Abstract
Purpose
Choledochal cyst is a cystic dilatation of common bile duct. Although the etiology is presently uncertain, anomalous pancreaticobiliary ductal union (APBDU) is thought to be a major etiology of choledochal cyst. In this study, we analyzed the clinical and anatomical characteristics and pathologies of patients diagnosed with choledochal cyst in a single institute for 25 years.
Methods
A total of 113 patients, diagnosed with choledochal cyst and who received an operation in Severance Children's Hospital from January 1988 to May 2013, were included. Medical records were reviewed, including clinical and demographic data, surgical procedures. Abdominal ultrasonography, magnetic resonance cholangiopancreatography, and intraoperative cholangiography were used as diagnostic tools for evaluation and classification of choledochal cyst and the presence of anomalous pancreaticobiliary ductal union. Todani's classification, and relationship between APBDU and surgical pathology.
Results
Among 113 patients, 77 patients (68.1%) presented symptoms such as hepatitis, pancreatitis and/or cholecystitis. Eighty three patients (73.5%) had APBDU, and 94 patients (83.2%) showed inflammatory pathologic changes. APBDU, pathologic inflammation, and serological abnormalities such as hepatitis or pancreatitis showed a statistically significant correlation to one another.
Choledochal cyst, first described in 1723 by Vater and Ezler [1], is a cystic dilatation of the extra- and intrahepatic bile ducts that can cause various hepatobiliary and pancreatic disorders. Its incidence varies from 1 in 13,000 to 15,000 in Western countries, and is as high as 1 : 1,000 in Japan, which implies that the incidence is higher in Asian countries [2,3]. The incidence is 3.5 times higher in females than in males, which indicates strong female predilection [2,3]. In 1977, Todani et al. [4] classified choledochal cysts in different subtypes according to their shape, location, and extent of involvement. Among them, type I cysts account for 75-85% of cases [5].
In pathological findings, the cyst consists of fibrous wall with no epithelial lining of a low columnar epithelium having mild chronic inflammation [4,6,7,8,9]. In infants with choledochal cyst, complete inflammatory obstruction of the terminal portion of the common bile duct (CBD) is typical [7,8]. Additionally, the liver shows inflammatory changes in the large duct, and further, portal tract edema, bile ductular proliferation, and fibrosis may also be prominent [6,7,8,9]. However, it is usually not until adolescence that the biliary cirrhosis or carcinoma of cysts occurs [4,10,11].
Approximately two thirds of patients with choledochal cyst come to medical attention before the age of 10 years [12,13,14]. The classical triad of choledochal cyst is abdominal pain, jaundice, and a palpable abdominal mass, which is manifested in less than 20% of patients. In addition, in infants and younger patients, nonspecific symptoms such as vomiting, irritability, and failure to thrive are characteristic, which can lead to misdiagnosis [14,15].
Abdominal ultrasonography, endoscopic retrograde cholangiopancreatography or magnetic resonance cholangiopancreatography (MRCP), and operative cholangiography are used for diagnostic modalities, and the treatment of choice is surgical excision of the cyst with reconstruction of the extrahepatic biliary tree-hepaticojejunostomy with a Roux-en-Y anastomosis [14,16,17,18,19,20].
There is no established cause of choledochal cysts. However, several possible etiologies have been suggested by many researchers. One hypothesis is a congenital weakness of the bile duct wall [21]. During the developmental period of the embryonic duct, primary abnormality of epithelial proliferation has occurred that led to congenital weakness of the bile duct wall. The other possible cause is a congenital obstruction of bile ducts during the developmental period. To support this hypothesis, Yamashiro et al. [21] reviewed the anatomies of choledochal cysts, and they reported that anomalous junction between the CBD and pancreatic duct such as sphincter dysfunction, anomalous pancreaticobiliary ductal union (APBDU), and obstruction of distal choledochus was seen in 40% of patients. Although the etiology remains uncertain, APBDU is thought to be correlated with choledochal cyst [9,21]. In this article, we have retrospectively investigated medical records of patients who have been diagnosed with choledochal cyst and received an operation in our institution. From our study population, we were to confirm some previously-established facts, and most significantly, we were able to elucidate the relationship between APBDU and inflammatory changes in surgical pathology.
A total of 113 infants and children under the age of 18 years who were diagnosed with choledochal cyst and treated at Severance Children's Hospital, Seoul, Korea, from January 1988 to May 2013 were included in this study. We obtained the data retrospectively by reviewing the medical records. This study was approved by our institutional review board, and study protocol was in accordance with the Declaration of Helsinki.
This study was approved by our institutional review board (IRB No. 4-2014-0610), and study protocol was in accordance with the Declaration of Helsinki.
From the study population, we reviewed demographic data, presenting symptoms, diagnostic imaging modalities, surgical procedures, Todani's classification, intraoperative cholangiographies, surgical pathology, perioperative complications, and postoperative complications. The study population was subdivided into four age groups: infant and toddlers under 24 months of age, preschool children from 24 to 95 months of age, school-age children from 96 to 144 months of age, and adolescents. The defining characteristics from each of these age groups were reviewed, because we suggested that there should be significant differences among the age groups when APBDU was regarded as one of the major etiologies of acquired choledochal cyst [22,23].
Hepatitis was defined as an elevation in serum aspartate aminotransferase (AST) and serum alanine aminotransferase (ALT) levels. When an increase in ALT levels alone was observed, and no evidence of other reasons for these levels to be elevated was present, the presence of hepatitis was concluded. Cholangitis was defined as any symptom of the Charcot triad (abdominal pain, jaundice, and fever) with an increase in total bilirubin, AST, and ALT levels above the normal range, while pancreatitis was defined as a preoperative serum amylase or lipase level of more than threefold the normal upper limit. APBDU was defined as the anomalous union of the pancreaticobiliary duct system at a distance greater than 15 mm from the papilla of Vater [22].
Abdominal ultrasonography, MRCP, and intraoperative cholangiogram were performed to all the patients with choledochal cyst. After choledochal cyst was diagnosed through abdominal ultrasonography, MRCP and intraoperative cholangiogram were performed to confirm the presence of APBDU. Intraoperative cholangiogram was performed to all the patients diagnosed with choledochal cyst since abdominal ultrasonography and MRCP were considered to be insufficient to determine the presence and the type of APBDU. Most of APBDU cases were diagnosed prior to operation via abdominal ultrasonography or MRCP, but in some cases (7 out of 83 cases), the presence of APBDU was not confirmed until the intraoperative cholangiogram was performed.
Hepaticojejunostomy with a Roux-en-Y anastomosis, the treatment of choice, was performed for all the patients using an open surgery, laparoscopic approach, or Da Vinci Robotic surgery. Regular postoperative follow-up was performed after one, three, and six months post-surgery, and then annually when the patient showed no specific symptoms during the follow-up period. When the patient exhibited no complications within 3 years post-surgery, regular checkup in the outpatient clinic was terminated.
Statistical analysis was carried out in the Department of Biostatistics, Yonsei University College of Medicine. For the statistical analysis, PASW Statistics 18.0 (IBM Co., Armonk, NY, USA) was used. Chi-square test, exact test, Mann-Whitney U test, and Kruskal-Wallis test for parametric variables were used to evaluate the relationships between clinical characteristics, surgical pathologies, and APBDU. All tests were 2-sided with a 5% significance level.
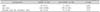
Among the 113 patients with choledochal cyst, there were 33 male (29.2%) and 80 female (70.8%) patients. Thirty-six patients (31.9%) were asymptomatic, while the remaining 77 patients (68.1%) manifested symptoms of hepatitis, cholecystitis, pancreatitis, or an incidence of two or more of these diseases. Moreover, more than half (76.6%) of symptomatic patients had hepatitis. Analysis of surgical pathology revealed that tissue with inflammatory change was shown in 94 patients (83.2%), whereas tissue with no inflammatory change was only seen in 19 patients (16.8%). On Todani's classification, there were 76 cases (67.2%) of type I choledochal cyst, with type Ic of 50 patients (44.2%), and the second most common type was type IVa choledochal cyst, with 28 cases (24.8%). Mean duration of laboratory data to normalization was 8.58 days, and 83 patients (73.5%) had APBDU (Table 1).
We have analyzed surgical pathologies in terms of age at diagnosis, gender, Todani's classification, duration until normalization of laboratory values, and presence of APBDU (Table 2). The median age of the subject base was 23.0 months; the median age of the group with inflammation was 23.5 months, while the median age of the group with no inflammation was 10.0 months. This showed no statistical significance between inflammation and age, with p=0.675. In gender and Todani's classification, we did not recognize any significant relationship with surgical pathology. We determined the duration of laboratory data to be normal according to different outcomes in surgical pathology. The median duration was consistently 8.0 days, both in the group with inflammation and in the group with no inflammation, with no statistical significance (p=0.430). Patients with APBDU constituted 83 (73.5%) of the 113 patients, and there were 73 (77.7%) APBDUs in the group with inflammation, while there were 10 (52.6%) cases in the group with no inflammation. This was statistically significant, with p=0.024. In the group with inflammation, there were 68 symptomatic patients (72.3%), while there were only 9 patients (47.4%) in the group with no inflammation, with statistical significance (p=0.033). The distribution of the cyst types in the two groups is shown in Fig. 1.
We analyzed by the presence of APBDU in terms of age, gender, Todani's classification, manifesting symptom, surgical pathology, and duration until normalization of laboratory values (Table 3). For the patients with APBDU, median age at diagnosis was 26.0 months, while non-APBDU patients were diagnosed at the median age of 2.5 months. This contrast was statistically significant (p=0.039). There was no significant relationship between genders (p=0.593). Patients with APBDU manifested pancreatitis more than non-APBDU patients, and the number of symptomatic patients with APBDU was 62 (74.7%), whereas the number among non-APBDU patients was 15 (50.0%). This contrast was statistically significant (p=0.013). Of the total patient base, 94 patients (83.2%) had inflammation in surgical pathology. In the APBDU group, 73 patients (88.0%) had inflammatory pathology, while there were 21 patients (70%) with such pathology in the non-APBDU group (p=0.024). The median duration of laboratory data to the normal value in APBDU patients was 8.0 days, while it was 7.0 days in non-APBDU patients (p=0.137). The distribution of cyst types in the two groups is shown in Fig. 2.
Finally, we considered the relationship between the age of initial diagnosis and the gender, symptoms, presence of APBDU or inflammatory changes, and duration of the normalization of laboratory values (Table 4). We have classified age groups into ages under 23 months, from 24 to 95 months, from 96 to 143 months, and above 144 months. This classification was based upon the age of infancy and early childhood, preschool age, school age, and adolescence. There were 58 patients aged 23 months or less, and 40 patients of preschool age. The numbers of school-age patients and adolescent patients were 6 and 9, respectively. Most patients (n=98, 86.7%) were diagnosed with choledochal cyst before the age of 95 months, and a total of 92% of patients were diagnosed with choledochal cyst before the age of 144 months. Symptomatic patients and the presence of APBDU were statistically significant among the age groups, with the p=0.005 and p=0.011, respectively.
The etiology of choledochal cyst is not yet certain, but APBDU is suggested as a major etiology of choledochal cyst [9,21,24]. In this study, we have reviewed medical records of pediatric patients with choledochal cyst for 25 years in a single institution, and we have attempted to enhance the state of knowledge concerning the characteristics of choledochal cyst and its correlation with numerous factors including age at diagnosis, symptoms, classifications, surgical pathology, and presence of APBDU.
Similar to prior studies, the sex ratio in our study group had a 1 : 2.1 male-to-female ratio, which shows female prevalence [25,26]. In addition, when we classified its subtypes by Todani's classidication, the incidence of type I was very high, with type Ic being the most common. Secondarily, type IVa was the second most common type, which is in agreement with prior studies [25,26]. Inflammation was pathologically confirmed in 94 patients (83.2%) out of 113 patients, and among these, APBDU was also present in in 73 patients (77.7%), which implies a strong connection between inflammatory changes and the presence of APBDU (p=0.024). Among the groups with inflammatory changes in their surgical pathology, 68 patients (72.3%) were symptomatic, while there were 9 patients (47.4%) in the non-inflammatory group (p=0.033). With statistical significance identified, this supports the suggestion that APBDU and symptoms such as hepatitis, pancreatitis, or cholecystitis are strongly related to the inflammatory changes of choledochal cyst. The factors of age, gender and Todani's classification showed no statistically significant relations with inflammatory changes of choledochal cyst.
Furthermore, we found that 92% of total patients were diagnosed at an age under 144 months. In the comparison between surgical pathology and age groups, inflammation was most commonly seen in the age group of 24 to 95 months (90%), compared with infants and adolescents. It can be said that the incidence of inflammation during infancy was less than that of early childhood, because the incidence of antenatal diagnosis via ultrasonography at birth was 26 cases (44.8%) of all of the patients under 23 months of age. Since diagnosis occurred early in the patient's life, there was less chance for inflammatory changes to occur. On the other hand, in the school-age and adolescent populations, fewer inflammatory changes were observed than in preschool children. In these populations, there were fewer symptomatic patients than in preschool children, which can explain the concomitant presence of fewer inflammatory changes in those populations. Another explanation is that the number of the age group in our study population was too small to draw adequate results. However, the reasons why there were fewer inflammatory changes in school age and adolescent groups requires additional study to determine the cause of this phenomenon.
We had suspected, prior to this study, that the preoperative laboratory findings would be related to the severity of inflammation. Therefore, we investigated the relationship between the presence of inflammation in surgical pathology and the duration that the preoperative laboratory values were normalized after the operation. However, it showed no statistical significance. The serological change, after all, results from the structure of the choledochal cyst and from acute inflammation, which can lead to the conclusion that the normalization of laboratory values will be more related to the outcome of the surgical procedure than to the severity of inflammation.
As mentioned previously, APBDU has been suggested as one of the etiologies of choledochal cyst [9,21,22,24]. An anomalous ductal union of CBD and pancreatic duct induces regurgitation of panceatic juice into the CBD, brings damage to the ductal wall by recurrent cholangitis, and results in cystic changes in the bile duct [22,23,24,25,26,27,28,29]. In 1988, Oguchi et al. [30] published an article stating that the choledochal cyst induced from APBDU shows more diffuse dilatation of duct, and that cystic dilatation of bile duct would be induced not only from APBDU but combined with other obstructive mechanisms such as an obstruction of distal choledochus. Many researchers have confirmed that the presence of APBDU cases influx pancreatic juice into the bile duct, and eventually, induces ductular dilatation along with the distal stenosis or elevation of intraductular pressure. Even when the congenital diliary dilatation is present with APBDU, the condition of choledochal cyst would be modified secondarily by stenosis of the distal bile duct or influx of pancreatic juice into the bile duct [30]. In our study, the median age of APBDU patients was 26.0 months, whereas the median age of non-APBDU patients was 2.5 months, and this difference was statistically significant (p=0.039). This supports the previously suggested hypothesis about APBDU as a major etiology of acquired choledochal cyst [9,23].
We have focused on characteristics of choledochal cyst with APBDU, and on the fact that patients with APBDU showed more inflammation on surgical pathology [29]. In the subject base with APBDU, there were 62 patients (74.7%) who showed serological abnormality such as hepatitis, cholangitis or pancreatitis, while there were 13 patients (43.3%) with serological abnormality in the non-APBDU group (p=0.013). Moreover, the number of patients with pathologically-confirmed inflammation was larger in the APBDU group than in the non-APBDU group, with statistical significance (p=0.024). From these results, we can conclude that there is a stong connection between APBDU, serologic abnormalities, and pathologic inflammatory changes.
Some literature has suggested that APBDU in choledochal cyst was strongly related to the inflammtory changes in the duct and periductular structure, but our study is the first to clarify the statistical relationship between APBDU and surgical pathology. Since this study was performed in a single institute using exclusively pediatric patients, a multi-centered study will be required to confirm the results we have obtained, in order to further the state of knowledge about this disease process.
Figures and Tables
Fig. 1
Distribution of the cyst types by Todani's classification in inflammatory and non-inflammatory group.

Fig. 2
Distribution of the cyst types by Todani's classification in anomalous pancreaticobiliary ductal union (APBDU) and non-APBDU group.

References
1. Vater A, Ezler CS. Dissertatio de Scirrhis viscerum occasione sectionis viri tympanite defunte. Wittenburgae. 1723; 881:22.
2. Gigot JF, Nagorney DM, Farnell MB, Moir C, Ilstrup D. Bile duct cysts: a changing spectrum of presentation. J Hepatobiliary Pancreat Sci. 1996; 3:405–411.

3. Lipsett PA, Pitt HA. Surgical treatment of choledochal cysts. J Hepatobiliary Pancreat Surg. 2003; 10:352–359.

4. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977; 134:263–269.
5. Yamaguchi M. Congenital choledochal cyst. Analysis of 1,433 patients in the Japanese literature. Am J Surg. 1980; 140:653–657.
6. Khandelwal C, Anand U, Kumar B, Priyadarshi RN. Diagnosis and management of choledochal cysts. Indian J Surg. 2012; 74:29–34.

7. Burnweit CA, Birken GA, Heiss K. The management of choledochal cysts in the newborn. Pediatr Surg Int. 1996; 11:130–133.

8. Casaccia G, Bilancioni E, Nahom A, Trucchi A, Aite L, Marcellini M, et al. Cystic anomalies of biliary tree in the fetus: is it possible to make a more specific prenatal diagnosis? J Pediatr Surg. 2002; 37:1191–1194.

9. Babbitt DP. Congenital choledochal cysts: new etiological concept based on anomalous relationships of the common bile duct and pancreatic bulb. Ann Radiol (Paris). 1969; 12:231–240.
10. Tsuchiya R, Harada N, Ito T, Furukawa M, Yoshihiro I. Malignant tumors in choledochal cysts. Ann Surg. 1977; 186:22–28.

12. She WH, Chung HY, Lan LC, Wong KK, Saing H, Tam PK. Management of choledochal cyst: 30 years of experience and results in a single center. J Pediatr Surg. 2009; 44:2307–2311.

13. Liu CL, Fan ST, Lo CM, Lam CM, Poon RT, Wong J. Choledochal cysts in adults. Arch Surg. 2002; 137:465–468.

15. Metcalfe MS, Wemyss-Holden SA, Maddern GJ. Management dilemmas with choledochal cysts. Arch Surg. 2003; 138:333–339.

16. Lee HC, Yeung CY, Chang PY, Sheu JC, Wang NL. Dilatation of the biliary tree in children: sonographic diagnosis and its clinical significance. J Ultrasound Med. 2000; 19:177–182.

17. Govil S, Justus A, Korah I, Perakath A, Zachariah N, Sen S. Choledochal cysts: evaluation with MR cholangiography. Abdom Imaging. 1998; 23:616–619.

18. Chijiiwa K, Koga A. Surgical management and long-term follow-up of patients with choledochal cysts. Am J Surg. 1993; 165:238–242.

19. Pietrabissa A, Boggi U, Di Candio G, Giulianotti PC, Sartoni G, Mosca F. Unsuspected choledochal cyst during laparoscopic cholecystectomy. Surg Endosc. 1995; 9:1127–1129.

20. Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 2 of 3: diagnosis. Can J Surg. 2009; 52:506–511.
21. Yamashiro Y, Sato M, Shimizu T, Oguchi S, Miyano T. How great is the incidence of truly congenital common bile duct dilatation? J Pediatr Surg. 1993; 28:622–625.

22. Kamisawa T, Ando H, Hamada Y, Fujii H, Koshinaga T, Urushihara N, et al. Japanese Study Group on Pancreaticobiliary Maljunction. Diagnostic criteria for pancreaticobiliary maljunction 2013. J Hepatobiliary Pancreat Sci. 2014; 21:159–161.

23. Han SJ, Hwang EH, Chung KS, Kim MJ, Kim H. Acquired choledochal cyst from anomalous pancreatobiliary duct union. J Pediatr Surg. 1997; 32:1735–1738.

24. Babbitt DP, Starshak RJ, Clemett AR. Choledochal cyst: a concept of etiology. Am J Roentgenol Radium Ther Nucl Med. 1973; 119:57–62.

25. O'Neill JA Jr, Templeton JM Jr, Schnaufer L, Bishop HC, Ziegler MM, Ross AJ 3rd. Recent experience with choledochal cyst. Ann Surg. 1987; 205:533–540.
26. Sela-Herman S, Scharschmidt BF. Choledochal cyst, a disease for all ages. Lancet. 1996; 347:779.

27. Alonso-Lej F, Rever WB Jr, Pessango DJ. Congenital choledochal cyst, with a report of 2, and an analysis of 94, cases. Int Abstr Surg. 1959; 108:1–30.
28. Büyükyavuz I, Ekinci S, Ciftçi AO, Karnak I, Senocak ME, Tanyel FC, et al. A retrospective study of choledochal cyst: clinical presentation, diagnosis and treatment. Turk J Pediatr. 2003; 45:321–325.
29. Song HK, Kim MH, Myung SJ, Lee SK, Kim HJ, Yoo KS, et al. Choledochal cyst associated the with anomalous union of pancreaticobiliary duct (AUPBD) has a more grave clinical course than choledochal cyst alone. Korean J Intern Med. 1999; 14:1–8.

30. Oguchi Y, Okada A, Nakamura T, Okumura K, Miyata M, Nakao K, et al. Histopathologic studies of congenital dilatation of the bile duct as related to an anomalous junction of the pancreaticobiliary ductal system: clinical and experimental studies. Surgery. 1988; 103:168–173.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download