Abstract
Infection-induced acute hepatitis complicated with acute pancreatitis is associated with hepatitis A virus, hepatitis B virus or hepatitis E virus. Although rare, Epstein-Barr virus (EBV) infection should be considered also in the differential diagnosis if the patient has acute hepatitis combined with pancreatitis. We report a case of EBV infection with cholestatic hepatitis and pancreatitis with review of literature. An 11-year-old female was admitted due to 1-day history of abdominal pain and vomiting without any clinical symptoms of infectious mononucleosis. Diagnosis of reactivated EBV infection was made by the positive result of viral capsid antigen (VCA) IgM, VCA IgG, Epstein-Barr nuclear antigen and heterophile antibody test. We performed serologic tests and magnetic resonance cholangiopancreatography to exclude other viral or bacterial infection, autoimmune disorder, and structural problems. The patient's symptoms recovered rapidly and blood chemistry returned to normal with conservative treatment similar to previously reported cases.
Go to : 
Acute hepatitis complicated with acute pancreatitis is often associated with infectious agent such as hepatitis A virus [1], hepatitis B virus [2] or hepatitis E virus [3]. Cases of acute hepatitis combined with pancreatitis induced by Salmonella typhi infection have also been reported [4-6].
Liver enzyme elevation is common in patient with Epstein-Barr virus (EBV) infection, and it typically resolves spontaneously. EBV can also induce cholestasis [7] or pancreatitis [8]. We report a rare case of EBV infection with acute cholestatic hepatitis concurrent with pancreatitis.
Go to : 
An 11-year-old female was admitted to the emergency center of another hospital with a 1-day history of left upper quadrant abdominal pain, nausea and vomiting. Laboratory data revealed amylase at 1,200 U/L (normal range, 0-220), lipase at 2,000 U/L (normal range, 13.8-110), aspartate aminotransferase (AST) at 724 U/L (normal range, 3-38), and alanine aminotransferase (ALT) at 815 U/L (normal range, 4-44). Computed tomography (CT) finding of the abdomen showed swelling of the pancreas with peripancreatic fluid accumulation compatible with acute pancreatitis. She was transferred to our hospital with a preliminary diagnosis of acute hepatitis and pancreatitis.
She had no past history of abdominal trauma, surgery or cholecystitis. She had not received any medications known to cause pancreatitis. She did not report any familial history of pancreatitis or gallstone.
On physical examination she appeared sick with icteric sclera. Tenderness on left upper quadrant of abdomen without rebound tenderness was noticed. Exudative pharyngotonsillitis, cervical lymphadenopathy, and hepatosplenomegaly were not present.
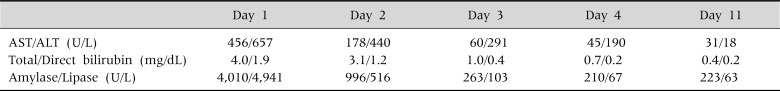
Laboratory investigation revealed hemoglobin of 13.6 g/dL, hematocrit of 39.5%, platelet of 356,000/mm3, white blood cell count of 8,540/mm3 (neutrophil 72%, monocyte 2.7%, lymphocyte 19%). Atypical lymphocyte was absent on peripheral blood smear. Blood chemistry showed AST of 465 U/L, ALT of 657 U/L, total/direct bilirubin of 4.0/1.9 mg/dL (normal range, total bilirubin 0.2-1.2, direct bilirubin 0-0.4). Serum amylase and lipase were elevated to 4,010 U/L and 4,941 U/L respectively (Table 1). Alkaline phosphatase was raised to 1,056 U/L (normal range, 104-338) and gamma-glutamyltransferase was raised to 456 U/L (normal range, 16-73). Diagnosis was acute cholestatic hepatitis concurrent with pancreatitis. Other laboratory data showed prothrombin time-international normalized ratio of 1.02, serum total protein of 7.7 g/dL, serum albumin of 4.5 g/dL, blood urea nitrogen of 7 mg/dL, creatinine of 0.7 mg/dL.
Viral hepatitis profiles results including HBsAg, anti-HAV IgM, anti-HCV, anti-HEV IgM/IgG were all negative. Laboratory results for various infectious agent for pancreatitis and hepatitis including anti-mycoplasma IgM, anti-cytomegalovirus IgM, anti-mumps IgM, anti-rubella IgM, anti-measles IgM, leptospira antibody, Clonorchis sinensis antibody were all negative. Serum antinuclear antibody result to evaluate autoimmune disease was negative. Stool smear test for parasites was also negative.
Although the peripheral blood smear did not show atypical lymphocytes, a diagnosis of reactivated EBV infection was made by the positive result of viral capsid antigen (VCA) IgM, VCA IgG and Epstein-Barr nuclear antigen. Heterophile antibody converted from initial negative result to positive in repeated serologic test on 9th day of hospitalization.
On radiologic examination, the plain radiographs of abdomen were found unremarkable. Magnetic resonance cholangiopancreatography was performed, which did not show choledochal cyst, pancreatic divisum or a pancreatic duct anomaly.
The patient was treated with conservative management with fasting and total parenteral nutrition. On 2nd day of hospitalization, blood chemistry was improved as amylase of 996 U/L, lipase of 516 U/L, AST of 178 U/L, ALT of 440 U/L, total bilirubin of 3.1 mg/dL, direct bilirubin of 1.2 mg/dL. Gastrointestinal symptom such as abdominal pain or vomiting improved also, and she started a regular diet on 4th day when amylase and lipase were normalized (Table 1). On 11th day of hospitalization, rapid normalization of biochemical results was observed on follow up laboratory tests. The results were amylase of 223 U/L, lipase of 63 U/L, AST of 31 U/L, ALT of 18 U/L, total bilirubin of 0.4 mg/dL, direct bilirubin of 0.2 mg/dL (Table 1). During the 20-month-follow up in the outpatient clinic, she remained in good condition without any sign of relapse of the hepatitis or pancreatitis.
Go to : 
Five cases of EBV infection with acute pancreatitis and hepatitis have been reported in the literature [8-12]. The patients' average (range) age was 16.5 (8-23) years. All cases presented with infectious mononucleosis symptoms like fever, sore throat, lymphadenopathy. Onset of abdominal pain and vomiting occurred at an average 7.8 (1-12) days after the onset of prodromal symptoms. Laboratory studies showed an average serum amylase of 584 (271-888) U/L, AST of 220 (76-360) U/L, ALT of 179 (57-415) U/L. Two patients had cholestatic hepatitis [8,11]. Hepatitis preceded by pancreatitis was noted in one patient [10]. Two patients had pancreatitis combined with hepatitis occurring on the same day [11,12]. Radiologic tests were done in three patients. One patient received an abdominal ultrasonography and CT [8]. There were no definite abnormalities except edematous pancreas. Another two patients underwent an oral cystogram with normal results [11,12]. The hepatitis combined with pancreatitis responded to conservative management in all patients even in a patient with septic shock, and disseminated intravascular coagulopathy [5].
Compared with previous reports, this present case did not have infectious mononucleosis symptoms like fever, sore throat, lymphadenopathy. The only presenting symptom was abdominal pain and vomiting. At admission acute pancreatitis was present with cholestatic hepatitis. The patient recovered uneventfully 11 day after admission by supportive treatment for hepatitis and pancreatitis, similarly to other reported cases.
Reports of hepatitis combined with pancreatitis by other infectious agents occurred in 10 cases of hepatitis A, 9 cases of hepatitis E, and 1 case of hepatitis B [1-3]. Compared to EBV infection, cholestasis was present in all cases and hepatitis preceded by pancreatitis. The patient generally needed more time to recover from the hepatitis. On average, serum total bilirubin was 16.4 (5.8-32.4) mg/dL, ALT was 888 (129-7,258) U/L, amylase was 808 (103-2,910) U/L and lipase was 1,753 (133-7,258) U/L. Hepatitis preceded pancreatitis by an average of 13 (2-22) days. All cases were managed with supportive treatment and hepatitis resolved after 4-6 weeks while pancreatitis resolved after 3-13 days.
The mechanism of the relation with development of pancreatitis associated to infectious hepatitis are unknown and likely multifactorial. One proposed hypothesis is direct destruction and inflammation of pancreatic acinar cells by the viruses. This theory is supported by the autopsy finding of hepatitis B surface and core antigens within the cytoplasm of pancreatic acinar cells of patients with hepatitis B surface antigenemia [13]. Another possible mechanism is the development of edema of the ampulla of vater with obstruction to the outflow of pancreatic fluid [3]. Possibly lysosomal enzymes are released by inflamed hepatocytes on circulation resulting in activation of trypsinogen to trypsin from virus-damaged acinar cell membranes [2]. Biliary sludge induced by hypomotility of gallbladder or diet change due to starvation during viral hepatitis can result in an outflow track obstruction of the pancreatic fluid [14].
We report a rare case of EBV infection with acute pancreatitis concurrent with cholestatic hepatitis that did not present any clinical symptoms of infectious mononucleosis. Symptoms and blood chemistry results was recovered rapidly with conservative treatment.
Go to : 
References
1. Mishra A, Saigal S, Gupta R, Sarin SK. Acute pancreatitis associated with viral hepatitis: a report of six cases with review of literature. Am J Gastroenterol. 1999; 94:2292–2295. PMID: 10445566.

2. Jain P, Nijhawan S, Rai RR, Nepalia S, Mathur A. Acute pancreatitis in acute viral hepatitis. World J Gastroenterol. 2007; 13:5741–5744. PMID: 17963301.

3. Bhagat S, Wadhawan M, Sud R, Arora A. Hepatitis viruses causing pancreatitis and hepatitis: a case series and review of literature. Pancreas. 2008; 36:424–427. PMID: 18437090.
4. Huang GC, Chang CM, Ko WC, Huang YL, Chuang YC. Typhoid fever complicated by multiple organ involvement: report of two cases. J Infect. 2005; 51:E57–E60. PMID: 16038753.

5. Kwak IS, Lee SB, Chung JS, Cho GJ, Rha HY. A case of candida fungemia in acute pancreatitis and hepatitis associated with typhoid fever. Korean J Med. 2000; 58:462–465.
6. Jung IS, Kim JW, Lim KS, Choi YM, Kong JM, Shu DR. A case of acute pancreatitis and hepatitis associated with typhoid fever. Korean J Intern Med. 1991; 41:119–122.
7. Kofteridis DP, Koulentaki M, Valachis A, Christofaki M, Mazokopakis E, Papazoglou G, et al. Epstein Barr virus hepatitis. Eur J Intern Med. 2011; 22:73–76. PMID: 21238898.

8. Khawcharoenporn T, Lau WK, Chokrungvaranon N. Epstein-Barr virus infection with acute pancreatitis. Int J Infect Dis. 2008; 12:227–229. PMID: 17913534.

9. Koutras A. Epstein-Barr virus infection with pancreatitis, hepatitis and proctitis. Pediatr Infect Dis. 1983; 2:312–313. PMID: 6310536.

10. Mor R, Pitlik S, Dux S, Rosenfeld JB. Parotitis and pancreatitis complicating infectious mononucleosis. Isr J Med Sci. 1982; 18:709–710. PMID: 6286529.
11. Everett ED, Volpe JA, Bergin JJ. Pancreatitis in infectious mononucleosis. South Med J. 1969; 62:359–360. PMID: 5765134.

12. Wislocki LC. Acute pancreatitis in infectious mononucleosis. N Engl J Med. 1966; 275:322–323. PMID: 5940698.

13. Shimoda T, Shikata T, Karasawa T, Tsukagoshi S, Yoshimura M, Sakurai I. Light microscopic localization of hepatitis B virus antigens in the human pancreas. Possibility of multiplication of hepatitis B virus in the human pancreas. Gastroenterology. 1981; 81:998–1005. PMID: 6169587.
14. Basaranoglu M, Balci NC, Klör HU. Gallbladder sludge and acute pancreatitis induced by acute hepatitis A. Pancreatology. 2006; 6:141–144. PMID: 16354962.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download