efficacy of the new formula on regurgitation (daily number and Vandenplas score), stool frequency and consistency were assessed at day 14 and 90. Growth data were recorded at each study visit.
Results
Ninety babies (mean age 9.6±5.8 weeks) were included in the full analysis data set. The mean number of regurgitation episodes at inclusion was 7.3±3.4. In all infants, regurgitations improved after 2 weeks. The daily number of regurgitations decreased significantly (-6.3±3.3, p<0.001) including in those previously fed a thickened formula (-6.2±3.0, p<0.001). There was no significant change in stool consistency at day 14. After 3 months, 97.5% of infants had formed or soft stools. Growth was appropriate with a slight increase of weight-for-age z-score (from -0.5±1.0 to -0.1±0.9) and no change of weight-for length z-score (-0.1±1.1 to -0.1±-1.1).
Regurgitation is a common physiologic phenomenon in infants with a peak prevalence at three to four months of age and occurs during this period in 50% to 70% of infants [123]. According to a thorough review of the literature, about 25% of the parents seek medical help because of infant regurgitation [4].
According to the NASPGHAN-ESPGHAN guidelines on the management of reflux, the recommended course of action in case of regurgitation is "parental education, reassurance and anticipatory guidance, and in formula fed infants, a thickened formula (or anti-regurgitation [AR] formula if available) to reduce the frequency of overt regurgitation and vomiting" [1].
Currently, several pre-thickened AR infant formulas using different types of thickening agents are available for the management of regurgitation [5].
The clinical efficacy on regurgitation of AR formulas thickened with locust bean has been demonstrated in several clinical trials [678]. However, infants fed with such formulas may have softer and more frequent stools than those fed with starch-thickened formulas [9].
The aim of this trial was to evaluate the efficacy of a formula containing a new thickening agent on regurgitation and to assess its digestive tolerance.
This prospective international open pilot multicentre clinical trial was conducted to evaluate the efficacy of a new formula (Novalac, Paris, France) on regurgitation and defecation. The formula contains an innovative thickening complex made of fibres including specially selected pectin. Fully formula fed infants less than 5 months old with at least 5 episodes of regurgitation per day and who had not yet started solids were eligible for inclusion.
After informed consent was obtained, the parents were given the appropriate number of tins of formula needed to cover their infant's needs for two weeks (±3 days). Parents were asked to report information on regurgitation and stools consistency in a diary during two 3-day periods: just after inclusion and just before day 14, when the infant was re-examined by the investigator.
After this visit, if an AR formula was still indicated and if parents wished to continue with the same formula, the investigator could provide more tins of the new AR formula for up to three months after inclusion or until the child reached the age of six months whichever occurred last. A third visit was planned 90 days after inclusion to further assess growth.
The efficacy of this new AR formula on regurgitation was assessed through the daily number of regurgitations and the estimated regurgitated volume (adapted Vandenplas score [8]; Table 1). The daily number of stools and stools consistency according to the Bristol scale were also recorded [10]. For analysis, four categories were defined regarding stool consistency: hard (Bristol scale 1, 2), formed (Bristol scale 3, 4), soft/mushy (Bristol scale 5, 6) and loose/watery (Bristol scale 7).
The growth parameters (weight, length, and head circumference) were collected at baseline, day 14, and day 90. Anthropometric parameters, including the body mass index (BMI) were expressed as z-score according to the World Health Organization Child Growth Standards [11].
The safety population was defined as all infants who consumed at least once the product. The full analysis set population is composed of all infants having an evaluation of the main outcome, i.e., the daily number of episodes of regurgitation at day 14. A posteriori, two subgroups were analysed according to whether the infants had or had not been fed with a thickened formula prior to inclusion.
The SAS software for Windows (version 9.2; SAS Institute, Cary, NC, USA) was used to perform the statistical procedures. Statistical analyses were performed in accordance with ICH-E9 guideline.
The study was approved by independent ethics committees: CPP Ile-de-France III, Paris, France, and VUB Ethics Committee, Brussels, Belgium. It was registered at ClinicalTrials.gov under the identifier NCT02425423. Parents or others legally responsible for the infants provided written consent.
Sixteen paediatricians (five in Belgium and eleven in France) included 100 infants. After 14 days of treatment, 90 infants (mean age at inclusion 9.6±5.8 weeks) were included in the full analysis data set (Fig. 1). The reason for drop-out between inclusion and day 14 were identified as follows; liquid stools (n=4), lost to follow up (n=1), withdrawal by parents for unknown reason (n=4), and one infant that was breastfed (n=1).
About half of the infants (48/90; 53.3%) had been fed a thickened formula before inclusion (pre-thickened or standard formula+thickening agent), but had still at least 5 episodes of regurgitation per day.
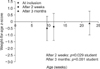
The mean number of regurgitation episodes was 7.3±3.4 at inclusion. After 14 days, the mean number of regurgitation had decreased significantly with -6.3±3.3 (p<0.001) (Table 2 and Fig. 2). In the subgroup of infants who were fed a thickened formula at inclusion, regurgitation also significantly decreased from 7.1±2.9 to 0.9±-1.1 after 14 days. There was no difference between both sub-populations regarding the effect on regurgitation. After two weeks, regurgitations decreased in all infants and 85.6% had no more than two regurgitations per day. Parents reported a significant decrease of the daily number of regurgitation already after three days: -6.1±3.7, p<0.001 with improvement in 94.5% (52/55). The regurgitation score had also decreased significantly after 14 days (Table 2).
There was no significant effect of the formula on stool consistency with 78.9% of infants having soft/mushy or formed stools at inclusion and 87.8% after 14 days (Table 3). The percentage of formed stools increased after 14 days from 36.7% to 51.1% (p=0.053).
Growth was within normal range, with an increase of the weight for age z-score
(-0.5±1.0 at inclusion and -0.1±0.9 after 3 months, p<0.001), length for age z-score
(-0.5±1.2 at inclusion and -0.0±1.2 after 3 months, p<0.001) and BMI for age z-score
(-0.3±1.0 at inclusion, and -0.2±1.1 after 3 months, not significant) (Fig. 3).
After 14 days, 66 parents answered the question regarding general satisfaction and 61 (92.4%) were in overall satisfied or very satisfied. Seventy-one parents answered the question about efficacy on regurgitation, and 67 (94.3%) said to be satisfied or very satisfied. Regarding the digestive comfort and general well-being of their child, as of day 3, respectively 76.1% (54/72) and 80.3% (57/71) of the parents reported to be satisfied or very satisfied. After 2 weeks, 87.8% (79/90) and 94.4% (85/90) of the paediatricians reported to be satisfied or very satisfied regarding respectively the digestive comfort and general well-being.
Thickening of infant formula is considered as an option to reduce regurgitation [1]. However, the efficacy and risk for adverse effects of all thickeners is not equal. For example, according to the meta-analysis by Horvath et al. [12], only corn starch thickened formulas have an impact on reflux index.
This pilot study has shown that the AR formula with the new thickening agent is effective in the treatment of regurgitation. As the study was not controlled and regurgitations do naturally decrease over time, the primary endpoint was evaluated only two weeks after inclusion. Actually, parents reported a significant decrease of the number of episodes of regurgitation as of day three, what minimalizes the effect of natural evolution. Moreover, the decrease in regurgitation was similar in infants already under AR formula but still regurgitating more than five times a day at inclusion. A major weakness of this open observational study is the lack of a control group. However, the short observation period of only two weeks and the fact that the reduction in regurgitation was similar in the group that had been treated before with an AR formula without success and new untreated infants makes it unlikely that the reduction in episodes of regurgitation is due to the natural evolution. A placebo effect of a formula on infant regurgitation seems also unlikely. Another shortcoming is that no information has been acquired on irritability or time needed for feeding. As the main objective of this study was to evaluate the impact on regurgitation and on stools, for which the record by the parents was very important, it was decided to keep the parents' diary as simple as possible to ensure a better quality of the data recorded. Therefore parents were not required to report precise information such as the duration of each feeding nor on the daily crying time. Irritability was evaluated through two questions about digestive comfort and global well-being.
This formula is thickened with a complex of fibers containing pectins. Pectins are safe and naturally present in fruits such as apple, frequently eaten by young infants. According to European Union regulation, pectins can be used in baby foods, cereals or food for special medical purposes for newborns. Moreover, special formulae containing pectins have been used in recent clinical trials on thickened formulae specially designed for the treatment of cow's milk allergy; they all show an adapted growth of the infants fed such formula for a duration up to 6 months [1314].
Depending on the nature of the thickening agent, the impact on the stool frequency and consistency can differ. For example with a formula thickened with locust bean, Iacono et al. [9] reported diarrhea to occur in 16.7% (14/84) of infants. Although the new formula is thickened with fibres and even though four children have left the study before day 14 due to loose stools, this formula seems to have a regulatory effect on stool composition. Indeed, 87.8% of the infants had soft or formed stools after 14 days, and 97.5% after three months.
It is important to assure optimal nutritional intake, especially in regurgitating infants. This new formula allowed a satisfactory growth over the three months of observation. This study shows that a formula containing a new thickening agent gives promising results not only in term of regurgitation but also without causing diarrhea or constipation.
Figures and Tables
Fig. 2
Evolution of the daily mean number of regurgitations and Vandenplas score from inclusion to 14 days.

ACKNOWLEDGEMENTS
Christophe Dupont received fees from Nestlé, United Pharmaceuticals, Danone, Sodilac; Yvan Vandenplas is consultant for Aspen, Ausnutria, Biocodex, Nestle Nutrition Institute and United Pharmaceuticals.
United Pharmaceuticals provided the tested formula and financial support.
References
1. Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr. 2009; 49:498–547.

2. Martin AJ, Pratt N, Kennedy JD, Ryan P, Ruffin RE, Miles H, et al. Natural history and familial relationships of infant spilling to 9 years of age. Pediatrics. 2002; 109:1061–1067.

3. Nelson SP, Chen EH, Syniar GM, Christoffel KK. Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med. 1997; 151:569–572.

4. Vandenplas Y, Abkari A, Bellaiche M, Benninga M, Chouraqui JP, Çokura F, et al. Prevalence and health outcomes of functional gastrointestinal symptoms in infants from birth to 12 months of age. J Pediatr Gastroenterol Nutr. 2015; 61:531–537.

5. Vandenplas Y, Lifshitz JZ, Orenstein S, Lifschitz CH, Shepherd RW, Casaubón PR, et al. Nutritional management of regurgitation in infants. J Am Coll Nutr. 1998; 17:308–316.

6. Vandenplas Y, Gutierrez-Castrellon P, Velasco-Benitez C, Palacios J, Jaen D, Ribeiro H, et al. Practical algorithms for managing common gastrointestinal symptoms in infants. Nutrition. 2013; 29:184–194.

7. Wenzl TG, Schneider S, Scheele F, Silny J, Heimann G, Skopnik H. Effects of thickened feeding on gastroesophageal reflux in infants: a placebo-controlled crossover study using intraluminal impedance. Pediatrics. 2003; 111:e355–e359.

8. Vandenplas Y, Hachimi-Idrissi S, Casteels A, Mahler T, Loeb H. A clinical trial with an "anti-regurgitation" formula. Eur J Pediatr. 1994; 153:419–423.

9. Iacono G, Vetrano S, Cataldo F, Ziino O, Russo A, Lorello D, et al. Clinical trial with thickened feeding for treatment of regurgitation in infants. Dig Liver Dis. 2002; 34:532–533.

10. Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997; 32:920–924.

11. World Health Organization. WHO Multicentre Growth Reference Study Group: WHO Child Growth Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization;2006. Available from: http://www.who.int/childgrowth/standards/en/.
12. Horvath A, Dziechciarz P, Szajewska H. The effect of thickened-feed interventions on gastroesophageal reflux in infants: systematic review and meta-analysis of randomized, controlled trials. Pediatrics. 2008; 122:e1268–e1277.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download