Abstract
Contrast echocardiography is an important technique that can be used to examine the cardiac cavity, vascular structure, intracardiac shunt, and myocardial microcirculation. It uses gas-filled microbubbles and various imaging techniques. The properties of microbubbles and their interaction with ultrasound are important in ultrasound-enhanced contrast imaging. This article will describe microbubble physics and new ultrasound techniques that are necessary to understand the basics of contrast echocardiography. The utility of contrast echocardiography in various clinical scenarios will be also described.
Figures and Tables
References
1. Oh JK, Seward JB, Tajik AJ. Contrast echocardiography. The Echo Manual. 2nd ed. 245–249.
2. de Jong N. de Jong N, editor. Higher harmonics of vibrating gas-filled microspheres. Acoustic Properties of Ultrasound Contrast Agents. 1993. Woerden, Germany: Zuidam and Zonen bv;61–78.
3. Burns PN, Powers JE, Simpson DH, Uhlendorf V, Fritzsche T. Harmonic imaging : principles and preliminary results. Clin Radiol. 1996. 51:Suppl I. 50–55.
4. de Jong N, Hoff L, Skotland T, Bom N. Absorption and scatter of encapsulated gas filled microspheres : theoretical considerations and some measurements. Ultrasonics. 1992. 30(2):95–103.

5. de Jong N, Hoff L. Ultrasound scattering properties of Albunex microspheres. Ultrasonics. 1993. 31:175–181.

6. Wei K, Skyba DM, Firschke C, Jayaweera AR, Lindner JR, Kaul S. Interactions between microbubbles and ultrasound : in vitro and in vivo observations. J Am Coll Cardiol. 1997. 29(5):1081–1088.

7. Frinking PJA, de Jong N, Cespedes EI. Scattering properties of encapsulated gas bubbles at high ultrasound pressures. J Acoust Soc Am. 1999. 105:1989–1996.

8. Shohet RV, Chen S, Zhou YT, Wang Z, Meidell RS, Grayburn PA, et al. Echocardiographic destruction of albumin microbubbles directs gene delivery to the myocardium. Circulation. 2000. 101(22):2554–2556.

9. Wei K, Jayaweera AR, Firoozan S, Linka A, Skyba DM, Kaul S. Quantification of myocardial blood flow with ultrasound-induced destruction of microbubbles administered as a constant venous infusion. Circulation. 1998. 97(5):473–483.

10. Simpson D, Chin C, Burns P. Pulse inversion Doppler:A new method for detecting nonlinear echoes from microbubble contrast agents. IEEE Trans Ultrason Ferr Freq Con. 1999. 46:372–382.

11. Becher H, Burns PN. Handbook of contrast echocardiography. 2000. Berlin: Springer.
13. Porter TR, Xie F. Visually discernible myocardial echocardiographic contrast after intravenous injection of sonicated dextrose albumin microbubbles containing high molecular weight, less soluble gases. J Am Coll Cardiol. 1995. 25:509–515.

15. Hagler DJ, Currie PJ, Seward JB, Tajik AJ, Mair DD, Ritter DG. Echocardiographic contrast enhancement of poor or weak continuous wave Doppler signals. Echocardiography. 1987. 4:63–67.

16. Crouse LJ, Cheirif J, Hanly DE, Kisslo JA, Labovitz AJ, Smith MD, et al. Opacification and border delineation improvement in patients with suboptimal endocardial border definition in routine echocardiography : results of the Phase III Albunex Multicenter Trial. J Am Coll Cardiol. 1993. 22(5):1494–1500.

17. Schroder K, Agrawal R, Voller H, Schlief R, Schroder R. Improvement of endocardial border delineation in suboptimal stress-echocardiograms using the new left heart contrast agent SH U 508 A. Int J Card Imaging. 1994. 10:45–51.

18. Kassab GS, Lin DH, Fung YC. Morphometry of pig coronary venous system. Am J Physiol. 1994. 267(6 Pt 2):H2100–H2113.

19. Kassab GS, Rider CA, Tang NJ, Fung YC. Morphometry of pig coronary arterial trees. Am J Physiol. 1993. 265(1 Pt 2):H350–H365.

20. Kassab GS, Fung YC. Topology and dimensions of pig coronary capillary network. Am J Physiol. 1994. 267(1 Pt 2):H319–H325.

21. Gould KL, Lipscomb K. Effects of coronary stenoses on coronary flow reserve and resistance. Am J Cardiol. 1974. 34(1):48–55.

22. Wu X, Ewert DL, Liu Y, Rittman EL. In vivo relation of intramyocardial blood volume to myocardial perfusion:evidence supporting microvascular site for autoregulation. Circulation. 1992. 85:730–737.

23. Keller MW, Segal SS, Kaul S, Duling B. The behavior of sonicated albumin microbubbles within the microcirculation:a basis for their use during myocardial contrast echocardiography. Circ Res. 1989. 65(2):458–467.

24. Skyba DM, Camarano G, Goodman NC, Price RJ, Skalak TC, Kaul S. Hemodynamic characteristics, myocardial kinetics and microvascular rheology of FS-069, a second-generation echocardiographic contrast agent capable of producing myocardial opacification from a venous injection. J Am Coll Cardiol. 1996. 28(5):1292–1300.

25. Lindner JR, Song J, Jayaweera AR, Sklenar J, Kaul S. Microvascular rheology of Definity microbubbles after intra-arterial and intravenous administration. J Am Soc Echocardiogr. 2002. 15(5):396–403.

26. Jayaweera AR, Edwards N, Glasheen WP, Villanueva FS, Abbott RD, Kaul S. In vivo myocardial kinetics of air-filled albumin microbubbles during myocardial contrast echocardiography. Comparison with radiolabeled red blood cells. Circ Res. 1994. 74(6):1157–1165.

27. Kemper AJ, O'Boyle JE, Cohen CA, Taylor A, Parisi AF. Hydrogen peroxide contrast echocardiography : quantification in vivo of myocardial risk area during coronary occlusion and the necrotic area remaining after myocardial reperfusion. Circulation. 1984. 70:309–317.

28. Villanueva FS, Glasheen WP, Sklenar J, Kaul S. Assessment of risk area during coronary occlusion and infarct size after reperfusion with myocardial contrast echocardiography using left and right atrial injections of contrast. Circulation. 1993. 88:596–604.

29. Firschke C, Camarano G, Lindner JR, Wei K, Goodman NC, Kaul S. Myocardial perfusion imaging in the setting of coronary artery stenosis and acute myocardial infarction using venous injection of FS-069, a second-generation echocardiographic contrast agent. Circulation. 1997. 96:959–967.
30. Ragosta M, Camarano GP, Kaul S, Powers E, Sarembock IJ, Gimple LW. Microvascular integrity indicates myocellular viability in patients with recent myocardial infarction:new insights using myocardial contrast echocardiography. Circulation. 1994. 89:2562–2569.

31. Ito H, Tomooka T, Sakai N, Yu H, Higashino Y, Minamino T, et al. Lack of myocardial perfusion immediately after successful thrombolysis:a predictor of poor recovery of left ventricular function in anterior myocardial infarction. Circulation. 1992. 85:1699–1705.

32. Ito H, Tomooka T, Sakai N, Yu H, Higashino Y, Minamino T, et al. Lack of myocardial perfusion immediately after successful thrombolysis. A predictor of poor recovery of left ventricular function in anterior myocardial infarction. Circulation. 1992. 85(5):1699–1705.

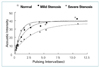
33. Lindner JR, Skyba DM, Goodman NC, Jayaweera AR, Kaul S. Changes in myocardial blood volume with graded coronary stenosis : an experimental evaluation using myocardial contrast echocardiography. Am J Physiol. 1997. 272:H567–H575.
34. Kaul S, Senior R, Dittrich H, Raval U, Khattar R, Lahiri A. Detection of coronary artery disease using myocardial contrast echocardiography : comparison with 99mTc-sestamibi single photon emission computed tomography. Circulation. 1997. 96:785–792.

35. Lindner JR, Skyba DM, Goodman NC, Jayaweera AR, Kaul S. Changes in myocardial blood volume with graded coronary stenosis : an experimental evaluation using myocardial contrast echocardiography. Am J Physiol. 1997. 272:H567–H575.
36. Lindner JR, Dayton PA, Coggins MP, Ley K, Song J, Kaul S, et al. Noninvasive imaging of inflammation by ultrasound detection of phagocytosed microbubbles. Circulation. 2000. 102:531–538.

37. Lindner JR, Song J, Xu F, Klibanov AL, Singbartl K, Kaul S, et al. Noninvasive ultrasound imaging of inflammation using microbubbles targeted to activated leukocytes. Circulation. 2000. 102:2745–2750.

38. Skyba DM, Price RJ, Linka AZ, Skalak TC, Kaul S. Direct in vivo visualization of intravascular destruction of microbubbles by ultrasound and its local effects on tissue. Circulation. 1998. 98:290–293.

39. Price RJ, Skyba DM, Kaul S, Skalak TC. Delivery of colloidal particles and red blood cells to tissue through microvessel ruptures created by targeted microbubble destruction with ultrasound. Circulation. 1998. 98:1264–1267.

40. Mukherjee D, Wong J, Griffin B, Ellis SG, Porter T, Thomas JD, et al. Ten-fold augmentation of endothelial uptake of vascular endothelial growth factor with ultrasound after systemic administration. J Am Coll Cardiol. 2000. 35:1678–1686.

41. Shohet RV, Chen S, Zhou YT, Wang Z, Meidell RS, Grayburn PA, et al. Echocardiographic destruction of albumin microbubbles directs gene delivery to the myocardium. Circulation. 2000. 101:2554–2556.

42. Birnbaum Y, Luo H, Nagai T, Fishbein MC, Peterson TM, Siegel RJ, et al. Noninvasive in vivo clot dissolution without a thrombolytic drug:recanalization of thrombosed iliofemoral arteries by transcutaneous ultrasound combined with intravenous infusion of microbubbles. Circulation. 1998. 97:130–134.





 PDF
PDF ePub
ePub Citation
Citation Print
Print















 XML Download
XML Download