Abstract
Purpose
Crigler-Najjar syndrome type II (CN-2) is characterized by moderate non-hemolytic unconjugated hyperbilirubinemia as a result of severe deficiency of bilirubin uridine diphosphate-glucuronosyltransferase (UGT1A1). The study investigated the mutation spectrum of UGT1A1 gene in Korean children with CN-2.
Methods
Five Korean CN-2 patients from five unrelated families and 50 healthy controls were enrolled. All five exons and flanking introns of the UGT1A1 gene were amplified by polymerase chain reaction (PCR) and the PCR products were directly sequenced.
Results
All children initially presented with neonatal jaundice and had persistent indirect hyperbilirubinemia. Homozygous p.Y486D was identified in all five patients. Three patients had an associated homozygous p.G71R and two a heterozygous p.G71R. The allele frequency of p.Y486D and p.G71R in healthy controls was 0 and 0.16, respectively. No significant difference in mean serum bilirubin levels was found between homozygous carriers of p.G71R and heterozygous carriers.
Hepatic glucuronidating activity is essential for efficient biliary excretion of bilirubin. Bilirubin glucuronidation is mediated by the enzyme bilirubin uridine diphosphate-glucuronosyltransferase (UGT1A1) [1]. UGT1A1 is encoded by five exons of the UGT1A1 gene. Defects in UGT1A1 cause a non-hemolytic unconjugated hyperbilirubinemia including Crigler-Najjar (CN) syndrome and Gilbert syndrome. CN syndrome is an autosomal recessive disease caused by mutations in UGT1A1 gene [2,3,4,5]. Genetic lesions causing an absence of enzymatic bilirubin glucuronidation result in CN syndrome type I (CN-1), whereas mutations causing incomplete deficiency of the enzyme result in CN syndrome type II (CN-2) [6]. CN-2 is characterized by intermediate levels of hyperbilirubinemia (7-20 mg/dL). In contrast to CN-1, kernicterus is rare and phenobarbital administration results in induction of the residual UGT1A1 activity with consequent reduction of serum bilirubin levels (>25%). CN-1 is caused by genetic changes that produce premature truncation or critical amino acid residue substitution. CN-2 results from substitution of single amino acid residues that markedly reduce, but do not abolish, enzyme activity [7].
Currently, the spectrum of mutations in Korean patients with CN-2 is not characterized. The aim of this study is to investigate the mutation spectrum of UGT1A1 gene in Korean children with CN-2.
Five Korean CN-2 patients (two males and three females) from five unrelated families were investigated. The median age was 10 years (range: 1-20 years). The diagnosis of CN-2 was based on intermediate levels of hyperbilirubinemia (7-20 mg/dL). The bilirubin was at least 90% unconjugated. Serum alanine aminotransferase and aspartate aminotransferase values were normal. Hemolysis was excluded on the basis of normal hemoglobin and reticulocyte counts. We also studied 50 healthy subjects with no known history of jaundice. This study was approved by the institutional review board of Seoul National University Hospital (IRB No. 1401-108-549). Informed consent was obtained from all of the patients' parents, and patient confidentiality was maintained.
Genomic DNA was extracted from peripheral blood leukocytes using the Wizard genomic DNA purification kit according to the manufacturer's instructions (Promega, Madison, WI, USA). All five exons and flanking introns of the UGT1A1 gene were amplified using polymerase chain reaction (PCR). PCR was performed using a thermal cycler (Applied Biosystems, Foster City, CA, USA). PCR products were purified and direct sequencing was performed using an ABI3100 Genetic Analyzer (Applied Biosystems). The sequences obtained were compared with the reference sequence NG_002601.2 registered in the National Center for Biotechnology Information database (http://www.ncbi.nlm.nih.gov).
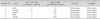
All children initially presented with neonatal jaundice requiring phototheray. The median age at the time of jaundice onset was 3 days of birth (range: 1-14 days) (Table 1). They had persistent indirect hyperbilirubinemia. Serum total bilirubin decreased with the administration of phenobarbital. Median follow up periods were 2 years (range: 1-17 years).
We identified a missense mutation (p.Y486D produced by the nucleotide substitution c.1456T>G in exon 5) and a polymorphism (p.G71R produced by the nucleotide substitution c.211G>A in exon 1). Homozygous p.Y486D was found in all five patients while p.Y486D was not found in healthy controls (p<0.01). Three patients had an associated homozygous p.G71R and two a heterozygous p.G71R. The allele frequency of p.G71R in CN-2 patients and controls was 0.88 and 0.16, respectively (p<0.01). No significant difference in mean serum bilirubin levels was found between homozygous carriers of p.G71R and heterozygous carriers.
This study presents the molecular characterization of UGT1A1 in Korean CN-2 patients. The homozygous p.Y486D missense mutation was observed in all five CN-2 patients. Four patients with CN-2 from Japan have been found to be homozygous for p.Y486D [8]. The p.Y486D mutation has also been reported in a Tunisian CN-2 patient [9]. Relative UGT1A1 activity of a homozygous p.Y486D expression model was 7.6% of the normal level [10]. Enzyme activity of a patient with CN-2 is generally less than 10% of normal level. Premature terminating mutations in UGT1A1 were more commonly observed among CN-1 patients, while missense mutations were more frequently associated with a CN-2 phenotype. This finding explains the milder phenotype observed in CN-2 and the inducibility of the residual enzyme activity by phenobarbital administration [7].
We found that all CN-2 patients had an associated homozygous or heterozygous p.G71R. Combination of homozygous p.Y486D and heterozygous p.G71R has been previously reported in a Taiwanese CN-2 patient [11]. A Japanese study revealed that three of the four CN-2 patients had an associated homozygous p.G71R [8]. It has been suggested that a homozygous p.Y486D associated with a homozygous or a heterozygous p.G71R always expresses CN-2 phenotypes in Asian populations.
In the present study, the allele frequency of p.G71R was 0.16 in healthy controls. p.G71R is considered as a polymorphism, which is any sequence variant present at a frequency >1% in a population. It has been reported that -c.3279T>G, TATA box, and p.G71R are three common polymorphisms in the Korean population, and that the allele frequency of p.G71R is 0.21. Serum bilirubin in homozygous carriers of p.G71R was reportedly significantly higher than those in heterozygous carriers or homozygous carriers of wild type allele [12]. A mutant expression model also showed that a heterozygous p.G71R and a homozygous p.G71R reduced transferase activity to 60% and 30% of the normal level, respectively [10]. Serum total bilirubin was markedly elevated when homozygous p.Y486D was present in combination with homozygous p.G71R [8]. In this study, no significant difference in serum bilirubin was found between homozygous carriers of p.G71R and heterozygous carriers. Further larger studies are helpful to investigate whether p.G71R additionally increases serum bilirubin level in homozygous p.Y486D carriers with CN-2. The p.G71R polymorphism has been identified as a risk factor for Gilbert syndrome [13,14] and neonatal breastfeeding jaundice [15,16] in East Asia.
In summary, the combination of homozygous p.Y486D and homozygous or heterozygous p.G71R is identified in CN-2 patients. The p.Y486D and p.G71R allele can be screened for the mutation analysis of UGT1A1 in Korea. Further larger genetic studies are needed to confirm our findings.
Figures and Tables
ACKNOWLEDGEMENTS
This study was supported by grant no. 0420071070 from the Seoul National University Hospital Research Fund.
References
1. Bosma PJ, Chowdhury JR, Bakker C, Gantla S, de Boer A, Oostra BA, et al. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert's syndrome. N Engl J Med. 1995; 333:1171–1175.

2. Bosma PJ, Chowdhury NR, Goldhoorn BG, Hofker MH, Oude Elferink RP, Jansen PL, et al. Sequence of exons and the flanking regions of human bilirubin-UDP-glucuronosyltransferase gene complex and identification of a genetic mutation in a patient with Crigler-Najjar syndrome, type I. Hepatology. 1992; 15:941–947.

3. Bosma PJ, Goldhoorn B, Oude Elferink RP, Sinaasappel M, Oostra BA, Jansen PL. A mutation in bilirubin uridine 5'-diphosphate-glucuronosyltransferase isoform 1 causing Crigler-Najjar syndrome type II. Gastroenterology. 1993; 105:216–220.

4. Ritter JK, Yeatman MT, Ferreira P, Owens IS. Identification of a genetic alteration in the code for bilirubin UDP-glucuronosyltransferase in the UGT1 gene complex of a Crigler-Najjar type I patient. J Clin Invest. 1992; 90:150–155.

5. Moghrabi N, Clarke DJ, Boxer M, Burchell B. Identification of an A-to-G missense mutation in exon 2 of the UGT1 gene complex that causes Crigler-Najjar syndrome type 2. Genomics. 1993; 18:171–173.

6. Seppen J, Bosma PJ, Goldhoorn BG, Bakker CT, Chowdhury JR, Chowdhury NR, et al. Discrimination between Crigler-Najjar type I and II by expression of mutant bilirubin uridine diphosphate-glucuronosyltransferase. J Clin Invest. 1994; 94:2385–2391.

7. Kadakol A, Ghosh SS, Sappal BS, Sharma G, Chowdhury JR, Chowdhury NR. Genetic lesions of bilirubin uridine-diphosphoglucuronate glucuronosyltransferase (UGT1A1) causing Crigler-Najjar and Gilbert syndromes: correlation of genotype to phenotype. Hum Mutat. 2000; 16:297–306.

8. Takeuchi K, Kobayashi Y, Tamaki S, Ishihara T, Maruo Y, Araki J, et al. Genetic polymorphisms of bilirubin uridine diphosphate-glucuronosyltransferase gene in Japanese patients with Crigler-Najjar syndrome or Gilbert's syndrome as well as in healthy Japanese subjects. J Gastroenterol Hepatol. 2004; 19:1023–1028.

9. Petit F, Gajdos V, Capel L, Parisot F, Myara A, Francoual J, et al. Crigler-Najjar type II syndrome may result from several types and combinations of mutations in the UGT1A1 gene. Clin Genet. 2006; 69:525–527.

10. Yamamoto K, Sato H, Fujiyama Y, Doida Y, Bamba T. Contribution of two missense mutations (G71R and Y486D) of the bilirubin UDP glycosyltransferase (UGT1A1) gene to phenotypes of Gilbert's syndrome and Crigler-Najjar syndrome type II. Biochim Biophys Acta. 1998; 1406:267–273.

11. Huang CS, Tan N, Yang SS, Sung YC, Huang MJ. Crigler-Najjar syndrome type 2. J Formos Med Assoc. 2006; 105:950–953.

12. Ki CS, Lee KA, Lee SY, Kim HJ, Cho SS, Park JH, et al. Haplotype structure of the UDP-glucuronosyltransferase 1A1 (UGT1A1) gene and its relationship to serum total bilirubin concentration in a male Korean population. Clin Chem. 2003; 49:2078–2081.

13. Aono S, Adachi Y, Uyama E, Yamada Y, Keino H, Nanno T, et al. Analysis of genes for bilirubin UDP-glucuronosyltransferase in Gilbert's syndrome. Lancet. 1995; 345:958–959.

14. Koiwai O, Nishizawa M, Hasada K, Aono S, Adachi Y, Mamiya N, et al. Gilbert's syndrome is caused by a heterozygous missense mutation in the gene for bilirubin UDP-glucuronosyltransferase. Hum Mol Genet. 1995; 4:1183–1186.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download