Abstract
Purpose
Bile duct dilatation is a relatively common sonographic finding; nevertheless, its clinical significance in children is controversial because little research has been done in the area. Therefore, we investigated the natural course and clinical significance of biliary duct dilatation in children.
Methods
We performed a retrospective study of 181 children (range, 1-day-old to 17-year-old) in whom dilatation of the intrahepatic duct and/or common hepatic duct and/or common bile duct was detected by abdominal ultrasonography at the Severance Children's Hospital between November 2005 and March 2014. We reviewed and analyzed laboratory test results, clinical manifestations, and clinical course in these patients.
Results
Pediatric patients (n=181) were enrolled in the study and divided into two groups. The first group included 59 subjects, without definitive cause of bile duct dilatation, who did not require treatment; the second group included 122 subjects, with definitive cause of bile duct dilatation or underlying biliary disease, who did require treatment. In the first group, 24 patients (40.7%) showed spontaneous resolution of bile duct dilatation, 20 patients (33.9%) showed no change, and 15 patients (25.4%) were lost to follow-up. In the second group, 31 patients were diagnosed with choledochal cysts, and 91 patients presented with biliary tract dilatations due to secondary causes, such as gallbladder or liver disease, post-operative complications, or malignancy.
By convention, the upper normal limit for the diameter of the common bile duct, measured by ultrasound, is 7 mm [1234]. Although these criteria are generally accepted, what is considered normal bile duct diameter is somewhat controversial because of the vagueness of the age criteria and various conditions, such as previous cholecystectomy, drug treatment, and the imaging modality itself that can affect the diameter measurement [5]. The ease and convenience of ultrasonography have led to its increased use for abdominal examination; the increased use of abdominal ultrasound has led to more frequent observation of biliary dilatation. Although bile duct dilatation has become a common sonographic finding, the clinical significance of asymptomatic bile duct dilatation has been controversial; there has been little research in this area to provide sound guidelines. In adults, asymptomatic biliary dilatation should be carefully evaluated because of the possibility of malignancy [6]. However, the causes of bile duct dilatations in the pediatric population differ from those of adults, with a lower prevalence of malignancy and higher prevalence of congenital anomalies [7]. Ultrasonography is a very sensitive and specific technique for diagnosing biliary diseases, as demonstrated in several studies [89]. We hypothesize that patients with localized biliary dilatation have a higher probability for a benign clinical course and prognosis. The aim of this study was to identify the natural course and clinical significance of incidentally discovered biliary tract dilatations in pediatric patients with normal liver enzymes, by analyzing resolution rates, final diagnoses, sites of bile duct dilatations, patients' characteristics, and laboratory tests.
We retrospectively evaluated 181 patients aged 0-17 years with biliary tract dilatation (intrahepatic duct, common hepatic duct, and common bile duct dilatation) as shown by sonography performed between November 2005 and March 2014 at the Severance Children's Hospital (Seoul, Korea). Ultrasound was performed for a variety of signs and symptoms, such as vomiting, abdominal pain, abdominal mass, jaundice, and fever of unknown origin. Patients with established choledochal cysts who were referred from other hospitals were excluded. Patient age, site of the biliary tract dilatation, laboratory test results, ultrasound findings, follow-up duration, and dilatation resolution were analyzed. We divided patients with biliary tract dilatation into two groups: one group consisted of patients with primary ductal dilatation with normal laboratory and sonographic findings; the second group included patients with ductal dilatation secondary to other diseases. We used the following diagnostic criteria for this study: normal common bile duct diameter, measured by abdominal ultrasonography of neonates was <1 mm, infants <2-3.5 mm, older children <4 mm, adolescents, and adults <7 mm. Normal internal diameter of the common hepatic duct, measured by abdominal ultrasonography of infants was <2 mm, older children <3 mm, and children aged 12 to 16 years <4 mm [12]. Two experienced pediatric radiologists performed ultrasonography. We defined the resolution group as those who showed spontaneous resolution to normal bile duct diameter in follow-up ultrasounds, and the non-resolution group as those with persistent bile duct dilatation. We used K-test, Mann-Whitney test, and chi-square test for comparisons between groups. The Statistical Package for the Social Sciences (PASW Statistics ver. 18.0; IBM Co., Armonk, NY, USA) was used for all analyses.
Of 11,859 abdominal ultrasonography procedures that were carried out during the period, 181 cases satisfied the inclusion criterion of dilated duct(s); 11,678 cases did not fulfill the inclusion criterion and were excluded (Fig. 1). Twenty-five patients (13.8%) had a hepatobiliary surgical history, where the dilatations appeared to result from post-operative complications. Thirty-one patients (17.1%) had congenital anomalies, such as a choledochal cyst or anomalous pancreaticobiliary ductal union. Thirty patients (16.6%) had gallbladder disease, and 18 patients (9.9%) had liver disease (1 hepatitis B virus infection, 1 fibropolycystic liver disease, 16 nonspecific reactive hepatitis). Fourteen patients (7.7%) were diagnosed with pancreatitis, trauma, malignancy, or hemangioma. Four patients (2.2%) had cholestasis with jaundice (3 total parenteral nutrition induced cholestasis, 1 drug induced cholestasis). Fifty-nine patients (32.6%) showed primary ductal dilatation without any apparent cause (Table 1). Among the 59 patients with primary ductal dilatations, 44 patients (74.6%) underwent follow-up ultrasound scans, with a mean follow-up period of 28 months (range, 1-95 months). Fifteen patients (25.4%) were lost to follow-up. Twenty-four cases of primary ductal dilatation (40.7%) resolved gradually (these patients comprised the resolved group). In the remaining 20 cases, dilatations (33.9%) did not resolve until the last evaluation (median follow-up duration: 1 year 3 months; these patients comprised the non-resolved group) (Fig. 2). When we compared laboratory tests between the primary and secondary ductal dilatation groups, aspartate transaminase and alanine transaminase were significantly higher in the secondary ductal dilatation group (p<0.001; Table 2). However, this result might be biased due to the heterogeneity of the secondary ductal dilatation group. When we compared laboratory test results between the resolved group and the non-resolved group of the primary ductal dilatation patients, there were no significant differences. No predictive factor associated with resolution was observed in the primary ductal dilatation patients. Furthermore, when we investigated whether there could be a factor that was predictive of resolution, none was identified that showed a difference between the resolved group and the non-resolved group of primary ductal dilatation patients (Table 3). Comparison of the resolution rates depending on dilatation site was also conducted; patients with dilatations only in extrahepatic ducts showed the highest rate of resolution (45.8%) (Table 4). With respect to dilatation sites, we investigated the likelihood of being diagnosed with other diseases. We found that more patients with only extrahepatic duct dilatations belonged to the primary ductal dilatation group than the secondary ductal dilatation group (Table 5). All groups divided according to dilatation sites showed similar proportions of secondary ductal dilatations, but patients with only extrahepatic duct dilatation had the highest percentage of primary ductal dilatations. This difference was statistically significant when analyzed by chi square test (p<0.001).
Reported cases of dilatated biliary tracts (such as choledochal cyst or bile duct carcinoma) have a higher prevalence in Asia than Western countries [10]. Furthermore, the majority of patients who reported having choledochal cyst disease are children. In nationwide survey of Korean children, acquired biliary diseases and congenital hepatobiliary diseases were 7.6% and 12.6% of total hepatobiliary diseases respectively [11]. Therefore, it is important to define abnormal bile duct dilatation because of its possible association with congenital malformation and pathologic conditions, such as infection, calculi, biliary dysfunction, and malignancy [61213141516].
Ultrasonography is a useful method to evaluate the biliary tract system in children. It is rapid, noninvasive, and does not involve radiation exposure [17]. Although there have been several studies regarding bile duct measurement in children, no worldwide standards on range of normal size of biliary ducts in different pediatric age groups have been accepted [121819]. For this study, we applied Siegel's diagnostic criteria [20], where common bile duct dilatation was defined as a diameter greater than 2 mm, 4 mm, and 7 mm in patients 1 month, 12 years, and 16 years of age, respectively. Likewise, common hepatic duct dilatation was defined as a diameter greater than 2 mm, 3 mm, and 4 mm in patients 1 month, 12 years, and 16 years of age, respectively.
Bile duct dilatation can result from a variety of causes. The most common etiology is bile duct obstruction, which may present as acute abdominal pain and/or jaundice, and is revealed by an abnormal liver function test [212223]. In addition, there have been several reports on biliary duct dilatation as a post-operative change [242526]. Lee et al. [27] demonstrated that among 162 patients, 131 cases had anomalous biliary tract dilatations and 31 cases had non-anomalous biliary dilatations consisting of normal variants or resulting from secondary causes. Although we could not identify a standard diameter of the common bile duct that indicated the presence of possible causative lesions, we believe that a common bile duct diameter greater than 7 mm is an arbitrary standard that needs further evaluation, in order not to overlook significant biliary tract lesions [28].
Occasionally, we have observed biliary duct dilatation on abdominal sonography, which was not correlated with the patient's symptoms and laboratory test results. In adults, there have been only a few studies on the prognosis and outcome in asymptomatic patients with biliary tract dilatation and normal liver enzyme test results [4628]. However, there have been no reports regarding the causes of common bile duct dilatation in healthy pediatric populations, and no guidelines are available as to whether we should perform further study in those patients. Therefore, the aim of our study was to identify the clinical significance of asymptomatic bile duct dilatation and long-term outcome in pediatric patients.
In our study, 181 patients were enrolled and of these, 59 patients (32.6%) had no causative lesion, remained asymptomatic, and kept a benign course upon follow-up study. In addition, patients with only extrahepatic duct dilatation had the highest proportion (81.4%) of primary ductal dilatation and highest rate of resolution (45.8%). Our findings are inconsistent with previous adult studies. Jeon et al. [6] reported that patients with intrahepatic duct dilatation accounted for the majority of patients with normal laboratory test results and no causative lesions.
We hypothesized that patients with localized biliary dilatation have a higher probability for a benign course and prognosis, but that the outcome may depend on dilatation site. In patients with localized biliary dilatation, the biliary duct dilatation can occur because of a temporary bile flow disturbance. Additional research is necessary to prove this hypothesis.
In our study, 74% of patients with primary ductal dilatation showed spontaneous resolution or remained unchanged during the study interval. In these patients, no pathologic conditions emerged on ultrasonography during the follow-up period.
Our study had several limitations. First was its retrospective design: patients could not be investigated under the same conditions even in the absence of symptoms. Asymptomatic patients tended to be lost during follow-up according to patient's or doctor's preference, which might have contributed to bias in the information that was recorded. In addition, because sonography has become so easily accessible, the rate of incidentally found biliary dilatation has greatly increased. Because this study had a mean follow-up period of 28 months, a longer follow-up period is necessary to obtain long-term outcomes. Furthermore, even though experienced radiologists reviewed the results, bias could have resulted from subjectivity of the radiologist and the limitations of ultrasound technology. Therefore, additional investigations are needed to evaluate long-term prognosis and outcome, and to compare clinically relevant findings in patients with similar findings by endoscopic retrograde cholangiopancreatography or magnetic resonance cholangiopancreatography.
In conclusion, incidentally discovered biliary dilatation without any symptoms or abnormalities in laboratory and ultrasound tests in children could be defined as primary ductal dilatation and considered a non-pathologic condition. This condition was associated with a relatively benign clinical course and did not require medical intervention.
Figures and Tables
 | Fig. 2Distribution of study population, presumed cause of bile duct dilatation, and outcome of primary ductal dilatation on follow-up. Of 181 patients with ductal dilatations, 59 (32.6%) had primary ductal dilatations. |
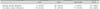
Table 2
Comparison of Demographic, Laboratory, and Sonographic Findings of Patients with Primary and Secondary Ductal Dilatations

References
1. Gore RM, Levine MS. Textbook of gastrointestinal radiology. Philadelphia: Elsevier;2015.
2. Brant WE, Helms CA. Fundamentals of diagnostic radiology. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health;2012.
3. Bowie JD. What is the upper limit of normal for the common bile duct on ultrasound: how much do you want it to be? Am J Gastroenterol. 2000; 95:897–900.

4. Oppong KW, Mitra V, Scott J, Anderson K, Charnley RM, Bonnington S, et al. Endoscopic ultrasound in patients with normal liver blood tests and unexplained dilatation of common bile duct and or pancreatic duct. Scand J Gastroenterol. 2014; 49:473–480.

5. Bruno M, Brizzi RF, Mezzabotta L, Carucci P, Elia C, Gaia S, et al. Unexplained common bile duct dilatation with normal serum liver enzymes: diagnostic yield of endoscopic ultrasound and follow-up of this condition. J Clin Gastroenterol. 2014; 48:e67–e70.
6. Jeon J, Song SY, Lee KT, Lee KH, Bae MH, Lee JK. Clinical significance and long-term outcome of incidentally found bile duct dilatation. Dig Dis Sci. 2013; 58:3293–3299.

7. Lin SF, Lee HC, Yeung CY, Jiang CB, Chan WT. Common bile duct dilatations in asymptomatic neonates: incidence and prognosis. Gastroenterol Res Pract. 2014; 2014:392562.

8. Gan SI, Rajan E, Adler DG, Baron TH, Anderson MA, Cash BD, et al. ASGE Standards of Practice Committee. Role of EUS. Gastrointest Endosc. 2007; 66:425–434.

9. Fernández-Esparrach G, Ginès A, Sánchez M, Pagés M, Pellisé M, Fernández-Cruz L, et al. Comparison of endoscopic ultrasonography and magnetic resonance cholangiopancreatography in the diagnosis of pancreatobiliary diseases: a prospective study. Am J Gastroenterol. 2007; 102:1632–1639.

10. Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL. Choledochal cyst disease. A changing pattern of presentation. Ann Surg. 1994; 220:644–652.

11. Park HJ, Shin CG, Moon JS, Lee CG. Analysis of hepatobiliary disorders from a nationwide survey ofdischarge data in Korean children and adolescents. Korean J Pediatr Gastroenterol Nutr. 2009; 12:16–22.

12. Zhang Y, Wang XL, Li SX, Bai YZ, Ren WD, Xie LM, et al. Ultrasonographic dimensions of the common bile duct in Chinese children: results of 343 cases. J Pediatr Surg. 2013; 48:1892–1896.

13. Douillet P, Brunelle F, Chaumont P, Valayer J, Sassoon C, Odièvre M. Ultrasonography and percutaneous cholangiography in children with dilated bile ducts. Report of six cases. Am J Dis Child. 1981; 135:131–133.

14. Arima E, Akita H. Congenital biliary tract dilatation and anomalous junction of the pancreatico-biliary ductal system. J Pediatr Surg. 1979; 14:9–15.

15. Büyükyavuz I, Karnak I, Haliloglu M, Senocak ME. Inflammatory myofibroblastic tumour of the extrahepatic bile ducts: an unusual cause of obstructive jaundice in children. Eur J Pediatr Surg. 2003; 13:421–424.

16. Tas A, Koklu S. Unusual cause of common bile duct dilatation in asymptomatic elderly patient: right hepatic artery syndrome. Ann Hepatol. 2012; 11:150–151.

17. Tahara K, Ishimaru Y, Fujino J, Suzuki M, Hatanaka M, Igarashi A, et al. Association of extrahepatic bile duct duplication with pancreaticobiliary maljunction and congenital biliary dilatation in children: a case report and literature review. Surg Today. 2013; 43:800–805.

18. McGahan JP, Phillips HE, Cox KL. Sonography of the normal pediatric gallbladder and biliary tract. Radiology. 1982; 144:873–875.

19. Hernanz-Schulman M, Ambrosino MM, Freeman PC, Quinn CB. Common bile duct in children: sonographic dimensions. Radiology. 1995; 195:193–195.

20. Siegel MJ. Liver and biliary tract. In : Siegel MJ, editor. Pediatric sonography. 2nd ed. New York: Raven Press;1995. p. 171.
21. Naji O, Hussain A, Baker D, Habib N, El-Hasani S. Obstructive jaundice due to autoimmune cholangiopathy. BMJ Case Rep. 2009; 2009.

22. Fumino S, Iwai N, Deguchi E, Shimadera S, Iwabuchi T, Nishimura T, et al. Bleeding tendency as a first symptom in children with congenital biliary dilatation. Eur J Pediatr Surg. 2007; 17:2–5.

23. Riederer J. Obstructive jaundice du to sludge in the common bile duct. Dtsch Med Wochenschr. 2000; 125:11–14.
24. Senturk S, Miroglu TC, Bilici A, Gumus H, Tekin RC, Ekici F, et al. Diameters of the common bile duct in adults and postcholecystectomy patients: a study with 64-slice CT. Eur J Radiol. 2012; 81:39–42.

25. Landry D, Tang A, Murphy-Lavallée J, Lepanto L, Billiard JS, Olivié D, et al. Dilatation of the bile duct in patients after cholecystectomy: a retrospective study. Can Assoc Radiol J. 2014; 65:29–34.

26. Daradkeh S, Tarawneh E, Al-Hadidy A. Factors affecting common bile duct diameter. Hepatogastroenterology. 2005; 52:1659–1661.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download