See the article "".
To the editor: We read with great interest the article entitled 'Cost-effectiveness of para-aortic lymphadenectomy before chemoradiotherapy in locally advanced cervical cancer' [1]. The authors used a modified Markov model which utilised estimates extrapolated from other published series and came to the conclusion that such staging would be cost effective in patients when positron emission tomography/computed tomography (PET/CT) imaging shows no evidence of para-aortic lymph node (PALN) metastasis.
The incidence PALN metastasis varies from 5% in the International Federation of Gynecology and Obstetrics (FIGO) stage I cervix cancer patients to 38% in stage III in various surgically and PET staging studies [2]. Table 1 taken from a review article [2] shows the prevalence of para-aortic nodal metastases according to FIGO stage from published literature [3456].
Even if the authors are right in their assumption that PALN surgical staging is 100% sensitive and specific in the cohort of patients who have <5 mm sized lymph node at the time of surgery, surely not all patients, regardless of their probability of harbouring microscopic PALN will benefit from surgical staging?
In general, the different methods of staging, be it pretherapeutic surgical PALN staging (n=184) [4], pretherapeutic PET staging (n=206) [7], or post-chemo radiotherapy pelvic and PALN dissection (n=73) [8] result in similar survival.
Here in Melbourne, Australia, we have extensively utilised both laparoscopic as well as PET staging in cervix cancer. Five hundred thirty-six locally advanced cervix cancer patients (squamous cell carcinoma or adenocarcinoma histology) were treated with curative intent using radiotherapy at Peter MacCallum Cancer Centre between 1996 and 2010. Based on initial assessment, 38 of these patients were planned for surgical evaluation of nodes followed by radical hysterectomy. Since positive nodes were found on frozen section, hysterectomy was abandoned and definitive radiotherapy was given. Seventeen out of these 38 patients (44%) have relapsed. On the other hand, 69 patients had both PET and laparoscopic staging, and of these 27 (39%) have failed. Three hundred twenty patients were staged with PET only, of these 36% have failed and 109 patients had neither PET nor laparoscopic staging, of these 34 (31%) have relapsed.
Ninety-seven of the 536 patients (18%) had PALN metastasis detected by either PET alone (n=67; of these 38 [56%] have relapsed), surgical staging alone (n=9; of these seven patients [77%] have relapsed) or both PET & laparoscopic staging (n=21; and of these 14 [66%] have relapsed). We would like to highlight that in the group that had a PET followed by laparoscopic staging, only three out of 21patients had a false negative PET where laparoscopic surgery recovered metastatic node(s) in the para-aortic region. Of these three patients, one has relapsed.
As this study has shown that it is difficult to identify a suitable patient group who would benefit from surgical staging in addition to a PET/PET-CT staging, we have since abandoned the routine practice of pretherapeutic laparoscopic staging.
It would indeed be useful if authors of this paper could describe precisely how would they select patients for PALN staging from a cohort of locally advanced cervix cancer patients, where PET/CT have not shown any metastatic node in para-aortic region.
Figures and Tables
Table 1
Prevalence of para-aortic nodal metastasis in locally advanced cervical cancer according to the FIGO stage
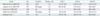
| Study | No. | Patients | Nodes+ (%) | FIGO I | FIGO II | FIGO III |
|---|---|---|---|---|---|---|
| Berman et al. (1984) [3]* | 621 | >IB1 | 16 | 5% of 150 | 16% of 222 | 25% of 135 |
| Leblanc et al. (2007) [4]* | 181 | All stages | 24 | 20% of 58 | 17% of 52 | 32% of 65 |
| Fine et al. (1995) [5]* | 189 | ≥II | 30 | - | 24% of 89 | 38% of 85 |
| Kidd et al. (2010) [6]† | 560 | All stages | 34 | 5% of 227 | 17% of 104 | 33% of 115 |
| Narayan et al.†,‡ | 410 | <IV | 47 | 14% of 149 | 20% of 179 | 32% of 82 |
References
1. Lee JY, Kim Y, Lee TJ, Jeon YW, Kim K, Chung HH, et al. Cost-effectiveness of para-aortic lymphadenectomy before chemoradiotherapy in locally advanced cervical cancer. J Gynecol Oncol. 2015; 26:171–178.
2. Narayan K, Lin MY. Staging for cervix cancer: role of radiology, surgery and clinical assessment. Best Pract Res Clin Obstet Gynaecol. 2015; 29:833–844.
3. Berman ML, Keys H, Creasman W, DiSaia P, Bundy B, Blessing J. Survival and patterns of recurrence in cervical cancer metastatic to periaortic lymph nodes (a Gynecologic Oncology Group study). Gynecol Oncol. 1984; 19:8–16.
4. Leblanc E, Narducci F, Frumovitz M, Lesoin A, Castelain B, Baranzelli MC, et al. Therapeutic value of pretherapeutic extraperitoneal laparoscopic staging of locally advanced cervical carcinoma. Gynecol Oncol. 2007; 105:304–311.
5. Fine BA, Hempling RE, Piver MS, Baker TR, McAuley M, Driscoll D. Severe radiation morbidity in carcinoma of the cervix: impact of pretherapy surgical staging and previous surgery. Int J Radiat Oncol Biol Phys. 1995; 31:717–723.
6. Kidd EA, Siegel BA, Dehdashti F, Grigsby PW. Pelvic lymph node F-18 fluorodeoxyglucose uptake as a prognostic biomarker in newly diagnosed patients with locally advanced cervical cancer. Cancer. 2010; 116:1469–1475.
7. Narayan K, Fisher RJ, Bernshaw D, Shakher R, Hicks RJ. Patterns of failure and prognostic factor analyses in locally advanced cervical cancer patients staged by positron emission tomography and treated with curative intent. Int J Gynecol Cancer. 2009; 19:912–918.
8. Delpech Y, Haie-Meder C, Rey A, Zafrani Y, Uzan C, Gouy S, et al. Para-aortic involvement and interest of para-aortic lymphadenectomy after chemoradiation therapy in patients with stage IB2 and II cervical carcinoma radiologically confined to the pelvic cavity. Ann Surg Oncol. 2007; 14:3223–3231.
We would like to thank Dr. Lin and their colleagues for interest and comments regarding 'Cost-effectiveness of paraaortic lymphadenectomy before chemoradiotherapy in locally advanced cervical cancer'.
The purpose of the present study was to evaluate the cost-effectiveness of nodal staging surgery before chemoradiotherapy for locally advanced cervical cancer in the era of positron emission tomography/computed tomography (PET/CT) [1]. As you mentioned, the survival benefit of surgical staging has not yet been determined. A major limitation of our study is the lack of survival data for unstaged para-aortic lymph node metastasis as no prospective trial has been performed that compares the outcomes of nodal staging followed by tailored chemoradiotherapy and pelvic chemoradiotherapy without surgical staging in the era of PET/CT. Although no randomized trials evaluate the role of surgical staging in the era of PET/CT, prospective studies suggest that nodal staging surgery followed by extended-field chemoradiotherapy provides survival gains for patients with para-aortic lymph node metastasis measuring 5 mm or less metastasis that would probably be missed by PET/CT [2]. Our cost-effectiveness analysis is based on the 30% improvement of survival in this subgroup.
To a certain extent, I agree with your institution's policy that routine surgical staging should be abandoned in locally advanced cervical cancer. Based on the cost-effectiveness analysis, we suggest that nodal staging surgery before definite chemoradiotherapy may be useful when PET/CT imaging shows no evidence of para-aortic lymph node metastasis. The study population in this model are patients with stage IIB or higher disease that was scheduled to undergo chemoradiotherapy when no uptake was recorded in paraaortic lymph node no PET/CT. The overall false-negative rate of para-aortic lymph node involvement is around 12%, most of which is attributable to non-detectable nodal disease [3]. We did not consider surgical staging when uptake is noted in the para-aortic area on PET/CT due to its high true-positive rate. In our model, nodal staging surgery followed by tailored chemoradiotherapy is cost-effective for a wide range of false-negative rates (5% to 17%) of PET/CT detecting para-aortic lymph node metastasis. From your institution's data, three out of 21 patients (14.2%) had a false negative PET where laparoscopic surgery recovered metastatic node in the paraaortic regions. False negative rate from your institution (14.2%) lies within the limit of our sensitivity analysis (5% to 17%).
A recent Cochrane Review summarized non-randomized controlled trial published data and suggests that surgical staging is more accurate than available imaging modalities with proven safety, and complete debulking of involved para-aortic nodes appears to translate into a survival advantage [4]. They suggested that the decision to offer pretreatment surgical para-aortic lymph node assessment needs to be individualized. In this study, we suggested a possible candidate who can have benefit from surgical staging. Based on the best evidence available, we insist that nodal staging surgery should be considered in all patients who have no uptake in para-aortic lymph nodes from PET/CT.
References
1. Lee JY, Kim Y, Lee TJ, Jeon YW, Kim K, Chung HH, et al. Cost-effectiveness of para-aortic lymphadenectomy before chemoradiotherapy in locally advanced cervical cancer. J Gynecol Oncol. 2015; 26:171–178.
2. Leblanc E, Narducci F, Frumovitz M, Lesoin A, Castelain B, Baranzelli MC, et al. Therapeutic value of pretherapeutic extraperitoneal laparoscopic staging of locally advanced cervical carcinoma. Gynecol Oncol. 2007; 105:304–311.
3. Gouy S, Morice P, Narducci F, Uzan C, Gilmore J, Kolesnikov-Gauthier H, et al. Nodal-staging surgery for locally advanced cervical cancer in the era of PET. Lancet Oncol. 2012; 13:e212–e220.
4. Brockbank E, Kokka F, Bryant A, Pomel C, Reynolds K. Pre-treatment surgical para-aortic lymph node assessment in locally advanced cervical cancer. Cochrane Database Syst Rev. 2013; 3:CD008217.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download