INTRODUCTION
Melena refers to tarry black stool, which is one of the most common gastrointestinal symptoms in pediatric patients [
1,
2]. Melena is frequently observed in upper gastrointestinal bleeding (UGIB) above the ligament of Tretiz. It can also be seen in the small intestine and proximal colon bleeding [
3,
4].
Melena is associated not only with slow or brisk bleeding, but also with a relatively small amount (50-100 mL) of bleeding in the stomach. The symptom can continue for up to three to five days after the bleeding has stopped [
5]. In the case of fast or massive bleeding, hematochezia appears in advance, which means higher bleeding rate than that of the tarry black stool [
2]. Diseases that can cause high-rate bleeding in children include esophageal varices, gastric or duodenal ulcer, Dieulafoy lesions, arteriovenous malformation, and Meckel's diverticulum [
4]. In children, melena is commonly induced by esophageal varices, peptic ulcer diseases (PUD) and Meckel's diverticulum. When bleedings occur due to such diseases, assessment of hemodynamic status and stabilization should be prioritized, followed by evaluation of bleeding causes and proper management [
2,
6]. Initially, the bleeding sites are assessed according to the age, hematemesis, melena patterns, abdominal pain and its location, other gastrointestinal symptoms, finding of gastrointestinal lavage, and clinical presentation of known underlying diseases [
1,
6]. The gastric lavage can clearly identify the presence of esophageal or gastric bleeding, but gives discomfort to patient and low yield in duodenal bleeding [
2].
In contrast, the blood urea nitrogen to creatinine ratio (BUN/Cr ratio) is known as a simple test to differentiate UGIB from lower gastrointestinal bleeding (LGIB) [
7,
8,
9]. The urea nitrogen increases following gastrointestinal bleeding because of an increased absorption of blood protein from the small intestine or a decreased renal excretion of urea nitrogen due to hypovolemic state. It has been reported that the BUN/Cr ≥30 in children implies UGIB [
5,
10,
11]. However, PUD can show a relatively small amount of bleeding and melena can occur even in a small amount of bleeding in children. In such cases, the increase in BUN can be insignificant. In addition, the aforementioned researches were performed targeting all GIB without differentiating diverse causes presented with different patterns of bleeding.
We investigated the availability of the BUN/Cr ratio to distinguish UGIB from LGIB and its difference between two major causative diseases of UGIB in children that developed melena.
MATERIALS AND METHODS
All patients who were investigated to identify causes of GIB that presented with melena at the Department of Pediatrics of Chungnam National University Hospital from January 1, 1994 to June 30, 2014 were enrolled in our study. Neonates included only those who were admitted in the neonatal intensive care unit for GIB with melena. Of the 63 melena cases, two cases of swallowing of maternal blood and one case of pulmonary hemorrhage were excluded, and finally the remaining 60 cases were enrolled.
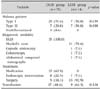
The patients were divided into UGIB and LGIB groups based on the bleeding sites at the ligament of Treitz. The patients with UGIB were classified into varices and PUD groups depending on the major causes. The patients with Meckel's diverticulum, which was the most common cause of LGIB, were classified as the third group. The melena patterns were differentiated as tarry black stool only or tarry black stool mixed with or preexisting fresh blood.
The medical records of the subjects, including their age, sex, melena pattern, laboratory findings, diagnostic modalities, cause of melena, therapeutic modality, and red cell transfusion, were retrospectively reviewed. All the laboratory results were applied with the values that were measured at the time when patients were hospitalized. Patients who had received blood transfusion before the test, or who suffered from an underlying disease such as liver diseases, renal diseases, dehydration, hematologic diseases, and oncology diseases, were excluded from the study. The study was approved by the institutional review board of Chungnam National University Hospital (IRB No. 2014-08-032).
The continuous variables were expressed as mean±standard deviation or median with range. The categorical variables were expressed as the number of case (percentage). Fisher's exact test was used for analyzing categorical variables. Mann-Whitney U test and Kruskal-Wallis test were used for analyzing continuous variables. Post-hoc comparison was performed when statistical significance was observed among the three disease groups. The BUN/Cr ratio was analyzed using univariate logistic regression, and the results were presented in odds ratios (OR) and their confidence intervals (95% CI). SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical processing. Statistical significance was accepted when the p-value was <0.05.
DISCUSSION
Our study was conducted to evaluate the BUN/Cr ratio, which has been known to be useful in distinguishing UGIB from LGIB, whether it was helpful in localizing bleeding site in cases with GIB presenting with melena, and also its differences in the three major melena diseases. The results showed that the BUN/Cr ratio and BUN/Cr ≥30 may be useful in differentiating UGIB from LGIB in cases with GIB presenting with melena. Particularly, the BUN/Cr ≥30 presented a significant OR of 6.9 in the UGIB than in the LGIB. However, the BUN/Cr ratio manifested a difference between the major causes of UGIB, varices and PUD, but there was no significant difference between PUD, the major cause of UGIB and Meckel's diverticulum, the most common cause of LGIB.
In previous studies, the BUN/Cr ratio has been reported as useful in localizing bleeding site in patients with GIB [
9,
10,
11,
12]. According to Felber et al. [
13], BUN/Cr ≥30 indicates UGIB, and <30 means UGIB or LGIB. In a study of children with GIB, the specificity and sensitivity of UGIB when BUN/Cr >30 were 98% and 68.8%, respectively [
10]. The BUN/Cr ratios were significantly different between UGIB and LGIB, and that in LGIB was lower than 30 [
11]. In our study, BUN/Cr >30 was observed in 17 cases (48.6%) in UGIB and in two cases (14.3%) in LGIB. In another study that targeted 125 adults with GIB, BUN/Cr >36 could imply UGIB, but the bleeding sites were hardly localized when the level was lower [
14]. In our study including only pediatric patients aged 1 day after birth to 18.0 years, the BUN/Cr ratio ranged from 10.8 to 124 (median 32.0) in the UGIB group, and from 10.4 to 35.4 (median 22.5) in the LGIB group, which was a significant difference. These results were consistent with those of previous studies, which suggested the usefulness of the BUN/Cr ratio and BUN/Cr >30 in differentiating UGIB from LGIB. However, the BUN/Cr ratio was significantly different between group with PUD ranged 13.5 to 38.1 (median 19) and group with varices ranged 17.6 to 124 (median 40.0), which are two major causes of UGIB presented with melena. These showed that the BUN/Cr ratio differs between the two major UGIB diseases. A BUN/Cr ≥30 was observed only in two cases of PUD group. This result can be attributed to the zero increase in the BUN/Cr ratio because melena may occur in a small amount of GIB in children with PUD. The BUN/Cr ratio in the Meckel's diverticulum group was lower than 30, which is consistent with the result of previous studies. In our study, there was no difference in the BUN/Cr ratio between the PUD group and Meckel's diverticulum group.
In the study of Cleveland et al. [
14] which included patients aged from birth to 17 year old with UGIB who underwent EGD, the major causes were prolapse gastropathy syndrome (12.7%), gastric erosions/ulcers (10.8%), erosive esophagitis (9.5%), duodenal erosions/ulcers (8.2%), and esophageal varices (6.3%). In other studies, the identified causes of UGIB were gastritis/erosion/ulcer (35.8%), duodenitis/duodenal ulcer (7.6%), and esophageal varices (7.2%) [
15]. In a study of Hassoon et al. [
16], the most common cause of UGIB was esophageal varices (39%), followed by gastric erosion/ulcers (29.3%), duodenal ulcer (7.4%), and esophagitis (4.9%). In our study, the 35 cases of UGIB included esophagogastric varices (35.1%), gastritis/gastric ulcer (16.2%), duodenitis/duodenal ulcer (21.6%), and esophagitis (5.4%). The incidence of variceal bleeding was similar to that of the study of Hassoon. In contrast, our study showed that LGIB accounted for 22.6% of all the melena cases, and the most common cause of melena was Meckel's diverticulum.
In children, the causes and incidence of GIB, which induce melena, differ according to age [
2]. A study of hospitalized children with GIB showed that the highest incidence was observed in the 11-15 years age range, and the lowest incidence was in those younger than 1 year old [
17]. In our study, the incidence of UGIB inducing melena was 29.7% in the 2-5 years age group, 27.0% in the >10 years age group, 21.6% in the 1 month to 1 year age group, and 13.5% and 8.1% in the 6-10 years and <1 month age groups, respectively. The highest incidence of LGIB was 42.9%, which was observed in the 6-10 years age group, and all the cases were induced by Meckel's diverticulum. Rafeey et al. [
15] showed that esophageal variceal bleeding was observed in 0.4% of the patients younger than 1 year, and in 6.7% of those older than 1 year. In another study, esophageal varices rarely developed in patients younger than 1 year old [
18]. In our study, variceal bleeding was observed in children aged 15 months to 4.3 years, and the youngest patient at 15 months had gastric varices bleeding caused by portal vein agenesis.
In variceal bleeding, the lymphocyte count was significantly higher than that in PUD and Meckel's diverticulum. This may be influenced by precedent viral infection with fever and cough in 53.8% of the cases of variceal bleeding.
Treatment of GIB patients with melena are customized according to the causes. In our study, all the PUD cases were treated with antacids, except two duodenal ulcer bleeding cases treated with endoscopic intervention and surgery. In the cases with vascular lesions, endoscopic variceal ligation or histoacryl injection was performed to control variceal bleeding, hemoclipping was used for treating Dieulafoy lesion, and snare polypectomy was performed for colon polyps. Surgical intervention was performed in all cases of Meckel's diverticulum, two duodenal ulcer cases, and a case of gastric arteriovenous malformation, a small bowel arteriovenous malformation, a gastrointestinal stromal tumor, and a huge duodenal polyp.
GIBs that cause melena in children usually stop spontaneously but sometimes become intense, repetitive or continuous, which means it can develop into a life-threatening problem [
2,
19]. Considering the limited hemodynamic reserve in younger patients, early assessments and restoration of hemodynamic stability are critical in the initial treatment [
19]. Transfusion improves deteriorated tissue perfusion, enhances the oxygen supply, and plays an important role in lifesaving [
18]. According to recent studies, the restrictive strategy of transfusion in acute UGIB at a 7 g/dL or lower hemoglobin level improved the patient outcomes more significantly than did the liberal strategy of transfusion at a 9 g/dL or lower level [
19]. The study of Sharma et al. [
20] on GIB patients who refused blood-derived products due to ethical or religious concerns showed that transfusion-free management could be effective and safe for patients who refuse transfusion. Nevertheless, these studies included only 18-year-old or older patients. No studies have been performed to evaluate the possibility of applying these strategy to children who have relatively less hemodynamic reserve than adults. In our study, transfusion was done on 51.7% of the cases. Of them, 50.1% of UGIB cases had variceal bleeding, and 88.9% of LGIB cases had Meckel's diverticulum. For the melena pattern, type II melena cases underwent transfusion more often than type I melena cases, but the difference was statistically insignificant. In the three major disease groups, 18.2% of PUD group underwent transfusion, which was significantly less than the variceal group (69.2%) and Meckel's diverticulum group (66.7%). Of the cases that received transfusion, 57.1% with hemoglobin <7 g/dL belonged to the recently suggested restrictive strategy group.
The present study has some limitations. It performed a retrospective small case study, the 11 undiagnosed cases may possibly result in a bias, and the BUN/Cr ratio was not classified by age.
In conclusion, the BUN/Cr ratio and BUN/Cr ≥30 were proved as useful parameters in distinguishing bleeding sites, i.e. UGIB or LGIB in cases of GIB presented with melena. However, the BUN/Cr ratio appeared differently uneven between two major causes of UGIB, varices and PUD. That of PUD was insignificantly different from the major cause of LGIB, Meckel's diverticulum. Further, the BUN/Cr ≥30 appeared significantly higher in the variceal group than in the PUD group, and no differences were observed between PUD and Mickel's diverticulum group. These imply that UGIB in children can act as a confounding variable because its causes are various compared with LGIB, and it can also induce melena depending on the transit in the gastrointestinal tract even in cases of small amount of gastric or duodenal bleeding. This study suggested that observant interpretations are necessary in applying BUN/Cr ≥30 for distinguishing UGIB from LGIB. Additional studies, including large-scale ones, are needed in the future.











 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download