Abstract
In children presenting to hospital with gastrointestinal symptoms, diseases such as intussusception and acute appendicitis require particular attention and careful examination. Early diagnosis and proper treatment are important because of possible severe complications such as peritonitis and death. Intussusception and appendicitis share similar clinical manifestations. More importantly, the presence of acute appendicitis together with intussusception in children is very rare. We describe an interesting case of a 38-month-old boy who presented with abdominal pain in the right lower quadrant. His vital signs were stable and laboratory test findings showed no specific alterations. We detected tenderness in the right lower quadrant. A computed tomography scan showed an ileocolic intussusception with no strangulation and diffuse wall thickening of the appendix trapped within the intussusception. The patient underwent an appendectomy and manual reduction.
Children presenting to hospital with gastrointestinal symptoms, such as abdominal pain and vomiting, require supportive treatment. However, diseases such as intussusception and acute appendicitis require urgent attention and careful examination. If the diagnosis fails in the early stages, there is a strong possibility of severe complications such as peritonitis and death may occur [12]. Therefore, early diagnosis and proper treatment are required. Both intussusception and acute appendicitis are similar in their clinical manifestations, which include vomiting, abdominal pain, or irritability, but are distinguished by the different ages at which children are affected [34]. Thus, younger infants with severe irritability are generally suspected of intussusception and acute abdomen, while older children are more likely to be affected by acute appendicitis. In this report, we present an interesting case of intussusception with acute appendicitis.
A 38-month-old boy visited the emergency room with abdominal pain. He complained of abdominal pain in the right lower quadrant that began 2 days prior. The pain was described as colicky and intermittent, and it waxed and waned.
In the emergency room, his vital signs were stable (body temperature, 37.2℃; pulse rate, 98 beats/min; respiration rate, 20 breaths/min). He did not report vomiting or diarrhea. On physical examination, we found tenderness in the right lower quadrant and auscultation indicated a hypoactive bowel. We did not find any rebound tenderness or palpable mass in the abdomen. He complained of increased pain in the right lower quadrant with coughing (Dunphy's sign). Abdominal radiography and laboratory tests were performed. Abdominal radiography showed a mild generalized ileus (Fig. 1), and laboratory investigations revealed the following: hemoglobin, 11.0 g/dL; hematocrit, 39.5%; platelets, 229,000/mm3; white blood cell (WBC) count, 8,540/mm3 (WBC differential: neutrophils, 56.9%; monocytes, 2.7%; lymphocytes, 36.4%). Atypical lymphocytes were absent on peripheral blood smear. Liver function test results were normal, and high-sensitivity C-reactive protein was mildly elevated (1.95 mg/L, normal range: 0-1 mg/L). We suspected acute appendicitis and performed an abdominal and pelvic computed tomography (CT) that showed an ileocolic intussusception with no strangulation and diffuse wall thickening of the appendix trapped within the intussusceptions (Fig. 2).
At emergency surgery, the appendix was found to be inflamed and was completely trapped within the intussusception. An open appendectomy and manual reduction of intussusception were performed. The surgically resected appendix looked edematous and enlarged and histological evaluation showed an early inflammatory infiltration. Three days post-operation, gas was absent and the patient began oral feeding. Seven days later, he was discharged with no specific complications.
The peak incidence of the two conditions is different, with intussusception not common in children over 2 years and acute appendicitis rare in children under 3 years of age. In addition, the causes and symptoms are two distinct features of the disease; one disease may be overlooked if we suspect the other. Therefore, it is important to consider the possibility that both conditions may be present when making a diagnosis.
Intussusception is a major cause of intestinal obstruction in children. Intussusception occurs when one segment of the bowel and its associated mesentery invaginates into an adjacent segment. The cause of intussusception is idiopathic and most (90%) intussusceptions in children are of the ileocolic or ileocecal type [56]. The incidence of intussusceptions with leading points in pediatric cases is approximately 2-12%, with incidence increasing to 57% in patients over 4 years of age. The most common causes of a leading point are Meckel's diverticulum and Henoch-Schönlein purpura. Other causes include lymphoma, duplication, hemangioma, and polyps of the intestine [789]. Ganglioneuroma, adenomyomatous hamartoma, and heterotopic pancreas are rarely associated with an intussusception leading point or are accompanied by disease [101112]. In general, we do not investigate for the leading point because many cases of ileocolic intussusception in young infants are not associated with a leading point. Had we not considered the presence of an associated disease in our case, we would have only performed a simple reduction and excluded the diagnosis of appendicitis. Therefore, it is necessary to investigate for associated diseases when patients with intussusception visit the hospital.
Intussusception with appendicitis, such as in the case reported here is very rare in both pediatric patients and adults. Few cases have been reported since those described by Bevan [13] in 1957. Kang et al. [14] reported a cecocolic intussusception caused by appendicitis in a 73-year-old woman, which was diagnosed by abdominal and pelvic CT, and subjected to surgery. The intussusception resolved without manual reduction. Most of the causes of intussusception in adults are malignancies [15], although biopsies around the surgical site show no specific findings.
Appendicitis is a major surgical emergency in childhood. Appendicitis is caused by obstruction of the appendix by fecalith. In our case, we did not find, as would be expected in acute inflammatory diseases, elevated WBC counts or C-reactive protein, or presence of fever. Moreover, fecalith was absent in surgical gross findings. The causal relationship was not clear; however, we may consider that the appendicitis was triggered by intestinal obstruction owing to intussusception. Additional investigation is necessary to determine a causal relationship.
The characteristic symptoms of appendicitis include vomiting (96%), fever (85%), and right lower quadrant abdominal pain (81%) [16]. However, in children, the clinical presentation is atypical, and these same symptoms are also seen with intussusception, gastroenteritis, pneumonia, and many other diseases [17]. Thus, the diagnosis tends to be delayed with perforation rates higher than those observed in the general adult population [18].
Recently, diagnosis and surgical treatment of appendicitis have greatly improved. Appendicitis has generally been considered relatively easy to diagnose; therefore, we did not consider the possibility of applying a differential diagnosis for this case. However, Crohn's disease or intestinal tuberculosis adenocarcinoma are also causes of appendicitis, and numerous other diseases can mimic appendicitis as well. Thus, it is very important to always determine the cause and presence of any associated diseases. In our case, we used radiology and laboratory testing for diagnosis according to the general protocol when a disease is suspected. If we had diagnosed intussusception through ultrasound and performed air reduction only, complications of appendicitis may have occurred. However, we do not recommend performing computer tomography at the first suspicion of intussusception. Instead, it is important to use diagnostic ultrasound initially to attempt a differential diagnosis and consider other accompanying disorders.
Figures and Tables
Fig. 1
Abdominal radiograph. (A) Erect positon, (B) supine position. Abdominal radiograph showing a mild generalized ileus with no specific findings.
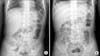
Fig. 2
Abdominal pelvic computed tomography. (A) Intussusceptions: ileocolic type intussusception without strangulation and significant obstruction (axial view, arrow). (B, C) Appendicitis: diffuse and mild wall thickening of the appendix partially trapped in the intussusception (B: axial view, C: coronal view; arrows).

References
1. McCollough M, Sharieff GQ. Abdominal surgical emergencies in infants and young children. Emerg Med Clin North Am. 2003; 21:909–935.

3. Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, Patel MM. Childhood intussusception: a literature review. PLoS One. 2013; 8:e68482.

4. Hardin DM Jr. Acute appendicitis: review and update. Am Fam Physician. 1999; 60:2027–2034.
5. Peyvasteh M, Askarpour S, Javaherizadeh H, Beigom Al-Taha B. Intussuception at atypical ages in children and adults--11 years experiences. Pol Przegl Chir. 2011; 83:304–309.
6. Cochran AA, Higgins GL 3rd, Strout TD. Intussusception in traditional pediatric, nontraditional pediatric, and adult patients. Am J Emerg Med. 2011; 29:523–527.

7. Ksia A, Mosbahi S, Brahim MB, Sahnoun L, Haggui B, Youssef SB, et al. Recurrent intussusception in children and infants. Afr J Paediatr Surg. 2013; 10:299–301.

8. Mills RW, McCrudden K, Gupta VK, Britton A, Al Qahtani M, Hasan RA. Intussusception caused by heterotopic pancreatic tissue in a child. Fetal Pediatr Pathol. 2011; 30:106–110.

9. Sonmez K, Turkyilmaz Z, Demirogullari B, Karabulut R, Kale N, Basaklar AC. Intussusception in children: experience with 105 patients in a department of paediatric surgery, Turkey. S Afr J Surg. 2012; 50:37–39.
10. Soccorso G, Puls F, Richards C, Pringle H, Nour S. A ganglioneuroma of the sigmoid colon presenting as leading point of intussusception in a child: a case report. J Pediatr Surg. 2009; 44:e17–e20.

11. Gal R, Kolkow Z, Nobel M. Adenomyomatous hamartoma of the small intestine: a rare cause of intussusception in an adult. Am J Gastroenterol. 1986; 81:1209–1211.
12. Gurbulak B, Kabul E, Dural C, Citlak G, Yanar H, Gulluoglu M, et al. Heterotopic pancreas as a leading point for small-bowel intussusception in a pregnant woman. JOP. 2007; 8:584–587.
14. Kang J, Lee KY, Sohn SK. Cecocolic intussusception in adult caused by acute appendicitis. Case Rep Surg. 2014; 2014:108327.

15. Lee CT, Lien WC, Wang HP, Lin BR, Huang PH, Lin JT. Primary appendiceal adenocarcinoma with cecocolic intussusception. J Gastroenterol Hepatol. 2006; 21:1079–1081.

16. Pepper VK, Stanfill AB, Pearl RH. Diagnosis and management of pediatric appendicitis, intussusception, and Meckel diverticulum. Surg Clin North Am. 2012; 92:505–526. vii

17. Mc Cabe K, Babl FE, Dalton S. Paediatric Research in Emergency Departments International Collaborative (PREDICT). Management of children with possible appendicitis: a survey of emergency physicians in Australia and New Zealand. Emerg Med Australas. 2014; 26:481–486.

18. Cheong LH, Emil S. Outcomes of pediatric appendicitis: an international comparison of the United States and Canada. JAMA Surg. 2014; 149:50–55.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download