Abstract
Purpose
The spontaneous seroconversion rate of hepatitis B e antigen (HBeAg)-positive chronic hepatitis B (CHB) virus infection in children is lower than that in adults. However, few studies have investigated the rate of transition from the immune-tolerant to the early immune-clearance phase in children.
Methods
From February 2000 to August 2011, we enrolled 133 children aged <18 years who had visited the Department of Pediatrics, Kyungpook National University Hospital. All subjects were in the immune-tolerant phase of HBeAg-positive CHB virus infection. The estimated transition rate into the early immune-clearance phase was calculated using the Kaplan-Meier method.
Results
Among the 133 enrolled pediatric CHB virus infection patients in the HBeAg-positive immune-tolerant phase, only 21 children (15.8%) had converted to the early immune-clearance phase. The average age at entry into active hepatitis was 10.6±4.8 years. The incidence of transition from the immune-tolerant to the early immune-clearance phase in these children was 1.7 episodes/100 patient-years. When analyzed by age, the estimated transition rate was 4.6%, 7.1%, and 28.0% for patients aged <6, 6-12, >12 years, respectively.
The natural history of chronic hepatitis B (CHB) virus infection in children is influenced by the age at infection, geographic region, ethnicity, mode of infection, host immunologic response, viral genotype, and concurrent infection with other viruses [1]. Most hepatitis B virus (HBV) infections acquired during adulthood present as acute hepatitis and have low conversion rates (5-10%) to chronic hepatitis or becoming a hepatitis carrier. However, HBV infection in the perinatal period or early childhood usually progresses to chronic infection, with a significant proportion of chronically infected patients developing liver cirrhosis and hepatocellular carcinoma. In fact, it is reported that more than 90-95% of perinatal infections and 30% of infections in children aged <6 years result in chronic hepatitis [2].
According to studies of the natural history of CHB virus infection, the timing of hepatitis B e antigen (HBeAg) seroconversion varies from childhood to adulthood, and occurs markedly between the ages of 15 and 35 years [3]. In Asian countries, vertical transmission (from highly infectious mothers to their babies) is an important route for HBV infection. Most carrier mothers experience delayed seroconversion in their 30s and 40s [4]. Many studies have reported on the natural history of CHB virus infection, including HBeAg seroconversion, but studies on the transition from the immune-tolerant phase to the early immune-clearance phase are rare. Therefore, in the present study, we aimed to elucidate the timing of the transition from the immune-tolerant phase to the early immune-clearance phase in children with CHB virus infection.
From February 2000 to August 2011, we enrolled a total of 133 children aged <18 years who had visited the Department of Pediatrics, Kyungpook National University Hospital (KNUH). All of the enrolled subjects were in the immune-tolerant phase of CHB virus infection. This cohort study was approved by the institutional review board of KNUH (IRB No. KNUH 2013-04-057).
Patients were considered to be in the immune-tolerant phase of CHB virus infection when they exhibited positive results for hepatitis B surface antigen (HBsAg) and HBeAg, negative results for hepatitis B surface antibody (anti-HBs) and hepatitis B e antibody (anti-HBe), elevated HBV DNA titers for at least 6 months, and persistently normal serum aspartate transaminase (AST)/alanine aminotransferase (ALT) levels since birth.
Patients were excluded from the study if they showed high levels of ALT at the time of the hospital visit, were transferred from another hospital during treatment, were co-infected with other viruses, for example hepatitis C virus, Epstein-Barr virus, Cytomegalovirus etc. were immune-compromised hosts, had other known metabolic or immune disorders, or had decompensated liver diseases, or other causes of liver disease such as steatohepatitis.
During follow-up periods, serum HBeAg (by using a commercially available electrochemiluminescence immunoassay (ECLIA) method; Roche Diagnostics, Indianapolis, IN, USA), HBV DNA (by real-time polymerase chain reaction [PCR]; Roche COBAS AmpliPrep/Taq-Man96 real-time PCR assay; Roche Diagnostics, Mannheim, Germany; detection limit 12 IU·mL), and AST/ALT titers were monitored at intervals of 3-6 months until the occurrence of elevation of the AST/ALT levels. During follow-up period, children were regarded as being in the early immune-clearance phase if the elevation of the AST/ALT levels (>1.5 times of the upper limits of normal value) persisted for more than 6 months without any evidence of systemic infection, because nonspecific reactive hepatitis is not uncommon in such young children. No known specific evidence for systemic infection or other causes of liver disease were noted at the time of regarding immune-clearance phase.
Patients were monitored at shorter intervals of 1-3 months if the AST/ALT titers were elevated. Entry into the early immune-clearance phase was considered when AST/ALT titers were elevated to at least 1.5 times over the upper limits of normal for a period of at least 3 months. The period to onset of active hepatitis was analyzed. If HBeAg seroconversion (HBeAg clearance plus undetectable HBV DNA by real time PCR) occurs during follow-up at the end of the immune-clearance phase, its implications were analyzed.
Statistical analysis was conducted using SPSS Statistics 17.0 (SPSS Inc., Chicago, IL, USA). All values are expressed as the mean±standard deviation (SD). Between age groups, differences were analyzed using unpaired Student's t-tests for the comparison of continuous variables, and p-values of <0.05 were considered statistically significant. The estimated transition rate from the immune-tolerant phase to the early immune-clearance phase was calculated using the Kaplan-Meier method. The cumulative proportion of children transitioning to the early immune-clearance phase were evaluated with Wald statistics, which can correct wide confidence intervals.
A total of 133 children (78 male, 55 female; 1.4 : 1) were in the immune-tolerant phase were enrolled. At the time of their first visit, their mean age was 6.9±4.9 years (mean±SD; range, 0-14.5 years) (Table 1). There were no significant demographic differences between patients aged ≥6 years and those aged <6 years. Most patients (98.5%) had a maternal history of CHB virus infection, suggesting that they were infected by vertical transmission. The mean duration of observation since birth was 9.5 years (range, 1.3-18.0 years), should it be tracked since birth.
Transition to the early immune-clearance phase was observed in 21 of the 133 children (15.8%), including 13 males and 8 females (M : F, 1.6 : 1); no notable differences were observed between these male and female patients. The mean age at entry into the early immune-clearance phase was 10.6±4.8 years (range, 1.7-16.9 years). Among the 21 patients in the immune-clearance phase, spontaneous HBeAg seroconversion occurred in 2 patients, whereas 17 patients were treated with an antiviral agent such as lamivudine. The remaining 2 patients were lost to follow-up. During treatment, AST, ALT, HBeAg, anti-HBe, and HBV DNA titers were monitored every 3 months. Lamivudine treatment was continued for at least 1 additional year after the occurrence of HBeAg seroconversion.
Patients who entered the early immune-clearance phase were observed for 100 person-years during which they developed 1.7 events of active hepatitis. The remaining 112 children persisted in the immune-tolerant phase during 1,036 person-years of observation. The maximum follow-up period was 12 years (range, 1.3-18.0 years), should it be tracked since birth. None of the children dropped out of the study within 6 months of enrollment.
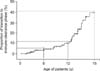
The proportion of patients transitioning to the early immune-clearance phase, as calculated by the Kaplan-Meier method, was estimated at 4.6% in the group aged <6 years, 11.7% in the group aged <12 years, and 39.7% in the group aged <18 years (Fig. 1). The transition proportion in the children aged 12-18 years (28.0%) was significantly higher than the transition proportion among patients aged <12 years (11.7%; p=0.001) (Fig. 2).
As of the time of writing, HBeAg seroconversion had occurred in 17 children among the 19 who entered the early immune-clearance phase, including the cases of spontaneous HBeAg seroconversion. In 13 of the 17 patients (76.5%), HBeAg seroconversion had occurred during a 4-year follow-up period. However, HBeAg seroconversion has not yet occurred in 2 of the 19 who converted to early immune-clearance, and these patients continue to receive treatment.
The rate of spontaneous HBeAg seroconversion has been reported to vary according to a patient's geographical region, age, and ethnicity. In Korea, Yoon et al. [5] reported that spontaneous HBeAg seroconversion occurred in 16% of adult patients with CHB virus infection annually. The rate of seroconversion in older patients was higher than that in younger patients. In comparison with the seroconversion rate in Asia, where HBV is highly endemic, Evans et al. [6] found a higher spontaneous HBeAg seroconversion rate in 454 chronic Asian-American carriers of HBV. They also found higher seroconversion rates among individuals aged 18-34 years (23%) than among those aged <18 years (15%). The major mode of HBV transmission may explain the low spontaneous seroconversion rate in Asia [7]. In Asia, HBV infection is endemic and usually transmitted by perinatal vertical transmission from mothers in a prolonged immune-tolerant phase of CHB virus infection. In addition, higher HBeAg seroconversion rates have been reported in horizontally infected children than in those infected perinatally [1].
The rate of spontaneous seroconversion is lower in children than in adults. In Taiwan, Chang et al. [8] reported that the annual HBeAg clearance rate was low (<2%) during the first 3 years of life but increased with age (4-5% in children aged >3 years and 10-14% for children aged 10-14 years). In Korea, Kim et al. [9] followed 214 children with CHB virus infection for 20 years and reported cumulative spontaneous HBeAg seroconversion rates of 8% for those aged <5 years, 11% for those aged <10 years, and 35% for those aged <19 years. Therefore, spontaneous HBeAg seroconversion occurred in approximately one-third of HBV-infected children, which is higher than previously reported [4]. These data are similar to our findings regarding the transition rates from the immune-tolerant phase to the early immune-clearance phase in different pediatric age groups. We observed the transition to the early immune-clearance phase in 21 (15.8%) of 133 children in the present study. Among these 21 patients, spontaneous HBeAg seroconversion occurred in 2 patients without treatment, and 17 patients were treated with an antiviral agent. The cumulative proportion of children transitioning to the early immune-clearance phase was estimated to be 11.7% in patients aged <12 years and 39.7% in patients aged <18 years.
Ethnicity has not been found to affect the HBeAg seroconversion rates between children and adults. Marx et al. [1] studied the long-term outcome of 174 HBeAg-positive children living in the United States who comprised a heterogeneous group with diverse ethnic origins. However, they reported a lower cumulative seroconversion rate in Asian-born children, predominantly vertically infected, as compared to all the other ethnic groups (75% vs. 94% by Kaplan-Meier analysis, p<0.05) after 13 years of follow-up.
As stated above, there are many published studies on the seroconversion rates that have used HBeAg seroconversion as the endpoint of the immune-clearance phase. From a clinical standpoint, it is more important to elucidate the time of conversion to active hepatitis, which is the early stage of the immune-clearance phase, to determine the optimal time to start treatment. However, there is little research covering this clinically significant turning point.
Although most CHB virus infection patients are asymptomatic, a long-term immune-clearance phase influences the development of complications such as liver cirrhosis. Because early management to shorten the duration of the immune-clearance phase is important for resolving hepatic inflammation, monitoring of liver function in immune-tolerant patients at regular intervals is necessary to detect the time of transition to the immune-clearance phase as early as possible. Many guidelines recommend that adult patients in the immune-tolerant phase should be monitored at intervals of 3 to 6 months [10,11,12]. In children, follow-up should be performed at least every 3 to 6 months, similarly to the follow-up guidelines for adults [13].
In the present study, we investigated the rate of transition to the immune-clearance phase according to age, in order to re-establish monitoring intervals. However, this study has several limitations. It is a retrospective cohort study of Korean children, in whom vertical transmission and genotype C are predominant [14]. We regarded CHB virus infection children with normal AST/ALT titers for at least 6 months as carrier in immune-tolerant phase since birth. This contention is based on assumption that conversion to the immune-clearance phase could occur only once in early life. The cutoff point of AST/ALT titers at 1.5 times over the upper limits of normal for defining entry to the early immune-clearance phase was determined arbitrarily. However, HBeAg seroconversion occurred in most children who transitioned to the early-clearance phase either spontaneously or with antiviral therapy [15,16,17,18].
Nevertheless, our report confirms that the transition rate to the immune-clearance phase is very low in children aged <12 years. Therefore, it may be advisable to extend the follow-up interval from the currently recommended 6-month follow-up interval for Korean children. Moreover, monitoring at 1-year intervals could be considered for children aged <6 years, in whom conducting short-term follow-up is not easy, since the transition rate in this age group was only 4.6%. However, further studies are needed to optimize follow-up intervals in children with CHB virus infection.
Figures and Tables
Fig. 1
Cumulative proportion of children transitioning from the immune-tolerant phase to the early immune-clearance phase analyzed using the Kaplan-Meier method (n=133).
ACKNOWLEDGEMENTS
The authors thank the World Congress of Pediatric Gastroenterology, Hepatology and Nutrition (WCPGHAN) for the 4th WCPGHAN Young Investigator Award and the European Society of Paediatric Gastroenterology, Hepatology and Nutrition International Award. This research was supported by Kyungpook National University Research Fund, 2012.
References
1. Marx G, Martin SR, Chicoine JF, Alvarez F. Long-term follow-up of chronic hepatitis B virus infection in children of different ethnic origins. J Infect Dis. 2002; 186:295–301.

2. McMahon BJ, Alward WL, Hall DB, Heyward WL, Bender TR, Francis DP, et al. Acute hepatitis B virus infection: relation of age to the clinical expression of disease and subsequent development of the carrier state. J Infect Dis. 1985; 151:599–603.

3. Chu CM. Natural history of chronic hepatitis B virus infection in adults with emphasis on the occurrence of cirrhosis and hepatocellular carcinoma. J Gastroenterol Hepatol. 2000; 15:Suppl. E25–E30.

4. Hsu YS, Chien RN, Yeh CT, Sheen IS, Chiou HY, Chu CM, et al. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology. 2002; 35:1522–1527.

5. Yoon JH, Rhee PL, Lee HS, Kim CY. Spontaneous HBeAg clearance rate and its affecting factors inpatients with chronic hepatitis B in Korea. Korean J Gastroenterol. 1992; 24:1313–1319.
6. Evans AA, Fine M, London WT. Spontaneous seroconversion in hepatitis B e antigen-positive chronic hepatitis B: implications for interferon therapy. J Infect Dis. 1997; 176:845–850.

7. Lok AS, Lai CL. A longitudinal follow-up of asymptomatic hepatitis B surface antigen-positive Chinese children. Hepatology. 1988; 8:1130–1133.

8. Chang MH, Sung JL, Lee CY, Chen CJ, Chen JS, Hsu HY, et al. Factors affecting clearance of hepatitis B e antigen in hepatitis B surface antigen carrier children. J Pediatr. 1989; 115:385–390.

9. Kim Y, Baek SY, Eom JH, Chung KS. Natural history of chronic hepatitis b in children. Korean J Pediatr. 2004; 47:282–289.
10. European Association for the Study of the Liver. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J Hepatol. 2012; 57:167–185.
11. Liaw YF, Kao JH, Piratvisuth T, Chan HLY, Chien RN, Liu CJ, et al. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2012 update. Hepatol Int. 2012; 6:531–561.

13. Shah U, Kelly D, Chang MH, Fujisawa T, Heller S, González-Peralta RP, et al. Management of chronic hepatitis B in children. J Pediatr Gastroenterol Nutr. 2009; 48:399–404.

14. Choe BH, Lee JH, Jang YC, Jang CH, Oh KW, Kwon S, et al. Long-term therapeutic efficacy of lamivudine compared with interferon-alpha in children with chronic hepatitis B: the younger the better. J Pediatr Gastroenterol Nutr. 2007; 44:92–98.

15. Bortolotti F, Jara P, Barbera C, Gregorio GV, Vegnente A, Zancan L, et al. Long term effect of alpha interferon in children with chronic hepatitis B. Gut. 2000; 46:715–718.

16. Fujisawa T, Komatsu H, Inui A, Sogo T, Miyagawa Y, Fujitsuka S, et al. Long-term outcome of chronic hepatitis B in adolescents or young adults in follow-up from childhood. J Pediatr Gastroenterol Nutr. 2000; 30:201–206.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download