Abstract
In Crohn's disease, mild gastrointestinal bleeding often occurs; however massive gastrointestinal hemorrhage, which can have a dramatic effect on a patient's vital sign, is rare. This could result in potentially life-threatening complications, which can lead to death. Massive hemorrhagic Crohn's disease is not well known and for this reason, they are a diagnostic and therapeutic challenge. Various diagnostic and therapeutic methods are currently being developed and used. The surgical method is often used only as a last measure since this approach has the risk of serious complications that may endanger patients. However, if massive bleeding continues even after all therapeutic methods are used, the surgical method must be implemented. In this case, all therapeutic methods were found to be ineffective; therefore, surgery was used as a last option. Ultimately, the surgical method was found to be successfully used to treat life-threatening hemorrhagic Crohn's disease.
Crohn's disease is an inflammatory disease of unknown etiology and can occur in any gastrointestinal tract from the oral cavity to the anus [1]. This disease brings about complications, including intestinal stricture, fistula and gastrointestinal bleeding. Whereas mild gastrointestinal bleeding is a common manifestation, acute and severe lower gastrointestinal bleeding, which significantly lowers blood pressure, is rare. Massive hemorrhagic Crohn's disease is not well known and for this reason, it represents a diagnostic and therapeutic challenge.
One of the common characteristic of Crohn's disease is that it repetitively shows recurring and worsening clinical progress and no clear treatment is developed for now [2,3]. Due to the diverse clinical presentations and complications of this disease, various therapeutic methods have been used and new treatments based on clinical studies are being suggested. Among these, medical therapy, endoscopic therapy and arterial embolization have been reported to be effective in controlling the bleeding of hemorrhagic Crohn's disease [4,5]. However, if massive bleeding continues even after attempting these various therapeutic methods, the surgical method must be used.
In this study, a 13 year old with Crohn's disease was admitted to the hospital and all methods, including medical therapy, exclusive enteral nutrition (EEN), angiographic intervention were attempted without success. Severe hemorrhagic gastrointestinal bleeding continued and without any further options, surgical therapy was performed. This mode of treatment eventually lead to successful controlled bleeding. This case is even more significant because it is extremely rare for massive hemorrhagic Crohn's disease to occur among children. In addition, this was the first case where severe gastrointestinal bleeding was the presenting symptom of Crohn's disease.
A 13 years old boy was admitted to the hospital because of gross hematochezia. There was nothing significant in the patient's past medical history over the past 6 months. He reported suffering from intermittent diarrhea and abdominal pain. Also, he went from 47 kg to 40 kg during the course of 3 months. He was initially believed to have hematochezia and therefore a colonoscopy was performed. After the colonoscopy, he was sent to our hospital with suspicion of inflammatory bowel disease. At his first visit, his blood pressure, pulse rate, respiratory rate, body temperature, height and body weight were 110/65 mm/Hg, 90/min, 20/min, 36.5℃, 164.2 cm (25-50 p) and 40 kg (5-10 p), respectively. He appeared chronically ill and was pale. The physical examination upon admission showed slight pain and tenderness at the peri-umbilical region without muscular guarding. His bowel sounds were normal and the rectal examination revealed an empty ampulla with no other peculiar symptoms regarding peri-anal abscess or fistula. The laboratory investigations during the first exam were as follows: erythrocyte sedimentation rate (ESR) 84 mm/h, C-reactive protein 106 mg/L (normal 0-8 mg/L), albumin 2.8 g/dL, prothrombin time 11.5 sec, partial thromboplastin time 28.1 sec, hemoglobin 10.4 g/dL, leucocytes 9.8×109/L with normal leukocyte differentiation, and thrombocytes 489×109/L. A stool occult blood test was also performed and found to be positive. The colonoscopy showed an inflammatory bowel with multiple linear deep ulcerations, cobble stone appearances and pseudo-polyps (Fig. 1). In addition, in the MRI enterography, a diffuse bowel wall thickening was observed at the distal to terminal ileum, cecum and rectosigmoid colon. Accordingly, he was diagnosed with Crohn's disease. His Pediatric Crohn's disease Activity Index (PCDAI) score was 68. Initially, induction therapy was performed with oral steroids (30 mg/day) and Azathioprine (100 mg/day). He was also given 8weeks of EEN with a polymeric formula (Monowell 2,000 mL daily). After medical therapy, the abdominal pain has declined slightly and the ESR and C-reactive protein (CRP) was reduced but intermittent mild bloody stools were still observed. After the 10th day of hospitalization, approximately 1,000 mL of a fresh bloody stool and dizziness with about a 10-second loss of consciousness had occurred. At this time, his blood pressure had dropped to 80/40 mmHg. In addition, his hemoglobin levels dropped from 10.4 g/dL to 7.6 g/dL. Accordingly, 6 units blood transfusion was performed over a 24 hour time period. After the blood transfusion, his vital signs had stabilized. Based on the patient's past history and the colonoscopy data, we presumed that this gastrointestinal hemorrhage was caused by Crohn's disease. At that point, oral steroid treatment was changed to intravenous steroids and the patient was placed under conservative care. However, even after 10 days, due to over 500 mL of continuous massive hematochezia and repetitive hemoglobin drop, blood transfusion was needed. Thus, a bleeding focus evaluation was performed. From the GI bleeding scintigraphy, the radiotracer was found to be up taken in the mid to left upper quadrant in the abdomen and no abnormal signs were observed in the abdomen CT. A duodenal ulcer was observed in the upper endoscopy but no other acute findings were made. A colonoscopy was then performed and multiple active ulcerations in the distal ileum and inflammatory polyps and cobble stone appearance were found (Fig. 2). Ulcers and bleeding was also expected to be found; however, current active bleeding was not observed and no other bleeding focus was present. For 3 weeks, even with steroid induction and azathioprine therapy, mucosal healing was not successful. The PCDAI score was also 60, which was indicative of continued severe disease activity. Since steroid therapy was ineffective, infliximab infusion (5 mg/kg) was initiated. On the 21st day, a superior mesenteric angiography was performed. In this test, no active bleeding was observed; however, a hypervascular blush, which caused by inflammatory changes, was observed near the proximal ascending colon and ileocecal (IC) valve. To account for this, 2 superior mesenteric arteries were selected using a microcatheter and gel foam arterial embolization was successfully performed (Fig. 3 and 4). A hematochezia was found nowhere and the PCDAI score had decreased by 20 points. Starting on the 27th day, mucosal healing and bleeding was thought to be well managed from infliximab infusion and embolization and maintenance therapy was performed using mesalazine (4,000 mg/day). 2 weeks after the first infliximab injection, which corresponded to the 34th day of hospitalization, valve, a second infusion of infliximab (5 mg/kg) was done. However, 650 mL of massive hematochezia was observed on the 35th day of hospitalization. For the first 24 hours, the patient was given 2 units of blood. However, even with active transfusion, the massive rectal hemorrhage continued and his hemoglobin levels dropped from 12.6 gm/dL to 11.6 gm/dL. At this point, we deemed it necessary to perform surgery. To examine the precise operation scale, a second angiography was performed before the operation. The superior mesenteric artery angiography showed a hypervascular blush near the proximal ascending colon and IC valve; however, no active bleeding was observed (Fig. 5). On the 36th day of hospitalization, an ileocecectomy and hand sewn end to side anastomosis were performed. During the operation, wall edema and inflammation was found on the IC valve which was about 30 cm deep into the terminal ileum. An ileostomy was initiated to observe the inside of the lumen and a cobble like appearance, mucosal ulceration and dark blood clot was found. The lumen of the cecum was relatively clean and inflammation was not severe. Although a single bleeding point was not identified, the hemorrhage presumably originated from the diffusely multifocal ulcerated ileal mucosa. Approximately 30 cm of the terminal ileum and cecum together were cut and an ileocecectomy was performed as well as a hand swen end to side anastomosis (Fig. 6). According to the pathologic examination, the ileocecum was erythematous and multiple ulceration, transmural inflammation with perforation and small non-caseating granuloma were observed, a condition that was compatible with Crohn's disease. No colonic diverticula were identified. After the ileocecectomy, the patient's bleeding promptly ceased and he did not require additional blood transfusions. On the 6th postoperative day, a clear liquid diet was started and on the 7th postoperative day, a dark brown colored stool was evident; however, no more hemorrhage episodes occurred and the abdominal pain was managed, which resulted in a steady increase in food consumption. The daily dose of prednisolone was set at 30 mg/day initially and was decreased according to the clinical activity of the disease. On the 12th postoperative day, the PCDAI score was 15 and the wound had cleared; therefore, the patient was discharged. Currently, the patient is in maintenance therapy and receives only infliximab. After the hospitalization, the PCDAI score remained below 10 and disease activity was controlled. The patient has no recurrence of bleeding or evidence of Crohn's disease and is currently in good condition.
Hematochezia is one of common manifestations of Crohn's disease and occurs in 45% of patients with this disease [6]; however massive gastrointestinal hemorrhage, which could cause a decrease in blood pressure, is a rare complication that occurs in only about 0.9% to 2.5% of patients with Crohn's disease [4,7]. There is no exact protocol regarding treatment of massive hemorrhagic Crohn's disease, which is rare. Original medical literature and works still provide insufficient information on massive hemorrhagic Crohn's disease patients [8].
A conservative approach has been suggested for initial treatment of these patients [9]. However, if bleeding cannot be controlled even with medical therapy and conservative care, additional acute therapeutic interventions are needed. Several approaches such as endoscopic treatment, angiographic intervention and surgical resection have been used to treat this disease [10,11].
For a majority of life threatening lower gastrointestinal hemorrhage patients, emergent surgical resection is performed as a standard treatment [4]. Cirocco et al. [7] reported that surgical resection offered excellent palliation, with low mortality (3%) and a low rebleeding rate (5.7%), when compared with those patients managed medically (38%).
However, it has been found out that Crohn's disease can easily reoccur and surgical resection does not affect the recurrence rate of Crohn's disease [12]. Also, surgery increases the risk of major complications, such as post operative bowel obstruction, intra-abdominal and wound infections, anastomotic leakages, and fistulas [13]. From repetitive bowel resection, serious complications, such as short bowel syndrome can occur, which could result in a variable amount of diarrhea and metabolic upset [2]. As described above, there are many limitations to the surgical method; thus, various therapeutic methods should be used together.
Non-surgical methods are preferred if an operation is not needed. Non-surgical methods include angiographic embolization, arterial vasopressin therapy, EEN and infliximab [5,10,14].
Superselective embolization has been used to prevent surgical resection in hemorrhagic Crohn's disease [4]. This therapeutic intervention with embolization was shown to have a downside: risk for intestinal infarction. However, with recent advances in interventional radiological techniques, developed microcatheters and embolic agents and microcoils, complications such as infarction have significantly decreased [8]. Therefore, angiographic embolization can be used as an initial treatment strategy for hemorrhagic Crohn's disease. It has been reported that angiographic embolization has a success rate ranging from 81% to 93%, with a mortality rate between 0% and 7% [5].
The availability of arterial vasopressin therapy to control bleeding during a massive hemorrhage in Crohn's disease has also been reported [15]. Even though vasopressin infusion was not sufficient to cease the hemorrhage and control the bleeding completely, the injection could provide time for stabilization and full resuscitation and thus it could be utilized to provide more time for the operation [16]. Another benefit of using vasopressin is that it can be selectively used in diffuse lesions and cases in which super selective catheterization is not technically possible [6].
EEN is also currently used for the treatment of Crohn's disease and it has been shown to have several benefits. EEN was first performed in 1973 by Voitk et al. [14] to reinforce the nutritional state of patients with Crohn's disease who were resistive to diverse types of medications. After the first report of remission of induction of this patient, the potential of using EEN to treat Crohn's disease was investigated [17]. Positive effects such as mucosal healing and nutritional improvements due to EEN treatment have been reported.
The use of infliximab for treatment of this disease is also controversial. Typically, for refractory Crohn's disease, which original medications aren't effective, and recurrable gastrointestinal bleeding, Infliximab could have possible benefits in regards to treatment [10,18,19]. Infliximab can induce rapid and sustained mucosal healing [10]. For instance, according to one study, steroids only have a 29% incidence of mucosal healing, whereas infliximab offers a theoretical advantage over steroids given its high rate of mucosal healing, which is about 50% [20]. In addition, infliximab has been shown to suppress and resolve severe acute bleeding [10]. Because this therapy has very rapid effects, and may be used instead of surgical resection for uncontrolled bleeding, we believe that infliximab therapy should be considered for acute and massive GI bleeding in Crohn's disease before surgery [10].
As described above, various methods to treat Crohn's disease with gastrointestinal bleeding without any surgical procedure have been suggested; however, if medical treatment fails or bleeding continues even with intervention, bowel resection through surgical therapy should be performed. Crohn's diseases with bleeding can be controlled in more than 50% of all cases by the use of medical treatment. Among these, 30% will reoccur and the surgical methods must often be performed to control bleeding [6]. Therefore, when recurrent major hemorrhage or severe bleeding is found, bowel resection through the surgical method should be considered.
In this case, severe gastrointestinal bleeding which almost unstabilized vital sign as a first symptom was observed at 13 years old Crohn's disease patient. After a massive blood transfusion, various therapeutic methods such as EEN and medical treatment were used; however, none were effective. Accordingly, diagnostic methods, such as colonoscopy upper endoscopy, GI bleeding scintigraphy and angiography were used to localize the bleeding point and bleeding was instantly ceased by arterial embolization and infliximab therapy. However, a massive hemorrhage soon recurred; thus, operation was performed and the bleeding was eventually successfully controlled.
In general, the surgical method is not always the first choice for the treatment of patients with massive hemorrhagic Crohn's disease because this treatment option can also result in many serious complications that could endanger the patient. However, if all other therapeutic methods are not effective, the surgical method should be considered as a final option.
Figures and Tables
Fig. 1
The 1st colonoscopy. Multiple linear deep ulcerations, cobble stone appearance and pseudo-polyp at terminal ileum, which are consistent with Crohn's disease.
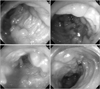
Fig. 2
The 2nd colonoscopy. Current active bleeding was not observed and no other bleeding focus was found in the scope.
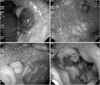
Fig. 3
The 1st superior mesenteric angiography shows increased focal staining in the ileocecal valve and proximal ascending colon.
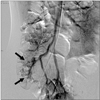
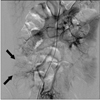
Fig. 4
Two superior mesenteric artery branches were selected and arterial embolization was performed.

References
1. Fascì Spurio F, Aratari A, Margagnoni G, Doddato MT, Papi C. Early treatment in Crohn's disease: do we have enough evidence to reverse the therapeutic pyramid? J Gastrointestin Liver Dis. 2012. 21:67–73.
2. Kim HA, Chung SS, Kim KH, Lee RA. The change of the clinical features that Crohn's disease treated by surgery. J Korean Surg Soc. 2005. 69:135–138.
3. Lee NY, Park JH. Clinical features and course of crohn disease in children. Korean J Gastrointest Endosc. 2007. 34:193–199.
4. Kazama Y, Watanabe T, Akahane M, Yoshioka N, Ohtomo K, Nagawa H. Crohn's disease with life-threatening hemorrhage from terminal ileum: successful control by superselective arterial embolization. J Gastroenterol. 2005. 40:1155–1157.

5. Alla VM, Ojili V, Gorthi J, Csordas A, Yellapu RK. Revisiting the past: intra-arterial vasopressin for severe gastrointestinal bleeding in Crohn's disease. J Crohns Colitis. 2010. 4:479–482.

6. Bae JW, Ko BS, Kim DH, Jeon HJ, Park SM, Youn SC, et al. A case of Crohn's disease with blood pressure falling intestinal bleeding. Korean J Gastrointest Endosc. 1998. 18:271–275.
7. Cirocco WC, Reilly JC, Rusin LC. Life-threatening hemorrhage and exsanguination from Crohn's disease. Report of four cases. Dis Colon Rectum. 1995. 38:85–95.
8. Iiritano E, Grassia R, Staiano T, Buffoli F. Life-threatening jejunal hemorrhage as first presentation of Crohn's disease. Inflamm Bowel Dis. 2010. 16:1277–1278.

9. Di Fiore F, Lecleire S, Hervé S, Savoye G, Lerebours E. Life-threatening bleeding revealing gastric involvement in a Crohn's disease patient. J Clin Gastroenterol. 2004. 38:833–834.

10. Ando Y, Matsushita M, Kawamata S, Shimatani M, Fujii T, Okazaki K. Infliximab for severe gastrointestinal bleeding in Crohn's disease. Inflamm Bowel Dis. 2009. 15:483–484.

11. Ye BD, Yang SK, Shin SJ, Lee KM, Jang BI, Cheon JH, et al. IBD Study Group of the Korean Association for the Study of the Intestinal Diseases. Guidelines for the management of Crohn's disease. Korean J Gastroenterol. 2012. 59:141–179.

12. Lee YJ, Oh SH, Kim KM. The principles of drug therapy of Crohn's disease in child and adolescent. Korean J Pediatr Gastroenterol Nutr. 2010. 13:Suppl 1. S59–S69.

13. Gardiner KR, Dasari BV. Operative management of small bowel Crohn's disease. Surg Clin North Am. 2007. 87:587–610.

14. Voitk AJ, Echave V, Feller JH, Brown RA, Gurd FN. Experience with elemental diet in the treatment of inflammatory bowel disease. Is this primary therapy? Arch Surg. 1973. 107:329–333.

15. Podolny GA. Crohn's disease presenting with massive lower gastrointestinal hemorrhage. AJR Am J Roentgenol. 1978. 130:368–370.

16. Barreiro de Acosta M, Seijo Ríos S, Domínguez Muñoz JE. Life-threatening acute lower gastrointestinal bleeding in patients with Crohn's disease. Rev Esp Enferm Dig. 2007. 99:388–391.
17. Suh HA, Kim SE, Jang JY, Kim BJ, Kim JS, Lee SY, et al. Efficacy of nutritional therapy in children with Crohn disease. Korean J Pediatr Gastroenterol Nutr. 2006. 9:210–217.

18. Lee KM, Kim JS, Shin DH, Cheong JY, Yoo BM, Kim JK, et al. Effect of infliximab in the treatment of refractory inflammatory bowel disease with complication. Korean J Gastroenterol. 2004. 44:259–266.
19. Kim SH, Yang S, Kim KJ, Kim EH, Yoon SM, Ye BD, et al. Efficacy of infliximab in the treatment of Korean patients with crohns disease. Korean J Gastroenterol. 2009. 54:108–116.

20. Ryu MK, Kim YH, Hyun JG, Moon W, Lee KS, Lee SS, et al. Clinical investigations of Crohn's disease in Korea. Korean J Med. 2001. 60:46–50.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download