Abstract
We present a case of a 13-year-old boy with Gorham's disease involving the thoracic and lumbar spine, femur, and gastrointestinal (GI) tract, which was complicated by recurrent chylothorax and GI bleeding. The presenting symptoms were intermittent abdominal pain, back pain, and melena. Esophagogastroduodenoscopy and colonoscopy showed no abnormal lesions, but duodenal biopsy showed marked dilation of the lymphatics in the mucosa and submucosa, which revealed positive staining with a D2-40 immunohistochemical marker. In cases of GI bleeding with osteolysis, the expression of a D2-40 marker in the lymphatic endothelium of the GI tract may help to diagnose GI involvement in Gorham's disease. To the best of our knowledge, this is the first case report to pathologically demonstrate intestinal lymphatic malformation as a cause of GI bleeding in Gorham's disease.
Gorham's disease is a very rare disorder of uncertain etiology, characterized by non-neoplastic proliferation of vascular or lymphatic capillaries within bone and surrounding soft tissues, leading to resorption and replacement with angiomatous tissues [1]. Surrounding tissues such as muscles, connective tissues, and viscera may be affected. Chylous pericardial or pleural effusions and viscera involvement are associated with high morbidity and mortality [2,3]. In this report, we present a case of Gorham's disease involving the thoracic and lumbar spine, femur, and gastrointestinal (GI) tract complicated by recurrent chylothorax and GI bleeding. To the best of our knowledge, this is the first case report to confirm lymphatic or lymphovenous malformation as a cause of GI bleeding in Gorham's disease by demonstrating the expression of D2-40 and CD-31 stains in lymphatic and venous endothelium of the duodenum.
A 13-year-old boy presented with melena for 1 month. He had experienced intermittent abdominal pain and lower backache for 2 years. He defecated black-colored loose stools measuring about 50-100 mL once every 1-2 days. Abdominal pain was localized in the epigastric and periumbilical areas with no radiating pain, developed before and after eating, was reported as a mild to moderate dull pain, and lasted for about 30 min. Lower back pain worsened when sitting for long periods or reclining. He had no nausea, vomiting, diarrhea, pain on defecation, night symptoms, fever, weight loss, or other GI symptoms. His family history was non-contributory.
On physical examination, bowel sounds were normoactive and there was no tenderness, hepatosplenomegaly, or edema. His body weight was 38.1 kg (10-25th percentile), height 150.7 cm (25-50th percentile), body temperature 36.5℃, heart rate 90 beats/min, respiratory rate 25 breaths/min, and blood pressure 100/50 mmHg.
Laboratory data were as follows: hemoglobin 11.6 g/dL (normal: 13-17 g/dL), hematocrit 34% (normal: 37-47%), transferrin saturation 8% (normal: 15-50%), ferritin 11.9 ng/mL (normal: 7-140 ng/mL), serum total protein 4.6 g/dL (normal: 6.5-8.3 g/dL), and albumin 2.9 g/dL (normal: 4.0-5.3 g/dL). Serum electrolytes, blood urea nitrogen, creatinine, liver enzymes, and total cholesterol were unremarkable. The results of fecal occult blood testing were positive.
Initial radiographic examination revealed a lytic lesion eroding the L1-3 and T8-11 vertebrae. Magnetic resonance imaging (MRI) showed the osteolytic lesion to involve L1-3, T8-11, and both femur and soft tissue mass surrounding the left paraspinal space (Fig. 1). These osseous and soft tissue lesions were hypointense on T1-weighted images and hyperintense on T2-weighted images. The patient underwent computed tomography (CT)-guided biopsy of the paravertebral mass at the level of the L2 vertebra. Histological study showed that the mass was consistent with vascular proliferation and telangiectasia with hemosiderin deposition, which stained positively with D2-40 (Fig. 2). Gorham's disease was diagnosed after evaluation of the radiologic, pathologic, and clinical features.
Esophagogastroduodenoscopy, colonoscopy, and a Meckel's scan did not reveal any abnormal lesions. However, duodenal biopsy showed marked dilation of lymphatics in the mucosa and submucosa, which stained positively with D2-40 (Fig. 3). Some vessels showed ectatic change and stained positively with CD-31, which are characteristic of lymphatic or lymphovenous malformation. Double-balloon endoscopy revealed lesions of multiple red spots that caused bleeding in the terminal ileum and were managed by electrocoagulation.
During examination, the patient presented with dyspnea. A chest x-ray showed a left pleural effusion and a tube was inserted on the left side of the chest for drainage. The pleural fluid was chylous and drained at a rate of 0.9-1.2 L per day. Pleural biopsy revealed thin-walled vessels of various shapes and sizes lined by a single layer of endothelial cells, which stained positively with a D2-40 immunohistochemical stain (Fig. 4). Radioisotope lymphangiography was used to detect any abnormalities of the lymphatic system and thoracic duct, but no abnormal lesions were found.
After diagnosis of Gorham's disease, he was given symptomatic treatment: tube drainage for chylothorax and electrocoagulation for GI bleeding. His symptoms fluctuated. Abdominal pain and backache were milder than at initial evaluation but developed intermittently. The frequency of melena reduced to once every 2-4 weeks, persisting for 1 year. Both anemia and fecal occult blood continued for 3 years, after which his GI symptoms and anemia improved and his growth accelerated to a normal rate: height in the 50-75th percentile and weight in the 25-50th percentile.
Gorham's disease is a rare disorder characterized by osteolysis [1,4]. Histopathologically, normal bone is replaced by vascular lymphatic proliferation but not neoplastic proliferation [5,6]. In 1955, Gorham and Stout found patient with angiomatosis of the blood vessels and lymphatic vessels and named as Gorham's disease. Although the etiology and pathophysiology is still unknown, there are numerous published studies concerning pathologically non-neoplastic vascular tissue in Gorham's disease [7]. Neovascular tissue is characterized by proliferation of thin-walled, endothelial-lined capillaries and sinusoidal channels of lymphatic origin [8]. However, we believe that only a few studies have explored immunohistochemical staining with lymphovascular markers. In an attempt to investigate the invasion of lymphatic vessels, we used a D2-40 stain. Lymphatics are thin-walled, endothelium-lined channels devoid of red blood cells and a smooth muscle layer, but it is very difficult to distinguish morphologically normal lymphatic channels from venules or capillaries. Currently, the monoclonal antibody immunohistochemical stain, D2-40, is considered to be a highly sensitive and specific marker of the lymphatic endothelium [9]. To the best of our knowledge, our case report is the first to identify lymphatic endothelium at an abnormal paravertebral soft tissue mass and the duodenum in Gorham's disease.
Gorham's disease often produces periosseous soft tissue abnormalities that extend into the pulmonary, pleural, and solid abdominal organs [1,3]. In our case, the patient presented with history of melena, abdominal pain, and backache. Esophagogastroduodenoscopy and colonoscopy did not reveal any abnormal bleeding lesions but revealed expression of D2-40 with ectatic vessels of the duodenal mucosa and submucosa. Although suspected bleeding lesions were found by double-balloon endoscopy in the terminal ileum and managed by electrocoagulation, positive results in a fecal occult blood test and anemia continued for 3 years after electrocoagulation management, so we deduced that the GI bleeding had improved spontaneously, not by electrocoagulation.
Chylothorax and vertebral involvement in Gorham's disease are rare but usually fatal owing to progressive hypoproteinemia, malnutrition, and immunosuppression with lymphocytopenia [10]. Chylothorax results from lymphangiectasia, whereby lymph drains into the pleural cavity, or from leakage of chyle from a thoracic duct due to its invasion of a blockage [2]. Management of chylothorax in Gorham's disease includes radiotherapy as well as surgery, including thoracic duct ligation, pleurodesis, excision of vascular tissue, and medical therapy [2,11,12]. In this patient, there was no evidence of abnormal structures and sources of chylous leakage on radioisotope lymphangiography, so we performed pleurodesis using sodium tetradecyl sulfate.
The treatment of Gorham's disease is controversial and most cases of Gorham's disease resolve spontaneously. The surgical treatment of the affected bone resection, radiotherapy, and medical treatment using estrogens, magnesium, calcium, vitamin D, or bisphosphonate were attempted but their effect was uncertain [3,13].
Here, we described a case of GI involvement in Gorham's disease in a 13-year-old boy. GI involvement in Gorham's disease should be suspected in any patient who experiences GI bleeding with osteolysis. Histological findings of D2-40 in the lymphatic endothelium of the GI tract from biopsies may aid diagnosis.
Figures and Tables
Fig. 1
(A) Magnetic resonance imaging (MRI) of the spine. Hyperintense areas of the T- and L-vertebrae on a T2-weighted image showing multiple osteolytic lesions (white arrows). (B) MRI of the pelvis. Hyperintense areas of both femur metaphysis and diaphysis on a T2-weighted image showing multiple osteolytic lesions (white arrows). (C) MRI of paravertebral mass. Soft tissue mass surrounding a left paraspinal space at the level of the T-vertebrae (white arrows).
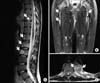
Fig. 2
(A) Biopsy specimen of a paravertebral mass showing lymphatic endothelial cells of various shapes and sizes, highlighted by D2-40 immunohistochemical stain (×400), (B) Biopsy specimen of a paravertebral mass showing lymphatic endothelial cells of various shapes and sizes, highlighted by D2-40 immunohistochemical stain (×400).

Fig. 3
(A) Irregularly dilated thin-walled lymphatics within the submucosa of the duodenum, which stain positively with D2-40 immunohistochemical stain (×400), (B) Irregularly dilated thin-walled lymphatics within the submucosa of the duodenum, which stain positively with D2-40 immunohistochemical stain (×400).
Fig. 4
Pleural biopsy revealed thin-walled vessels of various shapes and sizes lined by a single layer of endothelial cells. Amorphous eosinophilic material was found within the lumens and aggregates of lymphocytes were located in the vessels. Immunohistochemical staining with D2-40 identified lymphatic endothelial cells (×400).

References
1. Gorham LW, Stout AP. Massive osteolysis (acute spontaneous absorption of bone, phantom bone, disappearing bone); its relation to hemangiomatosis. J Bone Joint Surg Am. 1955; 37-A:985–1004.
2. Tie ML, Poland GA, Rosenow EC 3rd. Chylothorax in Gorham's syndrome. A common complication of a rare disease. Chest. 1994; 105:208–213.
4. Seok YK, Cho S, Lee E. Early surgical management of chylothorax complicated by Gorham's disease. Thorac Cardiovasc Surg. 2010; 58:492–493.

5. Devlin RD, Bone HG 3rd, Roodman GD. Interleukin-6: a potential mediator of the massive osteolysis in patients with Gorham-Stout disease. J Clin Endocrinol Metab. 1996; 81:1893–1897.

6. Pazzaglia UE, Andrini L, Bonato M, Leutner M. Pathology of disappearing bone disease: a case report with immunohistochemical study. Int Orthop. 1997; 21:303–307.

7. Hirayama T, Sabokbar A, Itonaga I, Watt-Smith S, Athanasou NA. Cellular and humoral mechanisms of osteoclast formation and bone resorption in Gorham-Stout disease. J Pathol. 2001; 195:624–630.

8. Heffez L, Doku HC, Carter BL, Feeney JE. Perspectives on massive osteolysis. Report of a case and review of the literature. Oral Surg Oral Med Oral Pathol. 1983; 55:331–343.
9. Fukunaga M. Expression of D2-40 in lymphatic endothelium of normal tissues and in vascular tumours. Histopathology. 2005; 46:396–402.

10. Fujiu K, Kanno R, Suzuki H, Nakamura N, Gotoh M. Chylothorax associated with massive osteolysis (Gorham's syndrome). Ann Thorac Surg. 2002; 73:1956–1957.
11. Swelstad MR, Frumiento C, Garry-McCoy A, Agni R, Weigel TL. Chylotamponade: an unusual presentation of Gorham's syndrome. Ann Thorac Surg. 2003; 75:1650–1652.

12. Shim YJ, Jung HJ, Lee KS, Lee EB, Lee JE, Park TI. A case of Gorham disease with chylothorax in a child treated by surgery and radiotherapy. Clin Pediatr Hematol Oncol. 2010; 17:209–212.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download