Abstract
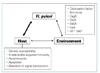
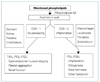
Before the discovery of H. pylori, the therapy of peptic ulcer disease(PUD) was focused on the acid secretion. Although acid secretion is still important in the pathogenesis of PUD, eradication of H. pylori and therapy/prevention of NSAID-induced disease is the mainstay of therapy these days. Multiple drugs have been evaluated in the therapy of H. pylori. No single agent is effective in eradicating the organism. Combination therapy for 10 to 14 days provides the greatest efficacy. The combination of two antibiotics among amoxicillin, metronidazole and clarithromycin plus either a PPI or bismuth compound(RBC : ranitidine bismuth citrate) has comparable success rates. Medical intervention for NSAID-related mucosal injury includes treatment of an active ulcer and prevention of future injury. Ideally the injurious agent should be stopped as the first step in the therapy of an active NSAID-induced ulcer. If that is possible, then treatment with one of the acid inhibitory agents (H2 blockers, PPIs) is indicated. Cessation of NSAIDs is not always possible because of the patient's severe underlying disease. Only PPIs can heal GUs or DUs, independent of whether NSAIDs are discontinued. Prevention of NSAID-induced ulceration can be accomplished by misoprostol (200 µg qid) or a PPI. The use of COX-2 specific inhibitor may also reduce injury to gastric mucosa. H. pylori-negative idiopathic peptic ulcer disease appears to be increasing. Antisecretory drugs remain the mainstay of treatment for promoting healing of idiopathic peptic ulceration. However, in the absence of H. pylori infection, antisecretory drugs are less effective in inhibiting gastric acidity. Managment of idiopathic PUD needs to be further defined and will require new clinical studies.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download