Abstract
Benign recurrent intrahepatic cholestasis (BRIC) is a rare autosomal recessive inherited disorder characterized by multiple recurrent episodes of severe cholestatic jaundice without obstruction of extrahepatic bile duct. We present the case of a 7-year-old boy with BRIC confirmed by mutation analysis in the ATP8B1 gene and typical clinical manifestation. Despite inheritance of BRIC, we detected a mutation on only one allele. To our knowledge, this is the first report of BRIC with a confirmed single heterozygote novel mutation in the ATP8B1 gene in Korea.
Benign recurrent intrahepatic cholestasis (BRIC) is a rare autosomal recessive inherited disorder characterized by multiple recurrent episodes of severe cholestatic jaundice without extrahepatic bile duct. Often the diagnosis is delayed, and patients frequently experience invasive diagnostic procedures without any conclusions. The identification of the genes responsible for the familial intrahepatic cholestasis has significantly improved the understanding of the disease and made the diagnosis of BRIC easier [1].
A male born in 2004 experienced his first cholestatic attack at 6-months-of-age. The patient was admitted with unexplained jaundice. There was no significant familial history. Immunologic and viral tests were negative. Both the 99mTc-diisopropyl iminodiacetic acid (DISIDA) scan and liver biopsy were normal except for mild cholestatic features in the biopsy. The first cholestatic episode lasted for about 6 months. Maximum total bilirubin and direct bilirubin were 20 mg/dL and 16.4 mg/dL, respectively, but γ-glutamyltranspeptidase (GGT) was normal. Ursodeoxycholic acid and rifampicin were given with little effect.
Three months later (2005), the second attack developed. The attack was preceded by an upper respiratory tract infection. During this attack, ursodeoxycholic acid and rifampicin were given with some effect. This attack ended after 3 months. Growth parameters were appropriate with a body weight of 11 kg (75-90th percentile) and a length of 77 cm (50-75th percentile).
After 2 years (2007), the patient suffered a third cholestatic episode, complicated with pancreatitis. The patient had taken herbal medicine 2 weeks prior to the episode. The total bilirubin level rose to more than 29.5 mg/dL. Maximum alkaline phosphatase (ALP), alanine aminotransferase (ALT), and GGT level was 390, 44, and 22 U/L, respectively. Amylase increased to 1,173 U/L. A computed tomography (CT) scan confirmed the diagnosis of acute pancreatitis. Bilirubin normalized after 5 months. Despite the diagnosis, there was a suspicion of BRIC. However, a genetic study was not performed due to lack of consent. Cholestyramine and antihistamines were given without any effect on the pruritus. In this attack, phenobarbital was administered in addition to ursodeoxycholic acid, but had no effect. Growth parameters were relatively small for age with a birth weight of 13.4 kg (10-25th percentile), a length of 92.9 cm (10-25th percentile). During the third attack, the patient was prepared for a liver transplantation (LT) due to severe pruritus and growth retardation. But the bilirubin normalized after 8 months.
One year later, in 2008, the patient experienced a fourth attack, which was preceded by an acute sinusitis. Ursodeoxycholic acid and cholestyramine were given for pruritus. Subsequently, bilirubin normalized after 6 months.
In 2009, the patient experienced a fifth attack. At that time, a gene study was performed. Written informed consent was obtained. DNA was extracted from peripheral blood leukocytes as previously described [4] and the sequences of all coding exons of ATP8B1, including the exon-intron boundaries, were determined. A heterozygote frame shift mutation by insertion of a nucleotide C at 2610_2611 (p.K871QfsX) was detected. The results confirmed a single heterozygote mutation in the ATP8B1 gene (Fig. 1). According to the literature concerning the inheritance of BRIC, mutation on two alleles is necessary. However, this patient displayed typical clinical manifestations. BRIC was diagnosed by genetic and clinical findings. This attack ended after 8 months.
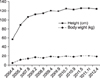
In March, 2010, the patient experienced a sixth attack, which was complicated with pancreatitis. Ursodeoxycholic acid and cholestyramine were given early in the course. The symptoms of pruritus improved but total bilirubin levels reached a maximum of 34.6 mg/dL and have not normalized. At that time, growth parameters were a body weight of 13.4 kg (10-25th percentile) and a length of 92.9 cm (10-25th percentile). To date, the patient's growth has not caught up (Fig. 2). The most recent liver ultrasonography finding was mild hepatosplenomegaly. Although the radiologic finding was near normal, we are considering LT because of the patient's severe growth retardation.
Fig. 3 shows total bilirubin, direct bilirubin and GGT level follow-up from the third attack to date.
Progressive familial intrahepatic cholestasis (PFIC), BRIC, and intrahepatic cholestasis of pregnancy (ICP) represent three different forms of familial intrahepatic cholestasis (FIC) characterized by intrahepatic cholestasis. Inheritance is autosomal recessive. The differentiation between PFIC, BRIC, and ICP is based on phenotypic presentation [1,5]. While PFIC starts in infancy or early childhood and often leads to liver cirrhosis, BRIC usually appears later in life and has a more benign recurrent pattern [6]. BRIC was first described by Summerskill and Walsh in 1959 [7]. In 1969, Tygstrup and Jensen [8]described the condition in five young males from the Faroe Islands. It was long suspected that the condition was inherited, and in 1994 it was possible to show that three different patients had the same gene segment on chromosome18 [9]. In 1998, a mutation in the ATP8B1 gene on chromosome 18q21 was localized [10].
The ATP8B1 gene is an aminophospholipid translocator (aminophospholipid flippase) localized on canalicular membranes in hepatocytes and in cholangiocytes. It is important for the normal flow of bile over the membranes, probably by maintaining an asymmetric distribution of different phospholipids between the outer and inner leaflets of the plasma membrane [11]. Deficiency of ATP8B1 may result in membrane instability, lack of cholesterol in the apical membrane, and reduced function of transmembrane transporters like the bile salt export pump (BSEP). The BSEP is the most important transporter of bile salts into the canaliculus. Therefore, it is not surprising that a malfunction can be responsible for severe cholestasis. ATP8B1 is expressed in extrahepatic tissues such as pancreas and small intestine. Therefore, pancreatitis and diarrhea can be present in patients [1,5]. Our patient had two attacks of pancreatitis.
To diagnose BRIC, the patient must have a minimum of two episodes of jaundice separated by intervals of weeks to years without any symptoms or cholestasis. Typically, GGT is normal during an episode with profound cholestasis. Ultrasound examination and magnetic resonance cholangio-pancreaticography do not show any abnormality. Other factors associated with cholestasis had to excluded. This combined clinical, biochemical, radiological, and histological approach associated with liver immunostaining and biliary lipid analysis should help to select BRIC candidates in whom a molecular diagnosis can be proposed [12].
By the sequencing of all coding exons of ATP8B1, we detected a heterozygote frame shift mutation by insertion of a nucleotide C at 2610_2611 (p.K871QfsX). To date, over 50 distinct mutations in ATP8B1 have been described [4,10,13]. The mutations G308V, D554N, and I661T are among the most frequently detected [5]. Seventy nine percent (27 of 34 combining this and our previous studies) [10,14,15] of Western European BRIC patients harbor ATP8B1 mutations carrying at least one copy of I661T4). However, a mutation in p.K871QfsX has not previously been reported, and so represents a novel mutation.
We detected a mutation on only one allele. Similarly, Leo et al. [4] analyzed 50 BRIC families and found three families with a mutation on single allele. A possible explanation is that a counter allele was present but was not detected. Some mutations (e.g., large deletions) may be undetectable by the methods used or may affect regions not analyzed (viz., untranslated regions, upstream regulatory sequences, introns) [4].
BRIC is a characterized by multiple episodes of cholestasis without extrahepatic bile duct obstruction and without permanent liver damage. Usually, LT is not indicated. But we are considering LT in the present case due to the severe growth retardation. Another case reported BRIC with LT due to uncontrolled pruritus, which could not be continued for life. The female patient underwent transplantation without requiring any blood transfusion and immediately became free of pruritus [16].
Our patient's last attack has not yet terminated. Two suppositions are possible. Our hypothesis is possibility of progression to PFIC. Occasionally BRIC will progress to the more severe and permanent form of PFIC, indicative of a clinical continuum, with intermediate phenotypes between mild and progressive disease [17-19]. Another hypothesis is a long duration of attack. But, according to other case, attack usually lasts for 2-24 weeks [7]. So, we are more concerned with the possibility of progression to PFIC and are conducting frequent radiologic evaluations.
We report here a typical BRIC patient confirmed with a single heterozygote novel mutation in the ATP8B1 gene.
Figures and Tables
Fig. 1
Direct sequencing of PCR products amplified from exon 22 of the ATP8B1 gene. The patient displayed a heterozygote frame shift mutation by insertion of a nucleotide C at 2610_2611.

References
1. Folvik G, Hilde O, Helge GO. Benign recurrent intrahepatic cholestasis: review and long-term follow-up of five cases. Scand J Gastroenterol. 2012. 47:482–488.

2. Kim OY, Sung BY, Kowg GD, Yoon HS, Shin YM, Oh HT, et al. A case of nonfamilial benign recurrent intrahepatic cholestasis. Korean J Hepatol. 1998. 4:188–193.
4. Klomp LW, Vargas JC, van Mil SW, Pawlikowska L, Strautnieks SS, van Eijk MJ, et al. Characterization of mutations in ATP8B1 associated with hereditary cholestasis. Hepatology. 2004. 40:27–38.

5. van der Woerd WL, van Mil SW, Stapelbroek JM, Klomp LW, van de Graaf SF, Houwen RH. Familial cholestasis: progressive familial intrahepatic cholestasis, benign recurrent intrahepatic cholestasis and intrahepatic cholestasis of pregnancy. Best Pract Res Clin Gastroenterol. 2010. 24:541–553.

6. Lykavieris P, van Mil S, Cresteil D, Fabre M, Hadchouel M, Klomp L, et al. Progressive familial intrahepatic cholestasis type 1 and extrahepatic features: no catch-up of stature growth, exacerbation of diarrhea, and appearance of liver steatosis after liver transplantation. J Hepatol. 2003. 39:447–452.

7. Summerskill WH, Walshe JM. Benign recurrent intrahepatic "obstructive" jaundice. Lancet. 1959. 2:686–690.
8. Tygstrup N, Jensen B. Intermittent intrahepatic cholestasis of unknown etiology in five young males from the Faroe Islands. Acta Med Scand. 1969. 185:523–530.

9. Houwen RH, Baharloo S, Blankenship K, Raeymaekers P, Juyn J, Sandkuijl LA, et al. Genome screening by searching for shared segments: mapping a gene for benign recurrent intrahepatic cholestasis. Nat Genet. 1994. 8:380–386.

10. Bull LN, van Eijk MJ, Pawlikowska L, DeYoung JA, Juijn JA, Liao M, et al. A gene encoding a P-type ATPase mutated in two forms of hereditary cholestasis. Nat Genet. 1998. 18:219–224.

11. Stapelbroek JM, van Erpecum KJ, Klomp LW, Houwen RH. Liver disease associated with canalicular transport defects: current and future therapies. J Hepatol. 2010. 52:258–271.

12. Davit-Spraul A, Gonzales E, Baussan C, Jacquemin E. Progressive familial intrahepatic cholestasis. Orphanet J Rare Dis. 2009. 4:1.

13. Liu LY, Wang XH, Wang ZL, Zhu QR, Wang JS. Characterization of ATP8B1 gene mutations and a hot-linked mutation found in Chinese children with progressive intrahepatic cholestasis and low GGT. J Pediatr Gastroenterol Nutr. 2010. 50:179–183.

14. Bull LN, Juijn JA, Liao M, van Eijk MJ, Sinke RJ, Stricker NL, et al. Fine-resolution mapping by haplotype evaluation: the examples of PFIC1 and BRIC. Hum Genet. 1999. 104:241–248.

15. Tygstrup N, Steig BA, Juijn JA, Bull LN, Houwen RH. Recurrent familial intrahepatic cholestasis in the Faeroe Islands. Phenotypic heterogeneity but genetic homogeneity. Hepatology. 1999. 29:506–508.

16. Mezey E, Burns C, Burdick JF, Braine HG. A case of severe benign intrahepatic cholestasis treated with liver transplantation. Am J Gastroenterol. 2002. 97:475–477.

17. van Mil SW, Klomp LW, Bull LN, Houwen RH. FIC1 disease: a spectrum of intrahepatic cholestatic disorders. Semin Liver Dis. 2001. 21:535–544.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download