Abstract
Purpose
Cholecystectomy is rarely performed in the child and adolescent. However, it is associated with several conditions. This study was conducted to describe the characteristics of pediatric patient who underwent cholecystectomy unrelated to hematologic disorders, and then to suggest its clinical significance in management by comparing a simple and complicated gallbladder disease.
Methods
We reviewed cases of cholecystectomy in pediatric patients (under 18 years old) at a single institution between January 2003 and October 2014. There were 143 cases during the study period and 24 were selected as the subject group.
Results
There were 7 male (29.2%) and 17 female (70.8%) patients. The mean age was 13.1 years old, and 66.6% of patients were older than 12 years. Mean body weight was 52.7 kg, and body mass index was 21.7 kg/m2, with 41.7% of patients being overweight or obese. We could identify a female predominance and high proportion of overweight or obesity in a complicated disease. There were also significantly increased levels of aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP) and bilirubin in this group. Most patients (87.5%) underwent laparoscopic cholecystectomy.
Conclusion
Cholecystectomy for diseases unrelated to hematologic disorders is rarely performed in the child and adolescent. In general, female patients who are overweight or obese, and those older than 12 years old, require laparoscopic cholecystectomy owing to multiple gallstones. This condition has a tendency to show a complicated gallbladder disease and significantly increased levels of AST, ALT, ALP, and bilirubin.
Cholecystectomy in children is relatively uncommon, despite being one of the most common surgical procedures in adults [123]. However, the number of cholecystectomy in children has increased over the past two decades [456]. A few studies on Western populations have demonstrated an increased rate of cholecystectomy in pediatric patients, and the most prevalent cause is a biliary dyskinesia [789]. Nonetheless, symptomatic gallbladder disease is due to gallstone in most pediatric patients.
The predisposing factors for the development of gallstone in pediatric patients differ slightly by age; prematurity, parenteral nutrition, abdominal surgery, or sepsis are factors in infancy, and hematologic disorders or obesity are factors in adolescence [10111213]. Among them, pediatric gallstones most frequently occurred in patients with hemolytic disorders [1415]. Recently, some reports have indicated that the proportion of hemolytic disease has decreased, and that of other conditions without hemolytic disease has increased [45], whereas idiopathic etiology is estimated between 20% and 65% [151617].
The estimated prevalence of gallstone in children in Western populations has been reported between 0.1% and 4.0%, but it has been reported as less than 0.13% in Japan [317].
In contrast to adult patients, pediatric patients with gallstone present with non-specific abdominal symptoms, and approximately 10-20% of these patients undergo cholecystectomy due to severe symptoms [1819202122].
The current study attempts to describe the characteristics of cases undergoing cholecystectomy due to disease unrelated to hematologic disorders in pediatric patients, and to suggest its clinical significance for managing it according to two different clinical situations; between a simple and complicated gallbladder disease.
We reviewed cases of cholecystectomy in pediatric patients (under 18 years old) at a single institution between January 2003 and October 2014. There were 143 cases during the study period. We excluded cases of cholecystectomy that were performed during other procedures for choledochal cyst, biliary atresia, and other hepatobiliary diseases, as well as hematologic disorders. Among these cases, 24 patients were selected as the subject group.
A retrospective study was conducted using patient's clinical data. We analyzed basic demographic characteristics such as sex, age, body weight, and body mass index (BMI), as well as clinical characteristics such as presented symptoms, preoperative diagnosis, laboratory and radiologic findings, associated conditions, and pathologic results. We divided subject as two clinical groups: group A, patients with simple gallbladder disease (ex. simple gallstone or gallbladder polyp) and group B, patients with complicated disease (ex. gallstone with choledocholithiasis or gallstone pancreatitis, with formation of pericholecystic abscess). Compared two clinical groups according to its clinical characteristics.
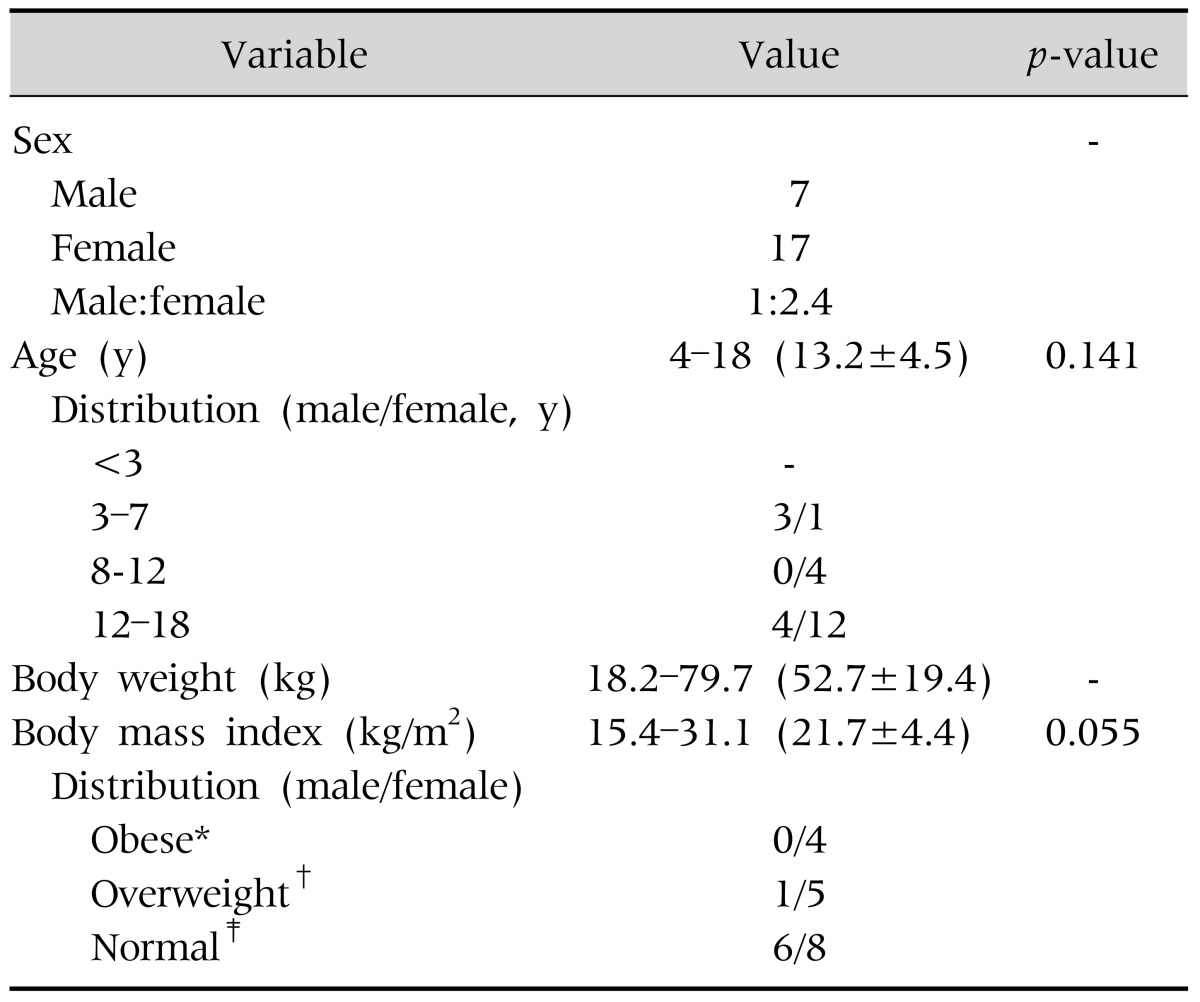
Among 24 patients, there were 7 male (29.2%) and 17 female (70.8%) patients. Mean age was 13.1 years old and 66.6% were older than 12 years. The mean body weight across all subjects was 52.7 kg, mean BMI was 21.7 kg/m2, and 41.7% of patients were obese or overweight. The proportion of obese and overweight patients was greater in female patients (52.9% in female and 14.3% in male patients). However there were no significant differences in these characteristics according to gender (Table 1).
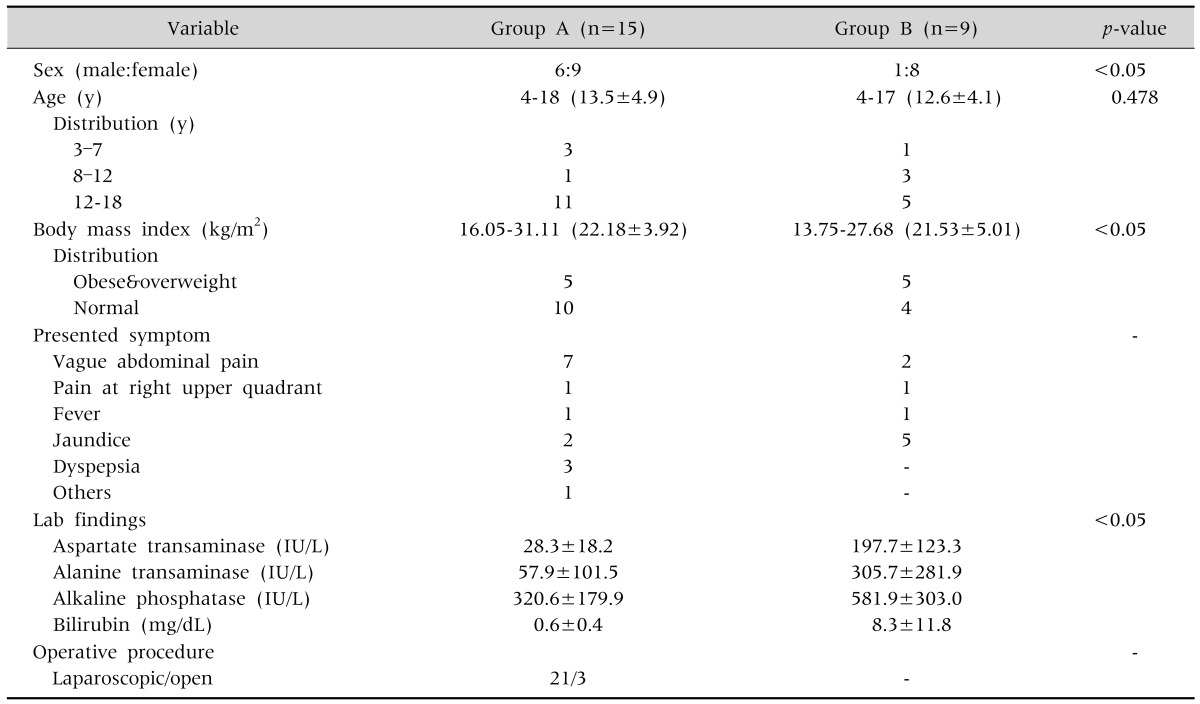
There were 15 (62.5%) patients in group A and 9 (37.5%) in group B. Most patients in group A had multiple stones, while patients in group B showed a combined choledocholithiasis in 7 patients, a gallstone pancreatitis in 2 patients. There was a gallbladder disease not associated with gallstone in each group, a gallbladder polyp and an acalculous pericholecystic abscess, respectively.
Composition of female patients was significantly higher in group B than A. There was no significant difference in the distribution of patient with regarding to age. Considering a BMI of patients, the proportion of overweight or obese patients was significantly higher in group B than group A (Table 2).
There was a variable presented symptom at admission, a vague abdominal pain was most common in group A and a jaundice in group B. Comparing liver function test between two groups, we identified significantly increased levels of aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP) and bilirubin in group B (Table 2).
Most patients (87.5%) underwent laparoscopic cholecystectomy. All patients with combined choledochalithiasis were managed by endoscopic retrograde cholangiopncreatography (ERCP) before cholecystectomy. There were no postoperative complications.
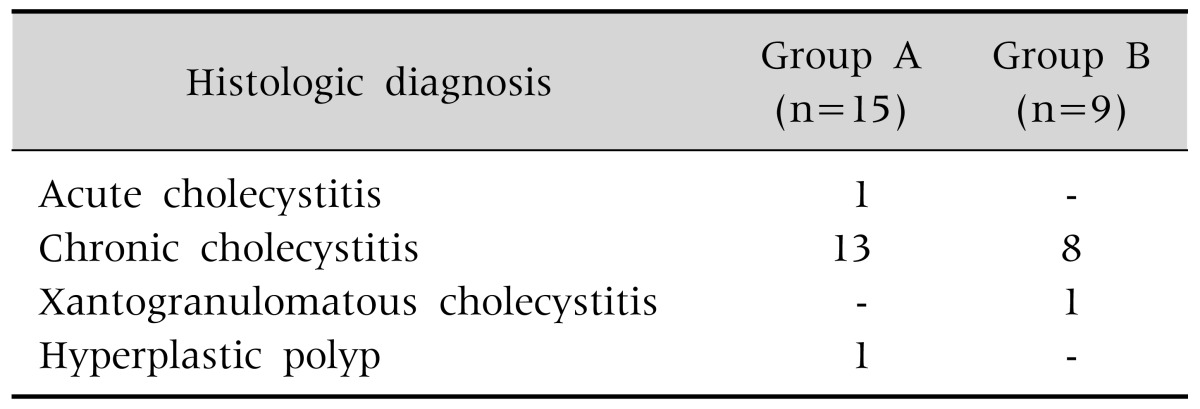
Postoperative diagnosis was confirmed by pathologic examination as follows: chronic or acute cholecystitis (22 cases), hyperplastic polyp (1 case), and xantogranulomatous cholecystitis (1 case) (Table 3).
Cholecystectomy is relatively rarely performed in pediatric populations, though it is extremely common in adults. Although we performed 143 cholecystectomies during the study period, there were only 24 cases for pure gallbladder problems unrelated to hematologic disorders. Recently, many studies have reported the increased prevalence of pediatric cholecystectomy due to gallstone disease in Western populations [456232425].
Our study also demonstrated that most cholecystectomies were due to gallstones (22/24, 91.7%). It was more common in female patients (70.8%) and adolescents (66.6%), with a mean age of 13.2 years. Considering certain risk factors (advanced age and female sex) for gallstone in adults [26], it may be assumed that these factors also affect the pediatric patients.
An idiopathic etiology of gallstone in the pediatric population has been proposed as between 20% and 65% [15242728], and certain predisposing factors have been suggested as follows: lithogenic interventions in neonatal period, such as long-term parenteral nutrition, a progressive increase in pediatric obesity, and recently, liberal use of ultrasonography [2930]. In this study, we did not evaluate the gallbladder disease in neonatal cholestasis because most of those cases did not need a surgical management. Ultrasonography is also widely used for monitoring gastroenterological and genitourinary conditions, and it has resulted in increased detection of asymptomatic gallstones, but we did not include those cases because it was generally microlithiasis without symptoms not requiring operation.
It is well known that there is an association between obesity and gallstone formation in adults, but this is now gaining recognition in the pediatric population [13313233]. Relative to adults, it is some difficult to accurately express a childhood obesity as BMI. This has led to inconsistency in result, Mehta et al. [5] reported a series of pediatric cases with 53% of nonhemolytic gallstone cases occurring in overweight or obese children/adolescents, whereas Bogue et al. [29] reported a series of cases with less than 1%. Our study showed not only a high proportion of obese and overweight patients (41.7%) in a complicated gallbladder disease, but also its significant relation to develop it. Although it is impossible to directly compare this proportion with the normal pediatric population, we could estimate that there is a relatively high rate of obesity or overweight in non-hemolytic gallstone cases. This problem seems to compound the presence of symptomatic gallstones, especially a complicated disease. Furthermore, considering the mean age at diagnosis, 13.2 years old, the high rate of obesity may also attributable to the rising incidence in that period.
Clinically, the pediatric population does not always present typical biliary colic symptoms, but rather, they often presented variable non-specific symptoms. However, when we examined the initial laboratory findings at admission, there were some differences. The levels of AST, ALT, ALP, and bilirubin were significantly higher in the group with complicated disease at admission, especially in cases accompanied by common bile duct stones. It may be possible that these highly increased levels suggest a combined choledocholithiasis in pediatric populations with gallbladder stones.
Gallstone may be presented by simple cholecystitis or a more complicated case combined with a biliary pancreatitis or choledocholithiasis causing jaundice. In this study, we could identify a gallstone pancreatitis in 8.3% and a choledocholithiasis in 29.2%. Generally, a choledocholithiasis is found in 8-10% of adult patients with cholelithiasis and between 10% and 15% in pediatric patients with gallstone, and the rate of gallstone pancreatitis has been reported as 7% [1529]. However, our study demonstrated higher incidence than those reports did. Although these patients were successfully managed by endoscopic sphincterotomy without complication, when considering a complication rate of 11% accompanied by ERCP in children and a high rate requiring a general anesthesia for procedure [3435], we should be aware of the possibility that these issues might occur more frequently when encountering or following up gallstone in pediatric populations. This study also revealed that significantly high frequency of complicated disease in female and overweight/obese patients, and so it may be suggested as aggravating factors to be considered in pediatric gallbladder disease, especially unrelated to hematologic disorders.
To manage gallbladder disease in pediatric populations, we performed laparoscopic cholecystectomy in 87.5% of cases and did not observe postoperative complications. Thus, the short-term outcome of cholecystectomy in pediatric population seems to be promising, but there may need more long-term drawbacks after removal of the gallbladder.
When comparing the histological results, most cases revealed chronic cholecystitis, but it did not seem to affect clinical characteristics.
There are some limitations in this study. It is result from the experience of single center and has relatively small subjects in certain regional area. Because it was retrospective study, could not compare with normal control group also. However considering a rare incidence of gallbladder disease unrelated to the hemolytic disorders in pediatric population, we feel that it may suggest clinical significance in managing pediatric gallbladder disease unrelated to hematologic disorders.
In conclusion, cholecystectomy is rarely performed in pediatric populations. Generally, a simple gallbladder disease is more common than complicated gallbladder disease unrelated to hematologic disorders. Female patients who are overweight or obese, or older than age 12 years require a laparoscopic cholecystectomy owing to multiple gallstones. Especially, the patient with a complicated gallbladder disease, such as a disease combined with choledochalithiasis or a gallstone pancreatitis, has a tendency to show such characteristics, and also significantly increased levels of AST, ALT, ALP, and bilirubin. It is necessary to consider these problems when managing cases of pediatric gallbladder disease, especially a gallstone unrelated to hematologic disorders.
References
1. Bailey PV, Connors RH, Tracy TF Jr, Sotelo-Avila C, Lewis JE, Weber TR. Changing spectrum of cholelithiasis and cholecystitis in infants and children. Am J Surg. 1989; 158:585–588. PMID: 2511775.

2. Kang JY, Ellis C, Majeed A, Hoare J, Tinto A, Williamson RC, et al. Gallstones--an increasing problem: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003; 17:561–569. PMID: 12622765.
3. Kratzer W, Mason RA, Kächele V. Prevalence of gallstones in sonographic surveys worldwide. J Clin Ultrasound. 1999; 27:1–7. PMID: 9888092.

4. Balaguer EJ, Price MR, Burd RS. National trends in the utilization of cholecystectomy in children. J Surg Res. 2006; 134:68–73. PMID: 16650434.

5. Mehta S, Lopez ME, Chumpitazi BP, Mazziotti MV, Brandt ML, Fishman DS. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics. 2012; 129:e82–e88. PMID: 22157135.

6. Waldhausen JH, Benjamin DR. Cholecystectomy is becoming an increasingly common operation in children. Am J Surg. 1999; 177:364–367. PMID: 10365870.

7. Kaye AJ, Jatla M, Mattei P, Kelly J, Nance ML. Use of laparoscopic cholecystectomy for biliary dyskinesia in the child. J Pediatr Surg. 2008; 43:1057–1059. PMID: 18558182.

8. Hofeldt M, Richmond B, Huffman K, Nestor J, Maxwell D. Laparoscopic cholecystectomy for treatment of biliary dyskinesia is safe and effective in the pediatric population. Am Surg. 2008; 74:1069–1072. PMID: 19062663.

9. Al-Homaidhi HS, Sukerek H, Klein M, Tolia V. Biliary dyskinesia in children. Pediatr Surg Int. 2002; 18:357–360. PMID: 12415355.

10. Whitington PF, Black DD. Cholelithiasis in premature infants treated with parenteral nutrition and furosemide. J Pediatr. 1980; 97:647–649. PMID: 6775066.

11. Roslyn JJ, Berquist WE, Pitt HA, Mann LL, Kangarloo H, DenBesten L, et al. Increased risk of gallstones in children receiving total parenteral nutrition. Pediatrics. 1983; 71:784–789. PMID: 6403918.

12. Shaffer EA. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep. 2005; 7:132–140. PMID: 15802102.

13. Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009; 9:322–329. PMID: 19560993.

14. Al-Salem AH, Qaisruddin S. The significance of biliary sludge in children with sickle cell disease. Pediatr Surg Int. 1998; 13:14–16. PMID: 9391196.

15. Wesdorp I, Bosman D, de Graaff A, Aronson D, van der Blij F, Taminiau J. Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr. 2000; 31:411–417. PMID: 11045839.

16. Palasciano G, Portincasa P, Vinciguerra V, Velardi A, Tardi S, Baldassarre G, et al. Gallstone prevalence and gallbladder volume in children and adolescents: an epidemiological ultrasonographic survey and relationship to body mass index. Am J Gastroenterol. 1989; 84:1378–1382. PMID: 2683739.
17. Nomura H, Kashiwagi S, Hayashi J, Kajiyama W, Ikematsu H, Noguchi A, et al. Prevalence of gallstone disease in a general population of Okinawa, Japan. Am J Epidemiol. 1988; 128:598–605. PMID: 3046339.

18. Angelico F, Del Ben M, Barbato A, Conti R, Urbinati G. Ten-year incidence and natural history of gallstone disease in a rural population of women in central Italy. The Rome Group for the Epidemiology and Prevention of Cholelithiasis (GREPCO). Ital J Gastroenterol Hepatol. 1997; 29:249–254. PMID: 9646217.
19. Zubler J, Markowski G, Yale S, Graham R, Rosenthal TC. Natural history of asymptomatic gallstones in family practice office practices. Arch Fam Med. 1998; 7:230–233. PMID: 9596456.

20. Attili AF, De Santis A, Capri R, Repice AM, Maselli S. The natural history of gallstones: the GREPCO experience. The GREPCO Group. Hepatology. 1995; 21:655–660. PMID: 7875663.
21. Friedman GD, Raviola CA, Fireman B. Prognosis of gallstones with mild or no symptoms: 25 years of follow-up in a health maintenance organization. J Clin Epidemiol. 1989; 42:127–136. PMID: 2918322.

22. McSherry CK, Ferstenberg H, Calhoun WF, Lahman E, Virshup M. The natural history of diagnosed gallstone disease in symptomatic and asymptomatic patients. Ann Surg. 1985; 202:59–63. PMID: 4015212.
23. Miltenburg DM, Schaffer R 3rd, Breslin T, Brandt ML. Changing indications for pediatric cholecystectomy. Pediatrics. 2000; 105:1250–1253. PMID: 10835065.

24. Kumar R, Nguyen K, Shun A. Gallstones and common bile duct calculi in infancy and childhood. Aust N Z J Surg. 2000; 70:188–191. PMID: 10765901.

25. Schweizer P, Lenz MP, Kirschner HJ. Pathogenesis and symptomatology of cholelithiasis in childhood. A prospective study. Dig Surg. 2000; 17:459–467. PMID: 11124549.
26. Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999; 117:632–639. PMID: 10464139.

27. Henschke CI, Teele RL. Cholelithiasis in children: recent observations. J Ultrasound Med. 1983; 2:481–484. PMID: 6644868.

28. Reif S, Sloven DG, Lebenthal E. Gallstones in children. Characterization by age, etiology, and outcome. Am J Dis Child. 1991; 145:105–108. PMID: 1898681.
29. Bogue CO, Murphy AJ, Gerstle JT, Moineddin R, Daneman A. Risk factors, complications, and outcomes of gallstones in children: a single-center review. J Pediatr Gastroenterol Nutr. 2010; 50:303–308. PMID: 20118803.

30. Khoo AK, Cartwright R, Berry S, Davenport M. Cholecystectomy in English children: evidence of an epidemic (1997-2012). J Pediatr Surg. 2014; 49:284–288. PMID: 24528968.

31. Holcomb GW Jr, Holcomb GW 3rd. Cholelithiasis in infants, children, and adolescents. Pediatr Rev. 1990; 11:268–274. PMID: 2408028.

32. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006; 295:1549–1555. PMID: 16595758.

33. Luo J, Hu FB. Time trends of obesity in pre-school children in China from 1989 to 1997. Int J Obes Relat Metab Disord. 2002; 26:553–558. PMID: 12075583.

34. Varadarajulu S, Wilcox CM, Hawes RH, Cotton PB. Technical outcomes and complications of ERCP in children. Gastrointest Endosc. 2004; 60:367–371. PMID: 15332025.

35. Metreweli C, So NM, Chu WC, Lam WW. Magnetic resonance cholangiography in children. Br J Radiol. 2004; 77:1059–1064. PMID: 15569653.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download