Abstract
As the prevalence of tuberculosis declines, the proportion of mycobacterial lung disease due to nontuberculous mycobacteria (NTM) is increasing worldwide. In Korea, M. avium complex and M. abscessus account for most of the pathogens encountered, whilst M. kansasii is a relatively uncommon cause of NTM pulmonary diseases. NTM pulmonary disease is highly complex in terms of its clinical presentation and management. Because its clinical features are indistinguishable from those of pulmonary tuberculosis and NTMs are ubiquitous in the environment, the isolation and identification of causative organisms are mandatory for diagnosis, and some specific diagnostic criteria have been proposed. The treatment of NTM pulmonary disease depends on the infecting species, but decisions concerning the institution of treatment are far from being easy. It requires the use of multiple drugs for 18 to 24 months. Thus, the treatment is expensive, often has significant side effects, and is frequently not curative. Therefore, clinicians should be confident that there is a sufficient clinical evidence to warrant prolonged, multidrug treatment regimens. In all situations, outcomes can be best optimized only when the clinicians, radiologists, and laboratories work cooperatively. The purpose of this article is to review the common presentations, diagnosis and treatment of the NTM that most commonly cause lung disease in Korea.
Figures and Tables
 | Figure 1
M. intracellulare pulmonary disease of the upper lobe cavitary form in a 56-year-old man. Chest radiograph shows cavitary consolidation in the right upper lobe. |
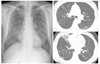
 | Figure 2
M. intracellulare pulmonary disease of the nodular bronchiectatic form in a 67-year-old woman. Chest radiograph shows a multifocal patchy distribution of small nodular clusters in both lungs. Transaxial lung window CT images (2.5mm section thickness, 70mA) show small centrilobular nodules and bronchiectasis in the both lungs, especially in the right middle lobe and in the lingular division of the left upper lobe. |
 | Figure 3
M. abscessus pulmonary disease in a 60-year-old woman. Chest radiograph shows multifocal patchy areas of small nodular clusters in both lungs. Transaxial lung window CT images (2.5mm section thickness, 70 mA) show bronchiectasis and small centrilobular nodules or tree-in-bud opacities in the both lungs, especially in the right middle lobe. Also note bronchiolitis of small centrilobular nodules and tree-in-bud opacities in both lower lobes. |
References
1. American Thoracic Society. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am J Respir Crit Care Med. 1997. 156:S1–25.
2. British Thoracic Society. Management of opportunist mycobacterial infections: Joint Tuberculosis Committee Guidelines 1999. Thorax. 2000. 55:210–218.
3. Korean Academy of Tuberculosis and Respiratory Diseases (KATRD). KATRD. Nontuberculous mycobacterial lung disease. Guideline of management of tuberculosis. 2005. Seoul: KATRD;136–146.
4. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci. 2005. 20:913–925.

5. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006. 129:341–348.

6. Yim JJ, Park YK, Lew WJ, Bai GH, Han SK, Shim YS. Mycobacterium kansasii pulmonary diseases in Korea. J Korean Med Sci. 2005. 20:957–960.
7. Jeon K, Koh WJ, Kwon OJ, Suh GY, Chung MP, Kim H, et al. Recovery rate of NTM from AFB smear-positive sputum specimens at a medical centre in South Korea. Int J Tuberc Lung Dis. 2005. 9:1046–1051.
8. Field SK, Fisher D, Cowie RL. Mycobacterium avium complex pulmonary disease in patients without HIV infection. Chest. 2004. 126:566–581.

9. Jeong YJ, Lee KS, Koh WJ, Han J, Kim TS, Kwon OJ. Nontuberculous mycobacterial pulmonary infection in immunocompetent patients: comparison of thin-section CT and histopathologic findings. Radiology. 2004. 231:880–886.

10. Koh WJ, Lee KS, Kwon OJ, Jeong YJ, Kwak SH, Kim TS. Bilateral bronchiectasis and bronchiolitis at thin-section CT: diagnostic implications in nontuberculous mycobacterial pulmonary infection. Radiology. 2005. 235:282–288.

11. Chung MJ, Lee KS, Koh WJ, Lee JH, Kim TS, Kwon OJ, et al. Thin-ection CT findings of nontuberculous mycobacterial pulmonary diseases: comparison between Mycobacterium avium-intracellulare complex and Mycobacterium abscessus infection. J Korean Med Sci. 2005. 20:777–783.

12. Daley CL, Griffith DE. Pulmonary disease caused by rapidly growing mycobacteria. Clin Chest Med. 2002. 23:623–632.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download